Introduction
A key role of medical emergency services at a mass-casualty incident (MCI) is to apply a triage system that enables the systematic treatment and transport of injured casualties. Triage is a process of sorting casualties and assigning a numerical priority based on their need for first aid, resuscitation, emergency transport, and definitive care.Reference Cuttance, Dansie and Rayner 1 Considering the context of a MCI means: that triage generally occurs in an environment where there is initially a resource limitation; decisions need to be made within the complexities of a probable chaotic situation; and a balance is needed with the demands of non-medical emergency first responders (such as fire and police services). 2 The ideal triage system should make chaotic situations more manageable by providing reproducible and objective assessments of medical need that are understandable by all responders involved in MCIs.Reference Lee, McLeod and Peddle 3 - Reference Kilner 6 Moreover, the triage process should be cost-effective and easily deployed operationally, as well as being supported by appropriate educational and training methods.Reference Aitken and FitzGerald 7 - Reference Arshad, Williams and Asaeda 9
Quantifying accuracy and reproducibility of triage in the MCI setting has been problematic due to general limitations in the knowledge and application of triaging in this context.Reference Arshad, Williams and Asaeda 9 - Reference Cross and Cicero 12 The development of structured guidelines, such as the Centers for Disease Control and Prevention (CDC; Atlanta, Georgia USA) Guidelines for Field Triage of Injured Patients,Reference Challen and Walter 13 has provided some guidance on quantifiable measurement points for field triage accuracy. These guidelines promote a target under-triage accuracy rate of less than five percent and an over-triage accuracy rate of<50%. Despite these triage accuracy rates being first reported in the late 1980s, and reconfirmed in the early 1990s, they have remained principally unchallenged over the past decade.Reference Sasser, Hunt and Faul 14 , Reference Wesson and Scorpio 15
The ultimate goal of triaged-based research and an assessment of accuracy rates is to identify opportunities to improve patient outcomes, which due to the chaotic nature of a MCI, may translate simply to decreased mortality. 16 - Reference Horne, Vassallo and Read 18 When reviewing the literature available in this area, it is evident there are a range of limitations that make adopting any recommendations to MCI triage difficult to support. For instance, applying findings from multiple-patient incidents where there is adequate resourcing is problematic, as is comparing a single trauma patient against a trauma registry to draw a comparison with casualties from a MCI.Reference Mohan, Rosengart and Farris 19 Similarly, using accuracy rates determined for a single field trauma patient (as those advocated by the CDC) rather than a MCI, and applying primary triage tools as indicators of injury severity and predictors of survival, can be misleading.Reference Deluhery, Lerner and Pirrallo 10 , Reference Cross and Cicero 12 , Reference Carron, Taffe and Ribordy 17 Notwithstanding, there has been recognition that due to the uncontrolled nature of MCIs, some level of methodological limitation may, in fact, be unavoidable.Reference Lerner, Schwartz and Coule 11 , Reference Hammond 20 - Reference Culley and Effken 24
Complicating the current inability to adequately analyze triage accuracy and outcomes, due to the lack of definable measurements, is the fact that there is more than one triage methodology used for MCI triage.Reference Arshad, Williams and Asaeda 9 , Reference Cross, Petry and Cicero 25 The more commonly reported adult primary triage methodologies are SALT (Sort, Assess, Lifesaving interventions, Treatment/Transport) and START (Simple Triage and Rapid Treatment),Reference Arshad, Williams and Asaeda 9 , Reference Culley and Effken 24 supported with SAVE (Secondary Assessment of Victim Endpoint) and Triage Sieve and Sort.Reference Debacker, Hubloue and Dhondt 26 - Reference Field and Norton 28 Each of these methodologies differs in patient assessment criteria and have adaptations for pediatric casualties. The major basis for adoption of these triage methodologies appears to be jurisdictional and dependent on local practices. 2 , Reference Deluhery, Lerner and Pirrallo 10 , Reference Jenkins, McCarthy and Sauer 29
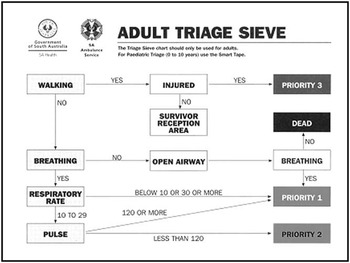
