Introduction
The frequency of mass-casualty incidents has increased over the past few decades. Once a mass-casualty incident occurs, an imbalance between the number of casualties and the medical resources available usually follows. In such settings, triage has an important role in achieving adequate medical management to the largest possible number of casualties. The objective of triage is to provide the appropriate care for each patient in the right time and place. In contrast to the primary triage, secondary triage has a lot of limitations to be practiced. It can be performed only in the setting with relatively sufficient number of staff and medical resources. However, it has a great role to refine the results of primary triage. The objectives of secondary triage are to identify the patients needing medical care and decide their treatment priority based on physiological and/or anatomical variables.
In Japan, the Simple Triage and Rapid Treatment (START) method is the most frequently used for primary triage. The Physiological and Anatomical Triage (PAT) method and the Triage Revised Trauma Score (TRTS) are widely used for secondary triage.Reference Smith 1 However, the START, PAT, and TRTS methods all lead to over-triage of children due to age-related differences of physiological variables.Reference Wallis and Carley 2 - Reference Gausche-Hill 4 In fact, no triage methods have been validated for children, especially for use in secondary triage.
Accordingly, this study was performed to develop a new secondary triage method for children in the disaster setting, the Pediatric Physiological and Anatomical Triage Score (PPATS), and to compare its accuracy for identifying patients who require immediate treatment with that of currently available triage methods, PAT and TRTS.
Methods
Subject
This study involved retrospective chart review of patients admitted to the Advanced Critical Care and Emergency Center, Yokohama City University Medical Center, Japan from April 1, 2014 through March 31, 2016. Inclusion criteria were as follows: (1) patients under 16 years old; (2) patients with an emergency department stay of over three hours; (3) patients transported directly from the incident scene; and (4) patients with vital sign data for calculation of the PPATS, PAT, and TRTS. Patients with out-of-hospital cardiac arrest were excluded from this study. The intensive care unit (ICU)-indicated patients were defined as having the triage priority of “immediate.”
Three authors (CT, TM, MG) independently reviewed the chart of all the patients and performed the patient selection, then confirmed all selected patients.
Ethics
This retrospective chart review was found to be approved at the Independent Ethics Committee of Yokohama City University School of Medicine, Japan to assure that patient confidentiality was maintained. Obtaining a consent from a patient had been waived due to the nature of the study design, which was an observational study.
Data Collection
The following data were collected for each patient: demographic variables (sex and age in months); clinical characteristics (mechanism of injury and predicted mortality rate calculated by the pediatric index of mortalityReference Kaziel, Meckler and Brown 3 ); outcome information (duration of mechanical ventilation [day], ICU stay [day], hospital stay [day], and in-hospital mortality [%]); physiological variables (Japan Coma Score, Glasgow Coma Score [GCS], respiratory rate [RR], SpO2 [%], heart rate [HR], systolic blood pressure [sBP], and body temperature [degree Celsius]); and anatomical variables (compound depressed skull fracture, jugular venous distention, subcutaneous emphysema of the neck or chest, flail chest, open pneumothorax, abdominal distension, pelvic fracture [flail and/or tenderness and/or leg length discrepancy], bilateral femoral fracture, quadruple amputation, quadriplegia, penetrating injury, degloving injury, and severe burns [and/or facial and/or inhalation burns]).
Criteria of the PPATS, PATS, TRTS
The PPATS was calculated from RR, HR, sBP, GCS, anatomical abnormalities, and need for life-saving intervention. Based on previous reports,Reference Fleming, Thompson and Stevens 5 , 6 representative centiles of RR (which were 1st, 10th, 25th, 75th, 90th, and 99th) and the normal range of sBP for each age were calculated (Appendix 1; available online only). Anatomical abnormality was defined as the presence of at least one of the above-mentioned anatomical variables. Life-saving intervention was defined as tracheal intubation, mechanical ventilation, chest and/or abdominal drainage, or emergency hemostasis. For calculation of the PPATS, scoring was performed as follows: 0=normal, 1=mild, 2=moderate, 3=severe, and 4=serious. The RR and HR were assigned scores from zero to three (0=25th-75th, 1=10th-25th or 76th-90th, 2=1th-9th or 91th-99th, and 3=<1th or >99th) and the other four variables were assigned scores from zero to four. The sum of those six items consisted of PPATS with 22 as the maximum score (Table 1). Patients with scores higher than the optimum cut-off value were assigned the triage priority as “immediate.”
