Introduction
Acute myocardial infarctions (AMIs)—heart attacks—represent a very significant portion of the overall cost and mortality associated with cardiovascular disease, 1 - 5 with approximately 620,000 Americans suffering a first heart attack and 295,000 suffering a repeat event each year.Reference Go, Mozaffarian and Roger 3 Early recognition of an AMI can increase the patient’s likelihood of survival,Reference Bang, Grip and Herlitz 6 especially when early recognition leads to early treatment and transport in the prehospital setting.Reference Hochman, Sleeper and Webb 7 As the first point of contact for patients accessing medical care through emergency services, emergency medical dispatchers (EMDs) represent the earliest potential identification point for AMIs, with EMDs who accurately identify AMIs able to assign a high-priority level to the case and send appropriate Advanced Life Support (ALS) resources.
Trained EMDs using clinically-based, scripted protocols have been shown to be able to identify high-acuity events such as cardiac arrests,Reference Clawson, Olola and Heward 8 as well as other types of medical cases requiring the administration of ALS interventions.Reference Sporer and Wilson 9 Unlike cardiac arrest, though, which is comparatively easier to identify over the phone, heart attacks are complex and can present quite differently between individuals. 10 , Reference Brady 11 Females in particular often present with heart attacks showing few or none of the stereotypical heart attack symptoms, and may receive less-effective treatment as a result,Reference Meisel, Armstrong and Mechem 12 or may have their AMIs missed completely.Reference Moy, Barrett and Coffey 13
Such a diversity of presentations makes heart attacks difficult enough to identify face-to-face. Over the phone, identification is further complicated by the lack of visual and other sensory information, the inability to perform tests, and the fact that the caller may not be right with the patient or know the patient’s medical history. As a result, it is imperative that EMDs are provided and required to comply with standardized protocols that ensure that they ask pre-determined, relevant questions to identify the highest-acuity symptoms. The Task Force on the Management of Chest PainReference Zadek 14 has outlined conditions that a medical dispatcher should listen for, such as severe discomfort located anywhere in the chest and “symptoms associated with sweating, nausea, and vomiting.” They also recommend a “fast track” (high-priority and/or fast response) for patients over 30 years old, those with discomfort that is similar to a previous AMI or previous angina, those experiencing pain or discomfort in one or both arms, or any report of “intermittent loss of consciousness.” Any medical dispatch system should thus require that EMDs ask questions that specifically ascertain these, or very similar, symptoms when evaluating patients for possible AMI.
The Medical Priority Dispatch System (MPDS; Salt Lake City, Utah USA) is a scripted protocol system that follows a questioning and information-gathering sequence closely aligned to these recommendations. Evaluating the ability of EMDs using the MPDS to identify true AMIs will help ensure the dispatch of the correct response personnel and the dispatch-advised provision of early interventions, such as aspirin administration, as well as potentially increasing the likelihood that AMI patients will be rapidly transported to a designated, specialized health facility, such as a ST-elevation myocardial infarction (STEMI) receiving center. 15
The primary objective of this study was to determine how AMIs were handled at the dispatch point by trained EMDs using the MPDS. Specifically, the study sought to characterize the Chief Complaint Protocols, dispatch priority levels, and determinant codes (specific clinical and situational dispatch codes) used by EMDs in prioritizing the AMI cases overall, as well as the mortalities resulting from AMIs. The study hypothesis was that certified EMDs using a scripted protocol would correctly triage the majority of AMI cases into higher-priority ALS response tiers and that the majority of cases ending in death at the hospital would also be triaged into these tiers.
Methods
Study Design and Setting
The retrospective, descriptive study utilized data collected from June 1, 2012 through December 31, 2013 from three sources: emergency medical dispatch, Emergency Medical Services (EMS), and emergency department (ED)/hospital. The EMS and ED/hospital data came from the Utah Department of Health (UDoH), Salt Lake City, Utah (USA). Dispatch data came from Salt Lake Valley Emergency Communications Center (VECC) and the Salt Lake City Fire Department (SLCFD), including cases referred to Gold Cross Ambulance. Both centers used MPDS version 12.2 NAE (released July, 2012) within the ProQA Paramount (Priority Dispatch Corp., Salt Lake City, Utah USA) software logic engine during the study period, and both are accredited as Centers of Excellence by the International Academies of Emergency Dispatch (IAED; Salt Lake City, Utah USA), with proven high MPDS protocol compliance. The part of the protocols studied has not changed in later versions of MPDS. The study was approved by the UDoH Institutional Review Board.