Within Australia, there appears to be some consensus towards a move to a national triage tag standard, which may result in a consistent approach to triage nation-wide.Reference Benson, Koenig and Schultz 27 Currently, however, the State of South Australia (SA) uses the Triage Sieve and Sort model of triage, as defined by Major Incident Medical Management Support (MIMMS).Reference Armstrong, Frykberg and Burris 30 The Triage Sieve (or primary triage) provides a numerical value (priority) for treatment based upon assessment of mobility (walking), respiration, and pulse. Considered as the “first look,” the Triage Sieve is not a perfect system and has been described as “crude and brutal,” but it has the benefit of being relatively easy and quick to apply.Reference Armstrong, Frykberg and Burris 30 - Reference Dethick 32 When supported by the Triage Sort (or secondary triage), the Triage Sieve and Sort model is proposed to provide accurate prioritization and efficient casualty clearance from the MCI scene; however, this is yet to be proven. An important component of the Triage Sieve and Sort model employed in SA is the inclusion of a triage sieve aide-memoir to assist the clinicians’ decision making; however, the effective use of this tool by first responders to an MCI would largely be dependent on their knowledge of where the triage pack was located in the ambulance.
Using a paper-based exercise (questionnaire), the purpose of this study was to assess operational career paramedics’ baseline ability to perform a triage sieve accurately (without any intervention/assistance) and compare this to accuracy rates following theoretical knowledge acquisition (via an educational refresher) and/or provision of an aide-memoir.
Methodology
Ethics
Ethical approval was granted by the Social and Behavioural Research Ethics Committee, Flinders University (Adelaide, Australia; SBREC 6319); SA Health (Adelaide, Australia; HREC/14/SAH/26), and SA Ambulance Service (SAAS; Eastwood, South Australia; SSA/13/SAH/47).
Data Capture
Data capture took place from March 11, 2014 through June 18, 2014 at the SAAS annual Professional Development Workshop (PDW) days, providing a sample of convenience. Data were collected from 17 PDWs. The inclusion criteria for the sample was defined as “Operational clinical staff who are either in training to become a paramedic, or have the clinical authority to practice at a paramedic level or higher, who respond either as part of an emergency ambulance crew or solo responder within SA Ambulance Service, who would undertake a triage sieve.” For the purpose of this study, the term “paramedic” is used in a generic sense in that it covers paramedic interns, paramedics, intensive care paramedics, and extended care paramedics – unless explicitly outlined.
No participants were contacted directly for recruitment. A recruitment flyer and information sheet outlining the research project was emailed to the prospective participants’ Team Leader for dissemination amongst their team.
Participants were allocated to a research sub-group (Figure 1) based on the 2014-2015 SAAS Metropolitan Training Roster. The first group of participants were allocated to Research Arm 1, Sub-group 1.1; the second group of participants was allocated to Research Arm 1, Sub-group 1.2; the third group of participants were allocated to Research Arm 2, Sub-group 2.1; while the fourth group of participants was allocated to Research Arm 2, Sub-group 2.2. This cycle continued until at least 70 participants were recruited into each research arm.

Figure 1 Study Research Arms.
On the day of data capture, the Principal Researcher gave an introduction to the study, outlined the benefits of the study to the participant, as well as any associated risks in undertaking the study.
Participants were given a data collection pack, which comprised of two separate parts. Part 1 contained: a written consent form, a demographics questionnaire, as well as a base line triage knowledge questionnaire and a non-see-through, sealable envelope. Part 2 consisted of: a second, larger, non-see-through sealable envelope containing the triage sieve questionnaire. Participants were informed not to remove the triage sieve questionnaire until instructed. Each data pack was identifiable by a unique code which participants were asked to record in case they requested to be withdrawn from the research at a later stage. No withdrawal requests were received.
Instructions were given to the participants about completing Part 1 of the data pack and all participants voluntarily signed a written consent form.