Table 1 Pediatric Physiological Anatomical Triage Scoring System: PPATS

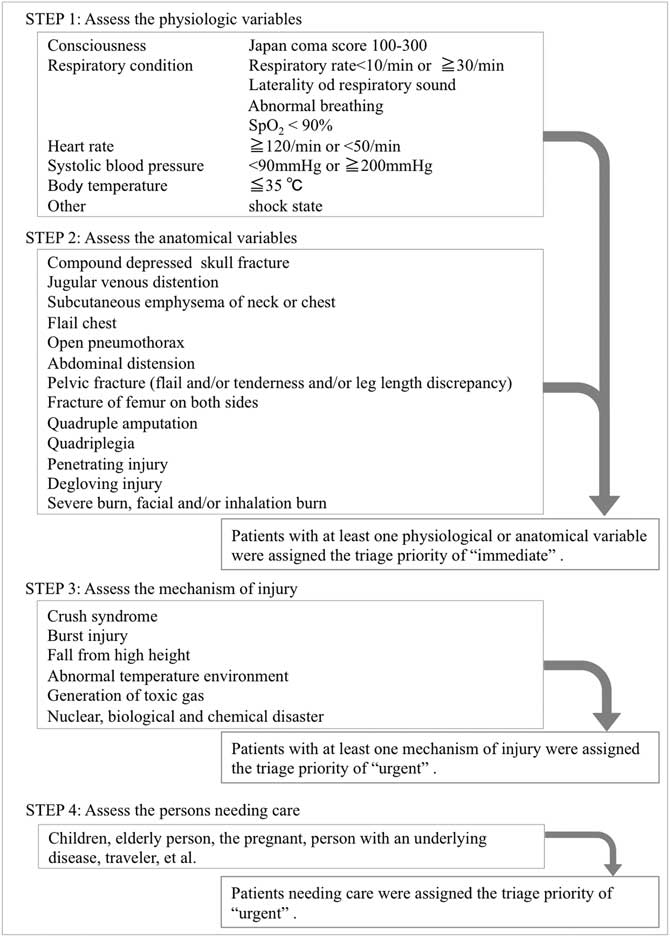
The PAT was assessed on the basis of four factors, which were physiological variables, anatomical variables, mechanism of injury, and persons needing care. Patients with at least one physiological or anatomical variable were assigned the triage priority as “immediate” (Figure 1).
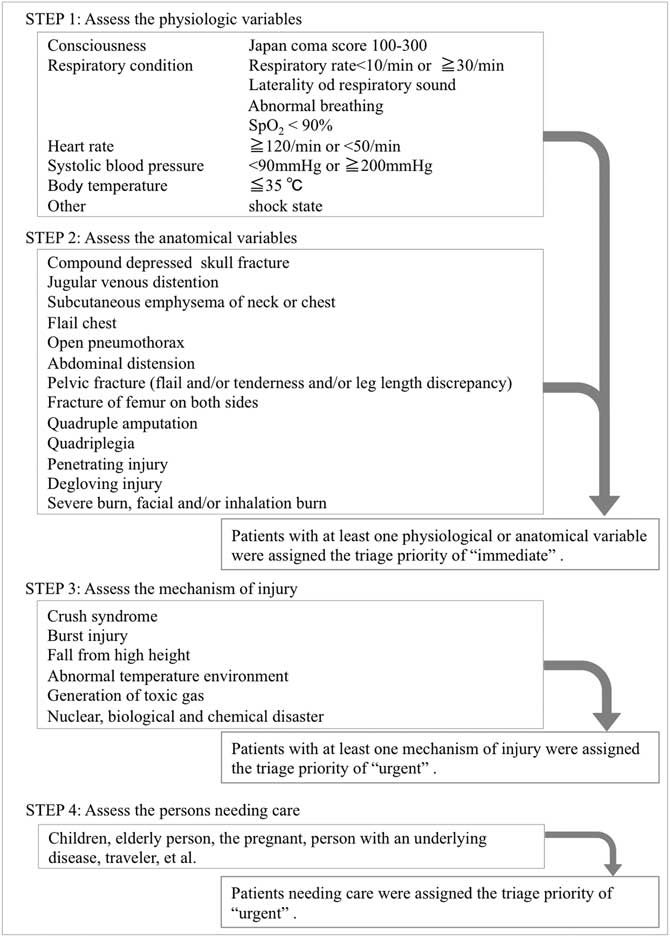
Figure 1 Physiological and Anatomical Triage: PAT. The PAT was assessed on the basis of four factors: physiological variables, anatomical variables, mechanism of injury, and persons needing care. Patients with at least one physiological or anatomical variable were assigned the triage priority of “immediate.”
