Introduction
Each year in the United States, approximately 300,000 people experience out-of-hospital cardiac arrest (OHCA) with only 9.6% surviving to discharge from the hospital. Reference McNally, Robb and Mehta1 Early cardiopulmonary resuscitation (CPR) and defibrillation remain key practice for improving OHCA survival. Reference Sasson, Rogers, Dahl and Kellermann2,Reference Abrams, McNally, Ong, Moyer and Dyer3 The rate of survival to discharge for OHCA was found to decrease by 2.3% with every minute of delay in performing CPR. Reference Larsen, Eisenberg, Cummins and Hallstrom4 These findings underscore the harm in delayed CPR, while reinforcing the American Heart Association (AHA; Dallas, Texas USA) recommendations of limiting pauses in chest compressions to ten seconds for pulse checks during resuscitation. Reference Panchal, Bartos and Cabanas5
Manual carotid pulse assessment is unreliable in the evaluation of cardiac activity and may delay CPR. In a study of 206 responders performing manual carotid pulse assessments on coronary artery bypass graft patients during spontaneous circulation versus non-pulsatile cardiopulmonary bypass, an absent pulse went unrecognized in ten percent of patients, while a present pulse was unrecognized in 45% of patients. Reference Eberle, Dick, Schneider, Wisser, Doetsch and Tzanova6 In another study, only two percent of first responders could recognize pulselessness within ten seconds. Reference Dick, Eberle, Wisser and Schneider7 Prolonged pulse assessments delay the resumption of chest compressions and could potentially decrease survival rates. Conversely, false identification of an absent pulse may result in unnecessary CPR and additional doses of resuscitative medications, including adrenaline, which has been associated with poor neurological outcomes with repeated doses. Reference Fukuda, Ohashi-Fukuda, Matsubara, Gunshin, Kondo and Yahagi8
Research has shown point-of-care ultrasound (POCUS) is a useful tool in mitigating inaccurate manual pulse assessments and managing patient care. Reference Breitkreutz, Price and Steiger9,10 Carotid and femoral compressibility, considered a “POCUS pulse-check,” and cardiac contractility on ultrasound (US) imaging can aid in discerning the presence of cardiac activity when the physical exam is equivocal. A case series using POCUS to assess for carotid and femoral compressibility found the POCUS pulse checks to be consistently performed in less than five seconds. Reference Simard, Unger, Betz, Wu and Chenkin11 One randomized controlled trial found that POCUS had a greater first attempt success rate (99.1% versus 85.6%) with faster mean detection times (4.22s versus 4.71s) for identifying pulses when compared with manual detection. Reference Badra, Coutin, Simard, Pinto, Lee and Chenkin12 Additionally, a multi-center study found that of 793 patients thought to be in pulseless electrical activity (PEA) rhythms, 54.3% had cardiac activity without palpable pulses, which were only discernable with US. Reference Gaspari, Weekes and Adhikari13 The detection of cardiac activity with US facilitated more appropriate management of these patients.
Although US has demonstrated utility in cardiac arrest, POCUS has not been integrated into most Emergency Medical Service (EMS) systems. Reference Taylor, McLaughlin, McRae, Lang and Anton14 A survey of American and Canadian physicians found that only 4.1% of EMS systems are using POCUS. Some studies have shown European and American EMS physicians demonstrating POCUS efficacy in prehospital care. Reference Breitkreutz, Price and Steiger9,Reference Taylor, McLaughlin, McRae, Lang and Anton14–Reference Ketelaars, Beekers, Van Geffen, Scheffer and Hoogerwerf17 Two studies have demonstrated that EMS technicians are able to interpret POCUS images, including assessing for cardiac contractility. Reference Chin, Chan and Mortazavi18,Reference Bhat, Johnson, Pierog, Zaia, Williams and Gharahbaghian19 Small studies expanded on this POCUS use to demonstrate that non-physician first responders were able to obtain US images in a prehospital setting. Reference Reed, Gibson, Dewar, Short, Black and Clegg20,Reference Rooney, Lahham and Lahham21
Utility of POCUS in medical OHCA was assessed in a prospective, observational cohort study. The primary outcome was the percentage of adequate POCUS video acquisition and accurate video interpretation during OHCA by paramedics. Secondary outcomes included POCUS-driven treatment changes, interventions, medications administered including adrenaline, clinical outcomes, and paramedic adherence to resuscitation protocol including end-tidal carbon dioxide (EtCO2) monitoring after placement of an advanced airway (endotracheal tube or i-gel) and compression pauses under ten seconds.