The Principal Researcher and the participant’s Team Leader were blinded to the data capture process from this point on; data capture was handed over to a Research Assistant. A time limit of 10 minutes was assigned for the completion of the first part of the data pack.
After Part 1 of the data pack was completed, the Research Assistant outlined further instructions for completing the triage sieve questionnaire for Research Arm 1 (Sub-groups 1.1 and 1.2); 10 minutes also was assigned for the completion of the triage sieve questionnaire. This was in line with Kilner.Reference Castle 5
For Research Arm 2 (Sub-groups 2.1 and 2.2) the Principal Researcher re-entered the room after Part 1 of the data pack was completed, delivered the educational refresher, and then exited the room. The triage sieve questionnaire was then completed in line with Research Arm 1.
Questionnaire
Permission was obtained from Kilner to use his paper-based triage exercise from 2002,Reference Castle 5 a questionnaire which contained 20 patients who required triaging. Using the original patient descriptors, a modified Delphi methodology was employed to map the casualty descriptions against the SMART TAG (TSG Associates; Halifax, England) Adult Triage Sieve aide-memoir to determine the appropriate casualty triage sieve priority. All casualty priorities, apart from two, were agreed upon during the first round of discussions. The two casualties requiring further discussion were casualties 18 and 20, who required a second and third round of discussions, respectively.
To align with SAAS standard terminology for a MCI, the term “patient” was swapped for “casualty.” Figure 2 shows the questionnaire including scenario, instructions, and agreed priorities.

Figure 2 Questionnaire with Agreed Priorities through Delphi Methodology.
Aide-Memoir
The aide-memoir used for Sub-groups 1.2 and 2.2 is shown in Figure 3; aide-memoirs were handed out to the participants at the appropriate time by the Research Assistant. The aide-memoir handed to the participants is a direct copy of the aide-memoir that was introduced into SAAS with the change to the new SMART triage process in 2011. Being a key component of the triage pack, the aide-memoir is applied as follows: (1) A mobility test is applied, asking can the casualty walk; if the casualty can walk and is injured, the casualty is a Priority 3; if they can walk but are uninjured, the casualty is directed to the “survivor reception area” (SRA). (2) If a casualty cannot walk and they are not breathing, the airway is opened (using simple airway maneuvers); once the airway is opened, if the casualty starts to spontaneously to breath, they are a Priority 1; if there is no spontaneous breathing, the casualty is deemed to be “dead.” (3) If a casualty is not walking and they are breathing, then the respiratory rate must be counted; for respiratory rates below 10 breaths per minute or 30 or more breaths per minute, the casualty is a Priority 1; where the respiratory rate is between 10 and 29 breaths per minute, a pulse check is undertaken. (4) A casualty with a pulse rate of 120 or more becomes a Priority 1; if the pulse rate is less than 120 beats per minute, the casualty is a Priority 2.
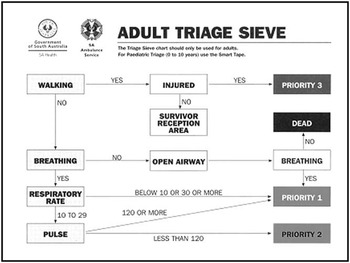
Figure 3 Aide-memoir.
Educational Refresher
A triage sieve Power Point (Version 14, Microsoft Corporation; Redmond, Washington USA) educational refresher was developed and delivered by the Principal Researcher. This was delivered as “just-in-time training,” followed by a short question period lasting no more than five minutes.Reference Hayward 33 It was outlined to the participants that the educational refresher should not be considered as a formal organizational triage education or training package.
Data Analysis
Casualty priorities for the questionnaire were agreed upon prior to data collection through a modified Delphi methodology, based upon the aide-memoir (Figure 3), which uses numerical values and the word “dead” and the term “SRA.”
Completed questionnaires were collected and coded with the data tabulated in a Microsoft Excel spreadsheet (Version 14, Microsoft Corporation; Redmond, Washington USA). Coding was in line with Kilner,Reference Castle 5 where the responses were coded: correct; incorrect – under-triaged (given a priority lower than that assigned during the Delphi process); or incorrect – over-triaged (given a priority higher than that assigned during the Delphi process). Any responses without a triage priority were coded incorrect – under-triage. Any numerical value recorded by a participant that was greater than Priority 3 (ie, Priority 4 and upwards) was assigned as incorrect – under-triage.
