Introduction
Endotracheal tube (ETT) cuffs are traditionally inflated with 10cc of air after insertion into the trachea to provide adequate seal against the tracheal lumen and to subsequently create closed-system positive pressure ventilation. Under-inflated cuffs may result in micro-aspiration passing around the cuffs, potentially increasing the risks of aspiration pneumonia as well as ventilator-associated pneumonia. Reference Pitts, Fisher, Sulemanji, Kratohvil, Jiang and Kacmarek1,Reference Bernhard, Cottrell, Sivakumaran, Patel, Yost and Turndorf2 Existing literature suggests that a minimum pressure of 20cmH2O is recommended to prevent aspiration and ventilator-associated pneumonia. 3 Achieving and maintaining a cuff pressure of 20-30cmH2O has been established as the standard of care.
However, although it is important to adequately inflate ETT cuffs, it is also dangerous to over-inflate them. There are several studies that suggest in practice, ETT cuffs are often inflated well beyond the accepted safe pressure range of 20-30cmH2O.3-Reference Sengupta, Sessler and Maglinger7 Elevated cuff pressures can be detrimental to patient outcomes because the excess pressure is transferred directly to the mucosal surface of the tracheal lumen. Current literature suggests ETT cuff pressures between 30-50cmH2O are associated with impaired tracheal capillary perfusion.Reference Benumof and Cooper8 When the pressure of the ETT cuff against the mucosa is equal to or greater than the perfusion pressure of the local capillary vessels, effectively occluding blood flow and impairing perfusion, complications including tissue ischemia, necrosis, scarring, and stenosis of the tracheal wall may develop.Reference Benumof and Cooper8-Reference Lim, Kim and Kim11 This can lead to serious complications including tracheal ulcer, tracheal rupture, and tracheoesophageal fistula.Reference Rubio, Farrell and Bautista9-Reference Hameed, Mohamed and Al-Mansoori12 In addition, there are also several animal studies that describe a similar effect and relationship between elevated ETT cuff pressure and capillary blood flow to tracheal lumen.Reference Bunegin, Albin and Smith13,Reference Nordin, Lindholm and Wolgast14
Despite it being considered a component in the standard of care in ETT management and prior studies supporting the use of cuff pressure recording in various clinical settings, ETT cuff pressures are not routinely recorded in prehospital patient care records or in hospital medical records.Reference Curiel García, Guerrero-Romero and Rodríguez-Morán15-Reference Galinski, Tréoux, Garrigue, Lapostolle, Borron and Adnet19 Furthermore, few studies address the ETT cuff pressure after prehospital intubation. This study aims to gain insight about the average ETT cuff pressures in patients who are intubated by Emergency Medical Services (EMS) and seeks to provide evidence supporting the adoption and integration of cuff pressure recording as a part of future prehospital care, as well as Respiratory Therapy (RT) protocols when receiving patients at the emergency department (ED). It was hypothesized that the average ETT cuff pressure after prehospital intubation exceeds the recommended 20-30cmH2O.
Methods
Settings and Participants
This study took place at a large, urban, tertiary care center ED. Patients were identified as prospective subjects in the trauma bay, resuscitation rooms, and standard patient care rooms. Informed consent was waived due to the minimal risk and observational nature of the intervention. In the region where this study was completed, only Advanced Life Support (paramedic) level prehospital providers perform intubations, and most intubations are medication-assisted intubations (MAIs).
Inclusion and Exclusion Criteria
The study included adult patients aged 18 or older who were intubated with a cuffed ETT by an EMS provider prior to arrival at the ED. Pediatric patients, patients who arrived with misplaced ETTs and/or ETTs that required manipulation before cuff pressure measurement, and patients who were intubated with an un-cuffed ETT were excluded. Patients who were intubated at an outside facility prior to transfer were also excluded.