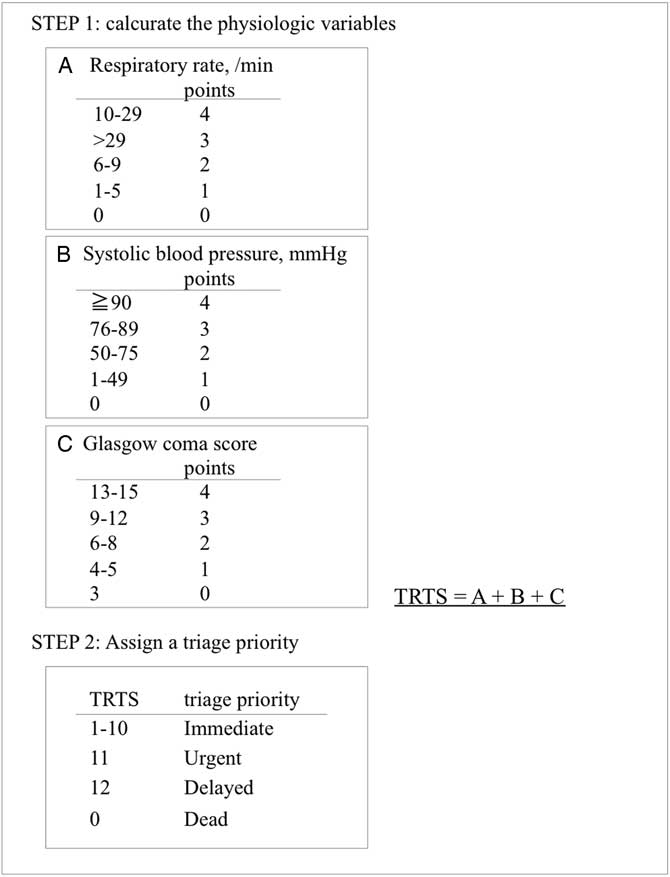
The TRTS was scored from RR, sBP, and GCS, with 12 as the maximum possible score. Patients with scores between one to 10 points were assigned the priority as “immediate” (Figure 2).
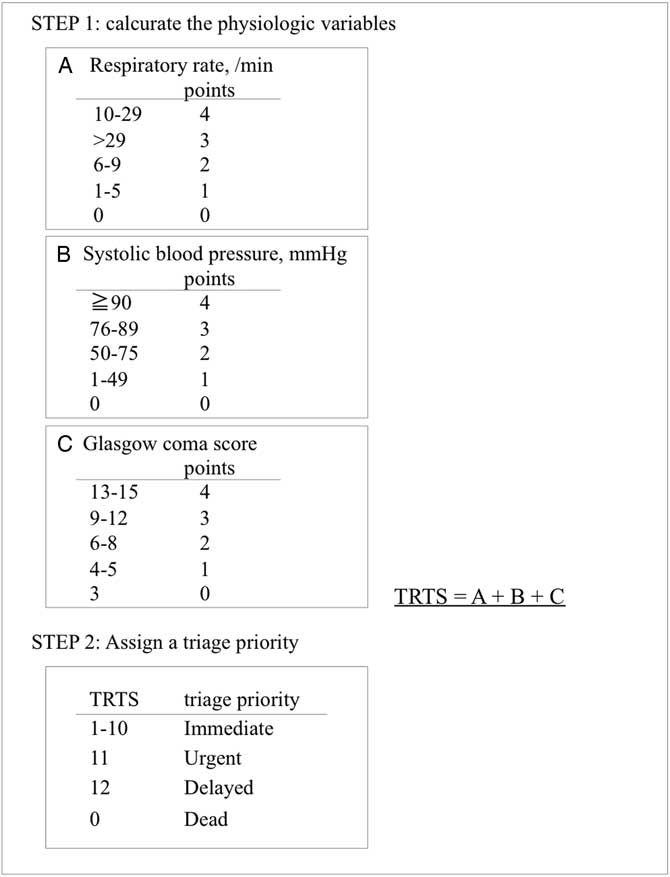
Figure 2 Triage Revised Trauma Score: TRTS. The TRTS was scored from the respiratory rate, systolic blood pressure, and Glasgow Coma Score with the maximum possible score being 12. Patients with scores of 1-10 points were assigned the priority of “immediate.”