The word “dead” and the term “SRA” were accepted without question and recorded as being triage sieved correctly, as both these terms are included on the aide-memoir; unless they were preceded by a numerical value indicating a treatment priority (ie, Priority 3 SRA), then the numerical value took precedence and coded appropriately.
The word “walking” was also accepted in place of Priority 3, although not technically in line with the aide-memoir. This acceptance was due to the fact the first person conducting a triage sieve may ask all the “walking” casualties to move to a certain geographical location and not actually attach a triage tag, therefore considering these casualties as “walking” until appropriately triaged and a triage tag is attached. All other words were coded as incorrect –under-triage, as no triage priority had been assigned.
During the coding phase, a number of comments (made by the participants) were noted on the questionnaires for questions numbered six and nine. This resulted in extra discussion amongst the Delphi group to review their agreed triage priorities for these questions. Question six related to an 8-year-old male. Four participants, all from Sub-group 1.2, did not assign a triage priority to this casualty. Three participants made notes on the questionnaire indicating that they didn’t have a SMART TAPE (TSG Associates; Halifax, England), a pediatric triage sieve assessment tool which is based upon pediatric physiological assessment criteria (the SMART TAPE was not included as part of this study), and the fourth participant indicated that the triage sieve is not used for pediatrics. Therefore, as the SMART TAPE was not available to the participants, the results from question six have been excluded from the analysis and therefore have not been reported.
Question nine, a 50-year-old female wandering around in a distressed state, uncooperative/unable to determine respiratory rate or pulse, was deemed to a be a Priority 3 during the original Delphi process. A number of responses had this casualty going to the SRA. The casualty descriptor doesn’t specify an injury or any abnormal physiological observations; therefore, this casualty may be suitable for the SRA. The Delphi group reconvened to consider the participants’ responses to this question where the following was discussed: that this casualty may be suffering with a psychological injury (which on reflection may be true); and that injuries are not accounted for during the triage sieve process (although the triage sieve aide-memoir does question if the casualty is injured in relation to mobility, but does not assess the injury), as it is purely a physiological assessment. These discussions could not reach a consensus; therefore, the priority determined through the original Delphi process (Priority 3) was the only answer accepted.
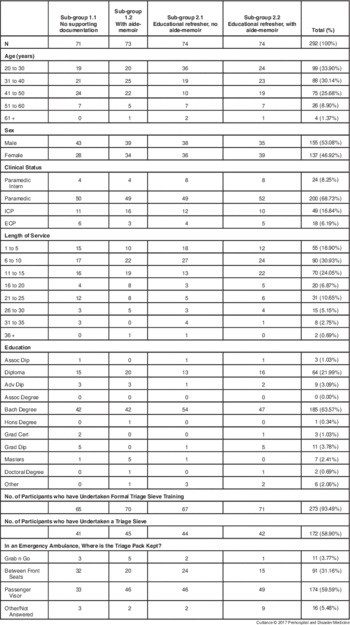
Percentages for the demographics table (Table 1) and the overall triage table (Table 2) were calculated in Microsoft Excel spreadsheet. The mean number of correct, under-triaged, and over-triaged cases (responses) was compared within and between research sub-groups using a One-way ANOVA with a Bonferroni post hoc analysis on SPSS Version 22 (IBM Corporation; Armonk, New York USA).
Table 1 Demographics

Abbreviations: ECP, extended care paramedics; ICP, intensive care paramedics.
Table 2 Overall Triage Results

Note: Although Casualty 8 was not reported on in the results section, it has been included in this table to give an overview of all the responses received as part of this study.
Results
From a metropolitan operational population of 831, the study inclusion criteria provided a sample population of 514, from which, 292 data sets were obtained providing a confidence level of 99% (SD=5%). Participants had the option not to answer all questions; this is reflected where not all demographical information totals 292 or 100%.