The MPDS is designed to direct certified EMDs to identify the chief complaint, severity (priority level), and specific presenting symptoms or causes of the problem (determinant descriptors) using scripted question sequences. Within the Chief Complaint Protocols, the MPDS uses six priority levels (Figure 1) to define the relative urgency and response needs of the patient. Each priority level is associated with a recommended, but still locally-determined, response assignment and travel mode: COLD or HOT. The COLD response mode comprises the OMEGA, ALPHA, and CHARLIE-level calls, while the HOT response mode comprises the BRAVO, DELTA, and ECHO-level calls. In addition, within each priority level, the EMD assigns a determinant descriptor, a succinct clinical or situational description of the presenting problem or specific highest-priority symptom.
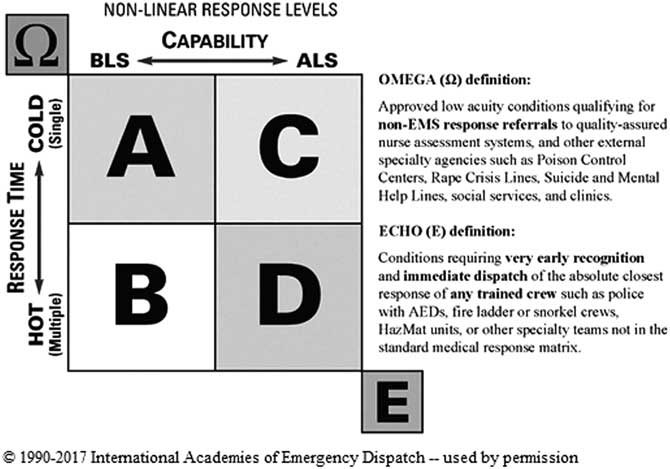
Figure 1 Medical Priority Dispatch System Priority Level Response Matrix (Non-Linear Methodology). Note: BLS: Basic Life Support ALS: Advanced Life Support HOT: Lights-and-Siren response COLD : No Lights-and-Siren response Ω: OMEGA Priority Level A: ALPHA Priority Level B: BRAVO Priority Level C: CHARLIE Priority Level D: DELTA Priority Level E: ECHO Priority Level Abbreviations: AED, automated external defibrillator; EMS, Emergency Medical Services.
Selection of Participants
The study sample included all AMIs, as identified by ICD-9-CM codes assigned at the study hospitals during the data collection period, that also had matching EMS and dispatch data records. The ICD-9-CM code used to identify cases for inclusion was 410 (Acute Myocardial Infarction). Given the purely retrospective nature of the study, the authors had no opportunity to influence or impose bias on the study population. Inclusion was based solely on the assignment of AMI ICD-9-CM codes at the hospital.
Outcomes
The primary outcome measures were the distributions of AMIs by dispatch Chief Complaint Protocol, dispatch priority level, specific determinant code, and patient age and gender. Secondary outcomes were the proportion of STEMI and Non-STEMI (NSTEMI) AMIs by dispatch priority level, and AMI deaths categorized by dispatch Chief Complaint Protocol, dispatch priority level, determinant code, and patient age and gender.
Analysis
STATA for Windows software (STATA Statistical Software: releases 14.1; StataCorp; College Station, Texas USA) was used for data analysis. All the EMS, ED, and hospital data were de-identified a priori by a data steward at the UDoH before being made available for the study. All three datasets contained a linkage data field that was used for the probabilistic linkage at the UDoH. The merged dataset was probabilistically matched (using a statistical fuzzy logic technique) 15 with the emergency dispatch records (Figure 2). The fuzzy logic utilized baseline measures such as date, time, location, age, gender, and chief complaint to calculate the probability of a match. The records in the resulting dataset were evaluated manually—duplicates on a case-by-case basis and non-duplicates by random selection—to determine the legitimacy of the matches.

Figure 2 Data Sampling Process for Acute Myocardial Infarction Cases. Abbreviations: EMD: emergency medical dispatcher; EMS, Emergency Medical Services; UDoH, Utah Department of Health.