Statistical Analysis
Data were expressed as median and interquartile range (25th - 75th percentile) for continuous variables or as percentages for categorical variables. The Mann-Whitney U test was used for analysis of continuous variables and Fisher’s exact test for categorical variables in order to compare between ICU admitted patients and the other.
Primary Analysis
In this study, a new secondary triage method (PPATS) was compared with two other methods (PAT and TRTS), which were currently utilized in Japan, to determine that PPATS would be superior to the two for predicting the triage priority as “immediate.” The accuracy of each method was assessed by determining the area under the receiver-operating characteristic curve (AUC). Then, AUC values were compared among the three methods. The optimum cut-off value for assigning the triage category as “immediate” was defined as that with the maximum combination of sensitivity and specificity. This study also obtained positive predictive value (PPV) and negative predictive value (NPV) for each triage method for comparison.
Secondary Analysis
This study also estimated the association between the PPATS and the predicted mortality rate, ventilation time, ICU stay, and hospital stay by using univariate regression analysis.
In all statistical tests, an α value of 0.05 with two-sided was defined as indicating significance. Analyses were performed using STATA SE software, version 12.1 (StataCorp; College Station, Texas USA).
Results
A total of 137 patients met the inclusion criteria of the study. The median age was 39 months and 59.9% were male. Of these 137 patients, 24 (17.5%) were admitted to ICU and their characteristics are shown in Table 2. The patients admitted to ICU had the median age of 135 months (interquartile range [IQR]: 99-170 months). The median ventilation time, ICU stay, and hospital stay were three days (IQR: 0-10 days), five days (IQR: 3-13 days), and 15 days (IQR: 4-38 days), respectively, while the median predicted mortality rate was 3.9% (IQR: 1.5-5.0%). The median PPATS score was significantly higher in the patients admitted to ICU than in those not admitted to ICU (11 [IQR: 9-13] versus three [IQR: 2-4]; P<.001].
Table 2 Characteristics and Hospital Course
Abbreviations: ICU, intensive care unit; PPATS, Pediatric Physiological Anatomical Triage Scoring System.
Development and Accuracy of PPATS
According to AUC analysis, the optimum cut-off value of the PPTAS was six. The sensitivity, specificity, PPV, and NPV of the PPATS were respectively 95.8%, 86.7%, 60.5%, and 99.0% at cut-off value of six (Table 3). The PPATS was also compared to two existing secondary triage methods, revealing that the AUC was larger for PPATS than for PAT or TRTS (0.95 [95% CI, 0.87-1.00] versus 0.65 [95% CI, 0.58-0.72]; P<.001 and 0.79 [95% CI, 0.69-0.89]; P=.003, respectively; Figure 3).
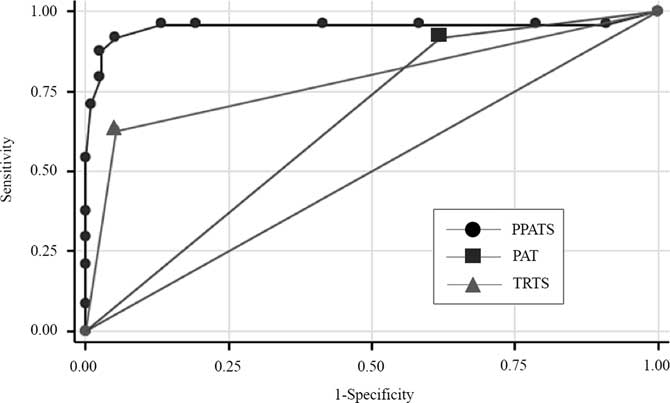
Figure 3 Receiver-Operating Characteristic Curves for the PPATS, PAT, and TRTS. The AUC was larger for PPATS than for PAT or TRTS (0.95 [95% CI: 0.87-1.00] versus 0.65 [95% CI: 0.58-0.72]; P<.001 and 0.79 [95% CI: 0.69-0.89]; P=.003, respectively). Abbreviations: AUC, area under the receiver-operating characteristic curve; PAT, Physiological and Anatomical Triage; PPATS, Pediatric Physiological Anatomical Triage Scoring System; TRTS, Triage Revised Trauma Score.