The demographics for the sample group are shown in Table 1 with 53.08% being males and 46.92% females. Most responders were in the age brackets of 20-30 (33.90%), 31-40 (30.14%), and 41-50 (25.68%) with study groups generally having a similar distribution of ages, except for Sub-group 2.1, which was skewed to the 20-30 brackets. The majority of the participants were paramedics (68.73%) with a similar distribution of clinical status obtained between groups. Consistent with the number of paramedics participating in the study, 64% had completed a Bachelor’s degree. In general, most participants had been with the SAAS for between one and 15 years, with the length of service reasonably well-distributed between groups.
Ninety-four percent of participants reported having undertaken formal organizational triage sieve training, but organizational triage sieve training was not reviewed as part of this study; 58.90% had performed a triage sieve as part of their training or in a real-life situation. Overall, 59.59% of participants knew the correct location of the triage pack in an SAAS emergency ambulance (above the passenger’s visor).
The results obtained from the two research arms of the study are shown in Figure 4A and Figure 4B, whereas Table 2 shows the combined responses obtained from all the questionnaires. Analysis of the responses from Research Arm 1 (Figure 4A) shows that with no intervention (Sub-group 1.1), the number of casualties triaged correctly was not significantly different from the number of casualties who were under-triaged (33.3 [SD=4.4] and 26.6 [SD=7.6], respectively). Both the correct and under-triaged rates, however, were significantly higher than the number of over-triaged casualties (11.1 [SD=6.4]; P<.05; Figure 4A). When supporting documentation in the form of an aide-memoir was provided (Sub-group 1.2), the accuracy response rate was found to be 65.8 (SD=4.9), which was significantly different to both the under-triaged 2.1 (SD=1.5) and over-triaged 5.1 (SD=5.0) response rates (P<.05; Figure 4A).

Figure 4 Triage Outcomes across Research Arms: A. Research Arm 1. B. Research Arm 2. Note: Data shown are mean ± SD. Significant differences between sub-groups (P<.05) are indicated by matching corresponding letters (eg, if two bars have a similar letter above them, then those two bars are significantly different from each other).
The responses from Research Arm 2 (Sub-group 2.1) show that provision of an educational refresher alone resulted in a significantly greater number of correctly triaged casualties (56.4 [SD=4.9]), compared to those that were under- or over-triaged (11.5 [SD=6.4] and 6.1 [SD=5.5], respectively; P<.05; Figure 4B). When the aide-memoir was provided to supplement the educational refresher (Sub-group 2.2), a similar profile of responses was obtained with a significantly greater number of correctly triaged casualties (65.9 [SD=5.4]) compared to the under- and over-triaged response rates (2.2 [SD=5.6] and 5.9 [SD=2.0], respectively; P<.05; Figure 4B).
Figures 5A-C directly compare the number of casualties correctly triaged, under-triaged, or over-triaged across each sub-group in the study. Overall, there was a statistically significant difference in the number of cases correctly and under-triaged between the four sub-groups (F (8, 152)=13.6; P<.001; Pillai’s trace=1.57, partial η2=.785). Figure 5A demonstrates that compared to Sub-group 1.1 (no supporting documentation), all other groups had a significantly greater number of correctly triaged cases. Clear improvements were found when participants were provided with an aide-memoir alone or in combination with an educational refresher (Sub-group 1.2 mean diff=32.3; P<.001 and Sub-group 2.2 mean diff=32.55; P<.001, respectively). While the provision of an educational refresher alone (Sub-group 2.1) also significantly increased the triage accuracy rate (mean diff=23.3; P<.001), post-hoc analysis (using the Bonferroni test) confirmed the improvement was not as great as when an aide-memoir was provided (Sub-group 1.2 v 2.1; mean diff=9.00; P=.03 and Sub-group 2.1 v 2.2; mean diff=-9.25; P=.02; Figure 5A).

Figure 5 Comparison of Triaging Accuracy between Research Groups: A. Correct. B. Under-Triage. C. Over-Triage. Note: Data shown are mean ± SD. Significant differences between sub-groups (P<.05) are indicated by matching corresponding letters (eg, if two bars have a similar letter above them, then those two bars are significantly different from each other).