Methods
A waiver from the State of Colorado (USA) was granted to South Metro Fire Rescue (SMFR; Centennial, Colorado USA) to train their paramedics to use POCUS to assess for cardiac contractility during a medical cardiac arrest. Currently, SMFR is an organization with approximately 175 practicing paramedics with 29 stations that serves 300 square miles with approximately 540,000 residents. Paramedics (n = 40), who were recruited on a voluntary basis via email, participated in a four-hour training session which included a didactic lecture and hands-on POCUS instruction from POCUS experts (emergency US fellowship-trained physicians). Training included assessment for cardiac contractility, pericardial effusion, and pneumothorax. Each paramedic performed at least 25 cardiac POCUS exams on live models which were reviewed by a POCUS expert prior to deployment of POCUS in the field.
An EMS POCUS protocol, the Prehospital Echocardiogram in Cardiac Arrest (PECA), was developed and integrated into standard OHCA care (Figure 1). 22 Field POCUS utilization was limited to medical non-shockable arrest. Selection of cases was based on PECA protocol (Figure 1) and the State of Colorado Waiver (Supplement 1; available online only). Exclusion criteria included: patients not experiencing medical cardiac arrest; pediatric patients; patients experiencing trauma, drowning, and electrocution; patients with incomplete datasets; and patients evaluated by paramedics without POCUS-credentialing. Standard OHCA treatment included high-quality CPR, early defibrillation, airway management, and three doses of adrenaline. The PECA protocol emphasized that POCUS use should not delay initial resuscitation efforts nor prolong compression pauses beyond ten seconds. The paramedic performing chest compressions counted to ten audibly during the pulse check and resumed compressions at ten seconds, instructing the paramedic capturing the US video to stop scanning. The POCUS-credentialed paramedics were only responsible for performing the US during the resuscitation.
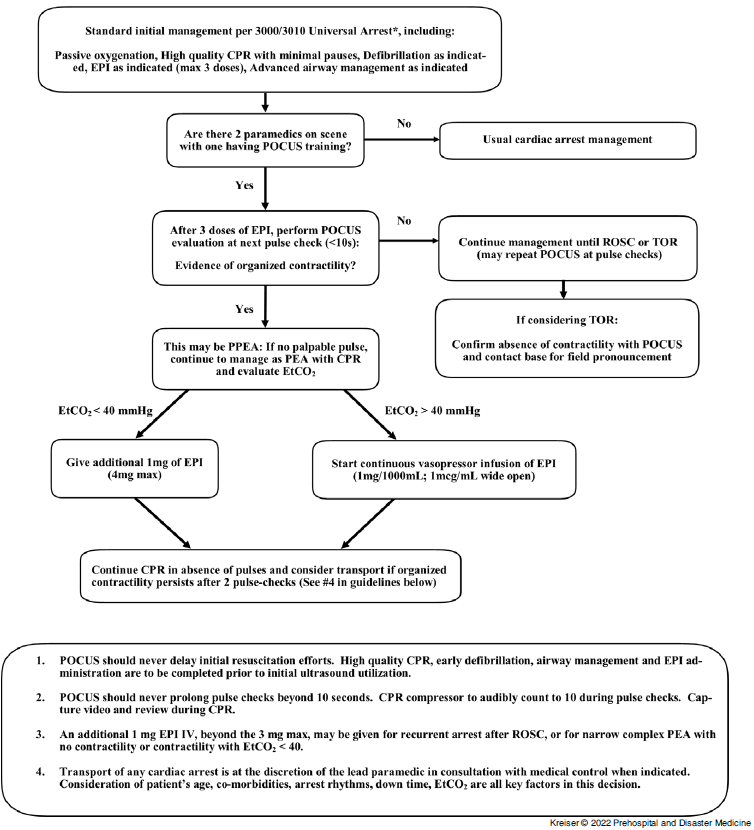
Figure 1. Prehospital Echocardiogram in Cardiac Arrest (PECA) Protocol.
Abbreviations: POCUS, point-of-care ultrasound; ROSC, return of spontaneous circulation; TOR, termination of resuscitation; PEA, pulseless electrical activity; PPEA, pseudo-pulseless electrical activity; CPR, cardiopulmonary resuscitation; EtCO2, end-tidal carbon dioxide; IV, intravenous; EPI, adrenaline.