Table 3 Performance of the PPATS, PAT, and TRTS

Abbreviations: AUC, area under the receiver-operating characteristic curve; NPV, negative predictive value; PAT, Physiological and Anatomical Triage; PPATS, Pediatric Physiological Anatomical Triage Scoring System; PPV, positive predictive value; TRTS, Triage Revised Trauma Score.
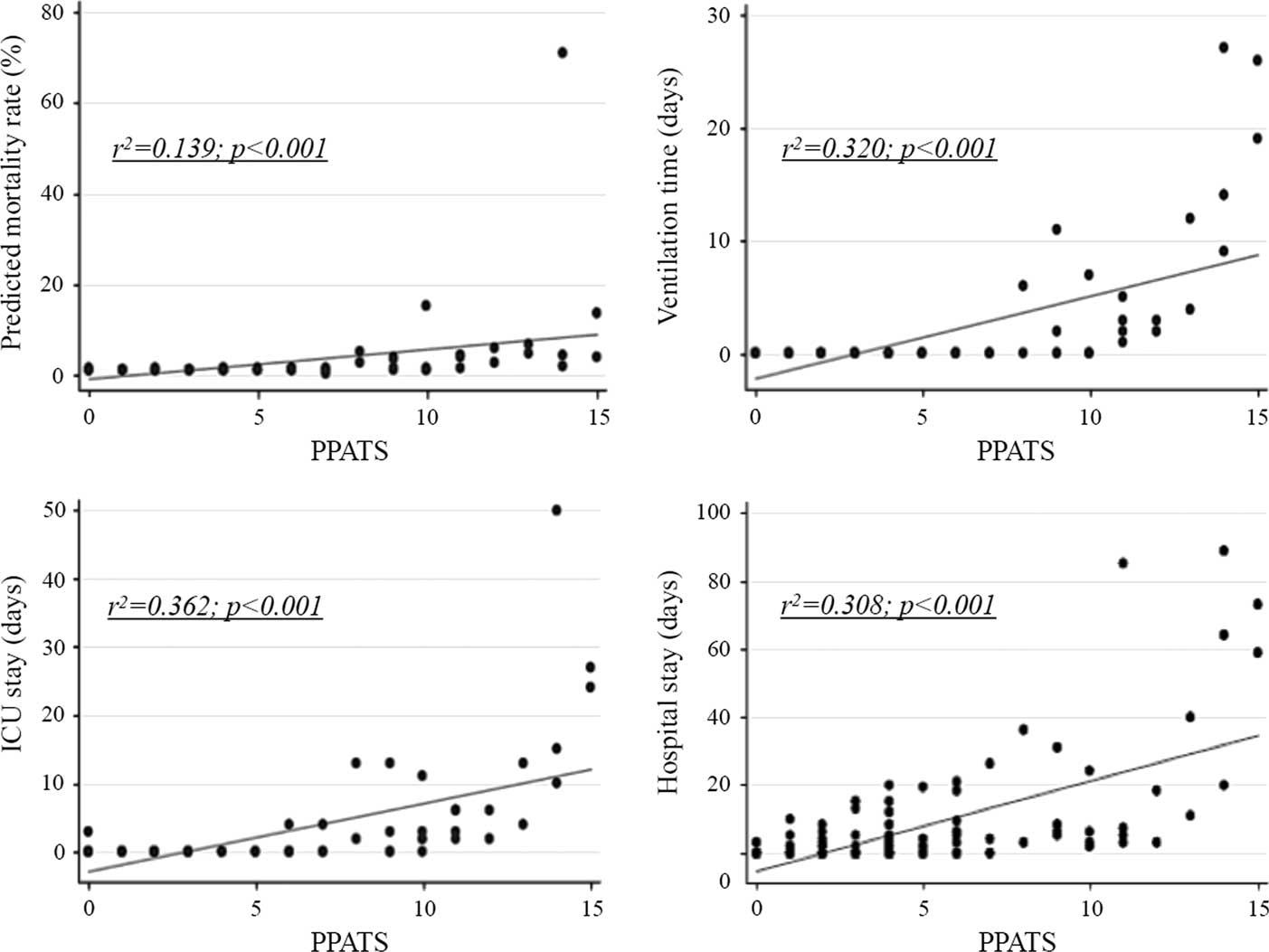
Association between PPATS and the Severity/Outcome
Regression analysis showed a significant association between the PPATS and the predicted mortality rate (r2=0.139; P<.001), ventilation time (r2=0.320; P<.001), ICU stay (r2=0.362; P<.001), and length of hospital stay (r2=0.308; P<.001; Figure 4).