Procedure
The study period ran from December 1, 2019 through August 1, 2020. Upon arrival at the study site ED, patients who were intubated by prehospital providers had their ETT cuff pressures measured by the RT team receiving the patient. All measurements were performed by respiratory therapists utilizing the AG Cuffill device (AG Cuffill; Mercury Medical; Florida USA) which had a detectable range of 0-100cmH2O, and any cuff pressures documented as “OP” (over 100cmH2O) were entered into database as 100cmH2O. The device was used in its Food and Drug Administration (FDA; Silver Spring, Maryland USA) approved manner. The RT team had been instructed on study inclusion/exclusion criteria by a member of the study team prior to initiation of data collection. Per the RT team’s own departmental protocol, respiratory therapists adjusted ETT cuff pressure to fall within the goal 20-30cm H2O in accordance with the standard of care if the cuff pressure was found to be inappropriate. The RT team recorded the initial cuff pressure, tube size, and EMS provider on a prefabricated patient enrollment card. Demographic data including age, height, weight, and indication for intubation were extracted from the patient’s chart. Data were uploaded into the institution’s REDCap system version 9.9.0 (Vanderbilt University; Nashville, Tennessee USA). Reference Harris, Taylor, Thielke, Payne, Gonzalez and Conde20,Reference Harris, Taylor and Minor21 Further statistical analysis was performed using Microsoft Excel spreadsheet Version 15.27 (Microsoft Corporation; Redmond, Washington USA). The institutional review board at the University of Massachusetts Medical School (Worcester, Massachusetts USA) approved this study (IRB docket number H00017608).
Analysis
An a priori power analysis was conducted. The standard deviation of the ETT cuff pressure measurements was predicted based on prior studies and it was determined that a minimum sample size of at least 44 patients was required to detect a statistically significant 15cmH2O difference in cuff pressure with 80% power and an alpha of 0.05.
Descriptive statistics were used to analyze and report the cuff pressures obtained during this study. Linear regressions were performed to describe any correlation between age and ETT cuff pressure as well as ETT size and ETT cuff pressure. A Two-tailed T test was used to detect any difference in the means between male and female groups.
The data collected were controlled for quality by ensuring the users of the AG Cuffill device had all had the same standardized training and the study team monitored operators to ensure it was used appropriately in practice.
Results
Descriptive Statistics
The study collected 45 cuff pressure measurements from six EMS services. One out of the 45 data points was missing patient demographics. The value of 100cmH2O was utilized for any cuff pressures documented to be “OP,” indicating that the cuff was over the pressure readable by the device. The ETT sizes in this study ranged from 6.5 to 8.0mm. Mean patient age was 52.2 years (67.7% male; Table 1). The mean cuff pressure was 81.8cmH2O (range of 15 to 100). Both the median and the mode cuff pressures were 100cmH2O. In total, 40 out of the 45 (88.9%) documented cuff pressures were above 30cmH2O and two out of the 45 (4.4%) cuff pressures were below 20cmH2O. Finally, three out of the 45 (6.7%) cuff pressures were between 20-30cmH2O.
Table 1. Descriptive Data
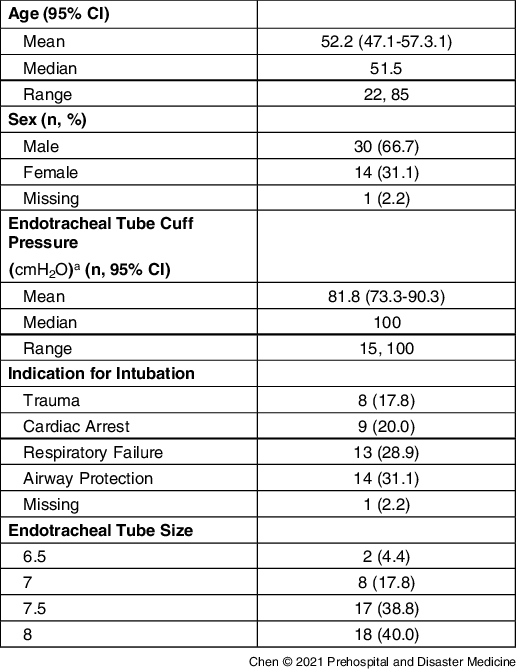
a OP was recorded as 100cmH2O for out-of-range pressures.
Correlations
Linear regression did not show any correlation between age and ETT cuff pressure (multiple R = 0.18). Linear regression also did not show any correlation between ETT size and ETT cuff pressure (multiple R = 0.23). A two-tailed T test did not show any statistically significant difference in the mean cuff pressure in male versus female patients (t = 1.90; P = .06).