*3000 is the Denver Metropolitan Prehospital Protocol (DMPP) for medical pulseless arrest to include shockable ventricular tachycardia/ventricular fibrillation and rhythm of asystole/PEA. 3010 is the DMPP which defines parameters for compression factors, defibrillation execution, ventilation recommendations, airway management, and ROSC defined. Pacing circumstance and flow are also addressed.Reference Reed, Gibson, Dewar, Short, Black and Clegg20
A hand-held US (Butterfly IQ Hand-Held US; Butterfly Network; Guilford, Connecticut USA) was used to acquire video images. The videos were stored in the Butterfly Network cloud, which is Health Insurance Portability and Accountability Act (HIPAA) and Health Information Technology for Economic and Clinical Health (HITECH) Act compliant with System and Organizations II (SOC II) certification. 23 The paramedics recorded their impression of the video US images in the digital cloud and their electronic health record (EHR). The US videos were reviewed by a single POCUS expert investigator (AT) to determine adequacy of image quality and the accuracy of the interpretation. The POCUS expert was aware of the initial clinical presentation (eg, 46-year-old man without vital signs), as it was documented with the video in the digital cloud, but was blinded to treatments, interventions, and outcome data. Feedback was given to the medics via the digital cloud. Paramedics additionally documented if POCUS use resulted in any changes in the decision whether to transport the patient or any changes in patient treatment in the EHR. The SMFR electronic medical record was accessed for patient demographic information, interventions, medications administered including adrenaline, and protocol adherence data including EtCO2 monitoring after placement of an advanced airway (endotracheal tube or i-gel) and compression pauses under ten seconds. The regional health information exchange (Colorado Regional Health Information Exchange; Denver, Colorado USA) was accessed for clinical outcomes. Institutional Review Board approval (IRB #2020-0057) was obtained from Rocky Vista University (Parker, Colorado USA). All descriptive statistics, which include means, frequencies, and percentages, were calculated using SAS v9.4 (SAS Institute; Cary, North Carolina USA).
Results
From September 19, 2019 through May 10, 2020, 128 patients were evaluated for medical OHCA with 50 patients receiving care from a paramedic team with at least one POCUS-credentialed paramedic who used the PECA protocol. One patient was excluded for incomplete data, leaving 49 patients with POCUS video for analysis. Patient demographics are listed in Table 1.
Table 1. Patient Demographics (n = 49 patients)

The POCUS video images were considered adequate in 42/49 (85.7%) patients. Paramedics accurately interpreted the POCUS images in 43/49 (87.7%) patients. Asystole was recorded as the initial rhythm in 33/49 (67.4%) patients. Ultrasound was indicated only in patients with a non-shockable rhythm after three doses of adrenaline; however, eight patients (16.3%) who had ventricular fibrillation on their initial rhythm converted to a non-shockable rhythm, making them eligible for POCUS per the PECA protocol. The remaining eight patients (16.3%) had PEA. Also, POCUS cardiac contractility was noted and documented correctly in 12 patients (24.5%). In 14/49 (28.6%) patients, paramedics reported that POCUS changed management decisions. The POCUS results changed both the decision to transport and treatment decisions in 7/14 (50.0%) patients, changed the decision to transport in 5/14 (35.7%) patients, and changed treatment decisions in 2/14 (14.3%) patients.
Eight patients had a do-not-resuscitate order, and three patients were pronounced dead prior to resuscitation, leaving 38 patients for analysis of other secondary outcomes, interventions, and clinical outcomes. An advanced airway was placed in 36/38 (94.7%) patients, with 26/38 (68.4%) receiving endotracheal tubes and 10/38 (26.3%) receiving i-gels (Table 2). One advanced airway was not performed at the request of the medical power of attorney for the patient. An airway was not attempted on an additional patient due to tracheostomy scarring, as effective oxygenation was achieved with an oropharyngeal airway and bag-mask ventilation. Of the 36 patients receiving an advanced airway, EtCO2 monitoring adherence was achieved for 36/36 (100%) patients. Adrenaline administration adherence was achieved for 38/38 (100%) patients. Compression pauses were under ten seconds for 36/38 (94.7%) patients. Other interventions, medications administered, and outcomes are listed in Table 2.
Table 2. Interventions, Medications Administered and Outcomes (n = 38 patients)

Abbreviations: EMS, Emergency Medical Services; ROSC, return of spontaneous circulation; ED, emergency department.