Figure 4 Association between the PPATS and the Predicted Mortality Rate, Ventilation Time, ICU Stay, and Hospital Stay. Regression analysis showed a significant association between the PPATS and the predicted mortality rate (r2=0.139; P<.001), ventilation time (r2=0.320; P<.001), ICU stay (r2=0.362; P<.001), and hospital stay (r2=0.308; P<.001). Abbreviations: ICU, intensive care unit; PPATS, Pediatric Physiological Anatomical Triage Scoring System
Discussion
This study developed a new secondary triage method for children, PPATS, and investigated the accuracy of the method. Two main findings were obtained. First, the PPATS could accurately identify pediatric patients with the triage priority as “immediate” from among the patients transported to the emergency center by using variables that were available in the emergency department. Second, the PPATS could accurately determine the triage priority according to the severity of patient’s condition.
In addition, the PPATS was more accurate for identifying high-priority patients than currently utilized for secondary triage, the PAT or TRTS methods. Triage methods that assess physiological variables have generally been favored in the setting of major incidents, because such methods are designed to identify unstable patients. However, age-related variations of physiological variables might cause a difficulty for accurate triage by such methods in children.Reference Kaziel, Meckler and Brown 3 , Reference Gausche-Hill 4 Several systems based on physiological variables tend to result in over-triage in children, especially when primary triage was performed using START, JumpSTART, CareFlight, and Pediatric Triage Tape.Reference Garner, Lee and Harrison 7 As well as under-triage, over-triage may lead to an increase of morbidity and mortality.Reference Aitken and FitzGerald 8 , Reference Donofrio, Kaji and Claudius 9 Therefore, it is important for secondary triage of disaster victims. When more time and medical resources are available, it has a great role to refine the result of primary triage in order to provide accurate evaluation sufficiently and to prevent over-triage or under-triage.
In Japan, the PAT and TRTS are most widely used as secondary triage methods for children.Reference Smith 1 However, the physiological variables assessed by PAT and TRTS are not suitable for pediatric patients due to age-related variations. To overcome the disadvantages of these conventional methods, age-based assessments of physiological variables were adopted (Appendix 1; available online only), and the PPATS showed superior accuracy to the other triage methods. In the future, it will be necessary to increase its accuracy and convenience for evaluation and sorting of patients by incorporating PPATS in electronic triage systems.
This study demonstrated that PPATS could accurately determine triage priority for children according to the severity of their condition among a large number of patients transported to the emergency department. It is crucial for providing suitable care to the maximum number of casualties when there is an imbalance between the number of disaster victims and the available medical resources. Moreover, this study identified a significant association between the PPATS and the ventilation time, length of ICU stay, and length of hospital stay. That is, patients with a high PPATS score were more likely to heavily utilize medical resources after admission to hospital. In cases of mass-casualty incidents, it is recommended that patients with a large requirement for medical resources should be transported from the disaster zone with insufficient medical resources to another area where medical resources are adequately provided. 10 Therefore, it is also crucial for a triage system to be able to determine the priority of disaster victims for medical evacuation. Results obtained with the PPATS in this study suggested that it could not only be used to determine the priorities for medical treatment, but also those for medical evacuation outside the disaster zone. Since it is more difficult to assess the severity of illness in children than in adult patients, the PPAT is very helpful for providing objective data to prioritize patients.
Limitations
This study had several limitations, with the first being its retrospective design. First, a new method is generally validated through three steps: derivation, retrospective validation, and prospective validation; this study only covered the first two steps. Second, this study was conducted at a single center in a limited population. Third, this study was retrospective. Accordingly, a large-scale prospective study will be needed to confirm the accuracy of the PPATS for performing triage of pediatric patients.
Conclusions
The accuracy of PPATS, a newly developed secondary triage method for children, was superior to current triage methods (PAT and TRTS). The PPATS method is not only useful for identifying high-priority patients, but it can also determine the priorities for medical treatment and evacuation. In the future, it would be beneficial to increase the accuracy and convenience of evaluation by incorporating the PPATS into electronic triage systems.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1049023X18000109