Figure 5B shows the collated under-triaging rates of each sub-group. Sub-group 1.1, with no supporting documentation, had the greatest under-triaging rate which significantly reduced when participants were provided with an aide-memoir (Sub-group 1.2 mean diff=-24.4; P<.001) and an educational refresher alone or in combination with an aide-memoir (Sub-group 2.1 mean diff=-15.45; P<.001 and Sub-group 2.2 mean diff=-24.35; P<.001, respectively). Consistent with the results shown in Figure 5A, both sub-groups who received an aide-memoir (1.2 and 2.2) had a significantly lower under-triage rate than Sub-group 2.1 (educational refresher only; mean diff=-8.95; P=.03 and mean diff=8.9; P=.03, respectively; Figure 5B). Overall, Sub-groups 1.2 and 2.2 were found to produce equivalent improvements in both correct and under-triaging rates as there were no significant differences between these sub-groups (Figure. 5A and 5B). There were no post hoc statistical differences between the over-triaged responses of any of the sub-groups (Figure 5C).
Discussion
It is well known to all emergency services personnel that MCIs provide a particularly challenging environment in which to perform their specialist tasks. Against this backdrop, optimizing patient medical outcomes from an MCI relies on the application by first responders of a designated triage system that often receive limited continuous training and practice due to the relatively infrequent occurrence of MCIs in general. As such, the triage system employed needs to be easy to apply by the first medical responders and needs to provide high accuracy rates with minimal operational investment into deployment, education, and ongoing training.Reference Aitken and FitzGerald 7 - Reference Arshad, Williams and Asaeda 9 This study specifically compared the impact on triage sieve accuracy rates by front-line paramedics of a just-in-time educational refresher, and/or the use of an aide-memoir compared to a non-intervention control group that relied on existing knowledge of triage protocols to guide their decision making during the paper-based exercise.
The results show the use of a printed aide-memoir while performing a MCI triage sieve provides the greatest potential for optimal patient outcomes, as it produced the highest accuracy rate with minimum intervention. This outcome contrasts with the suggestion by SappReference Hayward 33 that there is no “significant difference” or “additional value” between using printed triage decision-making tools and not using printed triage decision-making tools following an educational intervention. However, it does conform with the results of a previous study supporting the use of printed aide-memoirsReference Sapp, Brice and Myers 34 and does show that the printed aide-memoir used in this study was able to ensure under- and over-triage rates were consistent with currently acceptable criteria.Reference Cross and Cicero 12 , 16 Therefore, utilizing a printed aide-memoir would appear to provide a much more cost-effective and operationally accessible approach for ambulance services to achieve acceptable patient outcomes from a MCI than the prospect of providing an educational refresher at regular intervals to ensure an adequate level of triage sieve protocols are retained.
The non-intervention control group participants raised some concerns, as it was perceived to be researching a process outside the standard practice (ie, not undertaking a triage sieve without the use of an aide-memoir) for the paramedic population sampled; it does further reinforce why a printed aide-memoir should be used. Although this group demonstrated what appears to be a reasonable baseline accuracy rate of around 47%, it also produced a high under-triage rate of 37% which would potentially lead to poor patient outcomes. As noted by Navin,Reference Kilner and Hall 35 it is unreasonable to expect emergency responders to remember and accurately apply rarely used triage-sieve decision trees, with flowchart type protocols providing an appropriate tool to assist with this process. Given that Paramedics Australasia (Melbourne, Victoria, Australia) includes “Emergency Management and Triage” within the scope of practice for paramedics (Professional Stream),Reference Navin and Waddell 36 there is the implication that professional groups should maintain a certain level of competency in triage knowledge and proficiency in the application of triage skills. These results show that while there is an apparent underlying level of competency that can be quickly and relatively easily enhanced by the provision of an educational refresher, the use of a printed aide-memoir can offset any knowledge atrophy gaps.
A crucial enabler for the effective use of the triage sieve aide-memoir is that paramedics must be able to locate the triage pack (which contains not only the aide-memoir, but also the triage tags). Since these results show that only 59.59% of the population knew the correct location of the triage pack in a SAAS emergency ambulance, ambulance services should be encouraged to ensure that any educational refreshers include details on where to find the triage pack, as much as how to use it.