Discussion
This study demonstrated that paramedics were able to obtain adequate POCUS images and interpret the images for cardiac activity in medical OHCA patients. Additionally, the PECA protocol demonstrated a higher percentage of adequate images obtained by paramedics when compared to prior literature. In one study, paramedics were able to obtain adequate cardiac images in 55% of scans after a two-hour training. Reference Chin, Chan and Mortazavi18 In another study, 68% of the first scans obtained were adequate, although the accuracy of image interpretation was not included. Reference Reed, Gibson, Dewar, Short, Black and Clegg20 One prehospital trial did demonstrate an adequate scan rate of 89% with accurate interpretation in 17/17 cases of cardiac activity (100%; 95% CI, 67%-99%) and 2/2 cases of cardiac standstill (100%; 95% CI, 22%-100%). However, pause length was not reported and only four out of 20 POCUS-trained paramedics were included. Reference Rooney, Lahham and Lahham21 The PECA protocol study was more inclusive, had a larger cohort, and demonstrated POCUS proficiency while maintaining OHCA protocol adherence. These findings suggest that with appropriate training and image review, paramedics can effectively utilize POCUS for OHCA.
A primary concern is that POCUS use in cardiac arrest will increase the duration of the pulse check to greater than ten seconds. Increases in pulse check duration by five seconds from the AHA recommended ten-second protocol have been associated with an 18% increase in mortality rate. Reference Cheskes, Schmicker and Christenson24 One prospective cohort study of 123 pulse checks in 23 OHCA patients demonstrated a mean pulse check time of 21 seconds for emergency department (ED) providers using POCUS versus 13 seconds for pulse checks without the use of POCUS. Reference Huis In’t Veld, Allison and Bostick25 A similar cohort study evaluated 110 pauses in compression and noted median pulse check times of 17 seconds for ED providers using POCUS versus 11 seconds for pulse checks without the use of POCUS. Reference Clattenburg, Wroe and Brown26 Using the PECA protocol, 94.7% of compression pauses remained under ten seconds, which was likely due to the algorithm and training. Two of the compression pauses in the study exceeded ten seconds, but only one was secondary to POCUS use and feedback was provided. Adherence to the Advanced Cardiac Life Support (ACLS) compression pause guidelines was comparable to the 90% adherence of ED physicians using POCUS in cardiac arrest. Reference Hayhurst, Lebus and Atkinson27
Generally, POCUS protocols such as the PECA protocol have been shown to improve OHCA guideline adherence and decrease compression pause duration. The Cardiac Arrest Sonography Assessment (CASA) trial found that the development of an algorithm for US use during cardiac arrest significantly reduced sonography-related CPR interruptions by 4.0 seconds. Reference Clattenburg, Wroe and Gardner28,Reference Gardner, Clattenburg, Wroe, Singh, Mantuani and Nagdev29 Optimization of the PECA protocol and additional training may help improve adherence to OHCA protocols. The current percentages of protocol adherence suggest that paramedics can implement POCUS into their resuscitation protocol and maintain standards of care for OHCA.
Use of POCUS was also found to have a substantial impact on paramedic decision making and patient management in approximately 30% of patients. Previous studies have found even higher percentages of changes in patient management, with treatment changes in 78% of patients undergoing resuscitation and treatment changes in 88% of cardiac arrest patients. Reference Breitkreutz, Price and Steiger9,Reference Ketelaars, Beekers, Van Geffen, Scheffer and Hoogerwerf17 Data were only collected on whether POCUS use impacted the decision to transport or treatment but were not collected on the specifics. Further study is required to explicitly define these treatment and transport changes and whether they impacted patient outcomes.
Prehospital POCUS may be a useful objective adjunct in termination of resuscitation (TOR) decisions. A prospective, multi-center study involving 793 patients found that cardiac activity on US had the highest association with survival following cardiac arrest. Reference Gaspari, Weekes and Adhikari13 The percentages of patients with cardiac activity achieving return of spontaneous circulation (ROSC), survival to admission, and survival to discharge were 51.0%, 28.9%, and 3.8%, respectively. These percentages were significantly higher than the percentages of patients without cardiac activity who achieved ROSC (14.3%), survival to admission (7.2%), and survival to discharge (0.6%). Cardiac activity on POCUS was more highly associated with ROSC (odds ratio [OR] = 3.6) and survival to discharge (OR = 5.7) than any other variable, including bystander CPR (OR = 1.6 for ROSC; OR = 2.6 for survival to discharge). The PECA protocol study found 21.1% of patients had ROSC in the prehospital period, which is lower than the SMFR average ROSC rate of 31.0% for patients in which CPR is initiated. This finding is likely due to study criteria that patients could only be included if ROSC was not achieved after three doses of adrenaline. A multi-center study demonstrated cardiac standstill on US had a negative predictive value of 94.0% for ROSC, while other studies have shown a negative predictive value as high as 97.5% for ROSC. Reference Hayhurst, Lebus and Atkinson27,Reference Kedan, Ciozda, Palatinus, Palatinus and Kimchi30,Reference Botker, Jacobsen, Rudolph and Knudsen31 Per paramedic feedback, the US findings provided additional information that helped the paramedic determine that TOR was the appropriate course and provided the patient’s family and friends with more objective data to support that decision. Decreasing unnecessary emergent transports could conserve EMS resources and reduce safety risks to providers and the community associated with emergent transports. Future studies can address the impact of POCUS on OHCA health care costs and safety risks.