Discussion
ETTs are Over-Inflated in the Prehospital Setting
In this study, ETT cuff pressures were consistently over-inflated to levels that could result in clinically significant complications. From the samples collected, there does not appear to be any correlation between ETT cuff pressure and patient demographics or ETT size. Given the lack of significant existing literature on this topic, it is likely that there isn’t enough awareness and education pertaining to ETT cuff pressures in EMS training, which may lead to overall elevation in cuff pressures in intubations performed in the prehospital setting.
Potential Causes for ETT Cuff Over-Inflation in Prehospital Intubation
Currently, few studies directly address the root causes in ETT cuff over-inflation in the prehospital setting. Currently, EMS providers performing prehospital endotracheal intubation face many challenges that impact obscured views and tactile dexterity, tube placement, and proper cuff inflation including views obstructed by bodily fluids, obesity, patient positioning, and facial/spine trauma. Additionally, one could postulate that EMS providers tend to over-inflate in order to avoid sliding of the cuff, which may lead to tube dislodgement and a need to re-intubate during high-risk transport times. Re-intubation during transport can be very difficult and may delay transport time. Furthermore, EMS providers must work quickly, often in poor lighting and suboptimal settings, and may not carry confirmatory tools (as the one used in this study) therefore limiting their ability to ensure a proper cuff pressure. Ultimately, there is a lack of literature addressing why prehospital intubations are associated with elevated cuff pressures. Future studies may lead to more insights on this topic.
Summary and Further Research
Despite being considered the standard of care in ETT management, ETT cuff pressures are not routinely recorded in prehospital or ED medical records. Prior to the initiation of this study, prehospital ETT cuff pressures were not routinely measured as patients arrive at the hospital and over-inflated cuffs likely went unnoticed for long periods of time. Based on the data collected in this study, the authors concluded that the average ETT cuff pressures in patients that arrive at the study site ED who were intubated by EMS providers were above the accepted 20-30cmH2O, confirming the initial hypothesis, and this is consistent with other current literature on this topic. Reference Tennyson, Ford-Webb, Weisberg and LeBlanc6,Reference Galinski, Tréoux, Garrigue, Lapostolle, Borron and Adnet19 This could present a patient safety concern, as elevated cuff pressures have been associated with adverse patient outcomes including tracheal stenosis, tracheal ulcer, tracheal rupture, and tracheoesophageal fistula. Reference Rubio, Farrell and Bautista9-Reference Hameed, Mohamed and Al-Mansoori12
This study has provided evidence that supports the adoption and integration of cuff pressure recording both for prehospital services and as a part of respiratory protocol for teams receiving intubated patients from the prehospital setting. Further study may entail training EMS providers on taking ETT cuff pressure measurements to shift the task of cuff pressure quality assurance to the field. Additional studies might focus on the reproducibility of standardized cuff pressures when a measuring tool becomes part of prehospital providers’ protocol after intubation as well as their ability to obtain and retain the skill of ETT cuff measurement. Finally, the authors plan to perform future studies on examining whether maintaining appropriate ETT cuff pressure in the field impacts subsequent patient outcomes.
Limitations
This study had several limitations. Given the volume and the acuity of the study site ED, in a setting where RT teams are receiving multiple intubated patients at once, it was difficult to ensure that all eligible patients had their cuff pressures checked. In addition, this study began just prior to the 2019 COVID-19 pandemic and all study activities halted for the duration of the surge in COVID-19 cases in Massachusetts in order to focus resources on alleviating the impact of the pandemic. Any potential data points from the declaration of state emergency (March 15, 2020) until the resumption of data collection (May 15, 2020) were not documented or collected. Data collected in this study does not reflect true consecutive samples secondary to effects of the COVID-19 pandemic.
Because this was a single site study, it is unknown whether the findings of this study will duplicate or reflect those at other regions in the US, especially given that EMS providers at the study site perform MAI and other regions of the US may have different prehospital intubation protocols.
Data collection for this study was done between the months of January through August 2020. Pathologies that may ultimately lead to intubations by EMS may differ depending on the different seasons of the year. It is possible that the ambient temperature had an impact on results.
Conclusion
Prehospital intubations are associated with elevated ETT cuff pressures, which can lead to long-term complications. Future study should center around providing EMS personnel with additional training on cuff pressure measurement.
Conflicts of interest/funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The manufacturer of the endotracheal tube cuff pressure-measuring device provided the devices used to perform the study free of charge. No payment was made for time or direct support of the research and the manufacturer has no right of control of data. The authors have no conflicts of interest to report.