Triage accuracy in MCIs is of primary importance to ensure critically injured patients are not overlooked (under-triaged), and that medical resources are not over-burdened by casualties with minor injuries (over-triaged). To provide some structure, the guidelines for field triage, target under-triage and target over-triage rates of less than five percent and<50%, respectively,Reference Wesson and Scorpio 15 have been proposed based on retrospective analysis of MCIs.Reference Cross and Cicero 12 , 16 This study indicates an under-triage rate of less than five percent is achievable and supports previous studies advocating the utility of this measure.Reference Hogan and Brown 22 , Reference Hayward 33 , Reference Sapp, Brice and Myers 34 , 37 Conversely, the over-triage goal of<50% seems to be an over-estimation, given an average over-triage percentage of ≤27% was achieved in all sub-groups, although the provision of an aide-memoir brought this percentage down as low as 14%. As such, more consideration should be given to the over-triage benchmark, particularly given the ability of an aide-memoir to keep this at a low level, and hence, reduce the burden on what would already be stretched medical resources in the MCI context. The consistency of outcomes from this study are similar to others studies using the same questionnaire.Reference Castle 5 , Reference Sapp, Brice and Myers 34
While there are limited studies that relate directly to the triage sieve, several reporting frameworks have been discussed in the literature; these frameworks provide details on community assessment and the reporting of a disaster at a macro level, but there has been little focus on the micro level, such as the triage sieve.Reference Ersoy and Akpinar 38 ArmstrongReference Jenkins, McCarthy and Sauer 29 notes inconsistent approaches to practice and communication at a MCI (or disaster) can lead to poor outcomes. A standardized guideline for MCI triage would be a valuable tool to help maximize utilization of resources and improve patient survival; several key goals identified to underpin such a guideline or triage accuracy framework have been identified; these goals include simplicity, time efficiency, predictive ability, reliability, and accuracy.Reference Jenkins, McCarthy and Sauer 29 In addition to the checking of casualty priorities against a predetermined algorithm, a triage accuracy framework should also take into consideration the type and location of an incident and the dynamic nature of triage. While the development of such a framework needs further consideration, this study demonstrates the provision of an aide-memoir should be a core component.
Limitations
Limitations of this study are firstly that it has only involved a metropolitan emergency ambulance-based sample from a state-based ambulance service and has not included other organizational sectors, such as non-emergency ambulance personnel, the volunteer sector, or career country personnel. Secondly, the Team Leaders from the sample group were excluded, therefore not providing a complete cross section of the sample group. Thirdly, triage accuracy rates were raised during the discussion. This study has reported against the currently documented field triage accuracy rates; these field triage accuracy rates could be inappropriate for MCI triage and therefore misleading.
Being a paper-based exercise, it was completed in a controlled environment. There were no external pressures that would be experienced in an uncontrolled, operational environment while undertaking a triage sieve, such as noise and sight distractions. Although a time limit was placed upon the participants to add some pressure, the time limit was taken from previous research and does not appear to have any validation.
This study focused on the adult triage sieve using an aide-memoir; it has not reviewed or considered pediatric triage sieve using an appropriate assessment tool. Pediatric triage sieve using the SMART triage process requires the use of a SMART TAPE. The SMART TAPE is a specifically designed adaptation of the adult triage sieve aide-memoir for pediatric casualties with physiological assessment criteria based upon pediatric length and age. This limitation therefore does not provide a holistic picture across the complete age range of possible casualties that may be involved in a MCI.
Conclusion
This study has shown that when paramedics from a state-based ambulance service utilized an aide-memoir to triage sieve 20 casualties from a questionnaire, there was a significantly higher correct triage accuracy rate with a concomitant reduction in under- and over-triage rates compared to those paramedics who did not utilize an aide-memoir. Although a “just-in-time” educational refresher was provided to two sub-groups of this study, the overall usefulness in terms of results and practical application is questionable, as it did not produce a significant statistical difference between these two sub-groups and the sub-group of paramedics who only utilized the aid-memoir. The use of an aide-memoir when conducting a triage sieve is strongly recommended.