Some studies propose a role for POCUS in improving patient outcomes through detection and intervention-guidance during cardiac arrest with treatable aetiologies. Reference Breitkreutz, Price and Steiger9,Reference Badra, Coutin, Simard, Pinto, Lee and Chenkin12,Reference Gaspari, Weekes and Adhikari13,Reference Hayhurst, Lebus and Atkinson27,Reference Kedan, Ciozda, Palatinus, Palatinus and Kimchi30,Reference Long, Alerhand, Maliel and Koyfman32,Reference O’Dochartaigh, Douma and MacKenzie33 One ED study of 50 patients undergoing POCUS for cardiac arrest found that 12% of images resulted in an intervention as a direct result of the scan, including pericardiocentesis, thrombolysis, and chest drain. Reference Hayhurst, Lebus and Atkinson27 Emergency physicians in the Focused Echocardiographic Evaluation in Life Support (FEEL) prehospital trial reported additional changes in treatment, including inotropic therapy and needle decompression of pneumothorax. Reference Breitkreutz, Price and Steiger9 A multi-center study found that cardiac arrests with POCUS-diagnosed etiologies and subsequent treatments improved survival to discharge rates. Survival was achieved in 15.4% of those receiving pericardiocentesis and 6.7% for those receiving thrombolytics. Reference Gaspari, Weekes and Adhikari13 Further research is needed to assess whether POCUS can improve patient outcomes by identifying and potentially treating life-threating conditions in the prehospital setting.
Use of POCUS may help the paramedic differentiate between pseudo-pulseless electrical activity (PPEA) and PEA, where PPEA is defined as cardiac activity detected by US without a palpable pulse. Pulseless electrical activity accounts for 35% to 40% of cardiac arrests, while PPEA may account for up to 86% of PEA cardiac arrests. Reference Mehta and Brady34,Reference Wu, Zheng and Jiang35 Also, PPEA is associated with improved outcomes compared to PEA. Reference Engdahl, Bang, Lindqvist and Herlitz36,Reference Rabjohns, Quan, Boniface and Pourmand37 In 43.4% of patients with PPEA, ROSC was achieved compared to 12.2% of patients in PEA, Reference Wu, Zheng and Jiang35 and PPEA survival to admission was 55% compared to the eight percent of PEA. Reference Breitkreutz, Price and Steiger9 In addition, patients with PPEA reached survival to hospital admission rates of 45.5% when placed on intravenous adrenergic therapy, as opposed to 37.7% of patients who received standard ACLS interventions. Reference Gaspari, Weekes and Adhikari38 Unfortunately, the PECA protocol study did not have the medics report the rhythm at the time of the POCUS so the prevalence of PPEA could not be determined in this patient population. Future prehospital studies should utilize POCUS to discern PPEA as its management differs from standard PEA resuscitation protocols and is associated with improved survival.
Limitations
Several limitations were identified with this work. The study was performed by a single organization, which may limit its external validity. Data were collected via chart review, which may be subject to inaccurate and incomplete documentation. In addition, the chart abstractors and POCUS expert were not blinded to the objective of the study. Detailed information on how POCUS changed management was not collected. The study included only 40 POCUS-credentialed paramedics and 49 patients. A small sample size was intentionally chosen for the initial assessment of paramedic accuracy and protocol adherence. The performance of the POCUS-credentialed paramedics may not be generalizable to the entire group of SMFR paramedics or to a larger patient population. However, based on these results, SMFR has continued to educate paramedics on the use of POCUS in OHCA using the PECA protocol while monitoring paramedic performance and patient outcomes.
Conclusion
Paramedics were able to accurately obtain and interpret cardiac POCUS scans during medical OHCA while adhering to a resuscitation protocol. These POCUS findings changed management in approximately 30% of patients and assisted paramedics and patients’ families when deciding upon TOR. These findings suggest that POCUS can be effectively integrated into paramedic protocols for medical OHCA.
Acknowledgements
The authors would like to thank Rocky Vista University for their donation of training space and equipment.
Conflicts of interest
The authors have no conflict of interest to disclose.
Supplementary Materials
To view supplementary material for this article, please visit https://doi.org/10.1017/S1049023X21001357