Upon completing the matching of all the datasets, the study sample was classified into outcomes according to the ICD-9-CM codes. Descriptive statistics such as frequencies and percentages were used for statistical presentations. An initial analysis described the demographic distributions of AMI cases, categorizing by patient gender and age. The distributions of AMIs by dispatch chief complaint, priority level, and dispatch code descriptors were then determined. The final analyses described the distributions of AMIs by mortality, patient age, and gender.
Results
A total of 606 AMIs were included and analyzed in the study. Acute myocardial infarctions occurred almost exclusively among patients aged 35 years and older, who comprised 98.8% of the cases (Figure 3), then steadily decreased above age 75. Significant gender differences were observed in terms of when in life males and females were likely to experience AMIs. A higher percentage of males than females experienced an AMI between the ages of 45 and 64 (39.5% and 23.6%, respectively), while females were more likely than males to experience an AMI at age 75 or older (47.9% and 26.5%). Overall, approximately two-thirds (65.1%) of all male patients with AMIs were between the ages of 45 and 74, while two-thirds (63.6%) of the female patients experienced an AMI between the ages of 55 and 84.

Figure 3 Acute Myocardial Infarction Cases Categorized by Patient Gender and Age. Abbreviation: AMI, acute myocardial infarction. *Ages with significant gender difference in the percentage of AMIs.
The large majority (89.9%) of AMI cases were prioritized by EMDs into the higher-acuity priority levels, with 57.8% of all the AMIs prioritized at the DELTA level, 27.7% at the CHARLIE level, and 4.5% at the ECHO level. Significantly fewer AMIs were handled at the BRAVO (3.1%) and ALPHA (6.8%) levels (Figure 4).

Figure 4 Hospital-Confirmed AMIs Categorized by Dispatch Priority Levels. Abbreviations: AMI, acute myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction; STEMI, ST-elevation myocardial infarction. *One patient was coded with both a STEMI and NSTEMI ICD-9-CM code in the primary and secondary diagnoses.
Of the 606 patients presenting with an AMI, 287 (47.4%) were diagnosed with a STEMI and 319 (52.6%) were diagnosed with an NSTEMI in-hospital, based on ICD-9-CM coding—as either primary and/or secondary diagnoses. Overall, 417 patients had an AMI coded as a primary diagnosis and 193 had an AMI coded as a secondary diagnosis. Four patients total presented with multiple AMI codes in the primary and/or secondary diagnoses. Stratification by STEMI versus NSTEMI showed no significant differences in any dispatch priority level, although the NSTEMIs were slightly more common than STEMIs, quantitatively, in the ALPHA, CHARLIE, and DELTA levels, while STEMIs were more common in the ECHO level.
The five dispatch protocols with the highest percentage of AMIs were Chest Pain (43.1%), Breathing Problems (14.0%), Sick Person (9.1%), Unconscious/Fainting (8.3%), and Heart Problems (8.3%; Figure 5). Overall, 81.2% of all the AMIs were handled on these five protocols.

Figure 5 Acute Myocardial Infarctions Categorized by Chief Complaint Protocols. Abbreviation: AMI, acute myocardial infarction.
A total of 63 deaths occurred by the time of hospital discharge (10.4%; Table 1). Of these, 40 (63.5%) were male patients, and 54 (85.7%) were patients aged 55 years and older. There were no deaths recorded for patients younger than 35. Overall, 82.6% of the patients who ultimately died before discharge were cases that had been triaged into one of six MPDS Chief Complaint Protocols: Unconscious/Fainting (22.2%), Cardiac/Respiratory Arrest (15.9%), Breathing Problems (15.9%), Sick Person (12.7%), Chest Pain (11.1%), and Falls (4.8%). Additionally, most of the deaths (89.9%) were cases that had been prioritized at the higher-priority CHARLIE (20.6%), DELTA (52.4%), or ECHO (15.9%) levels. The most common specific dispatch determinant for cases that resulted in death was 9-E-1, the determinant for “not breathing at all” on Protocol 9: Cardiac or Respiratory Arrest/Death, which comprised 14.3% of the deaths. This was followed by 31-D-2, the “unconscious—effective breathing” determinant on the Unconscious/Fainting Protocol (11.1%), and 6-D-1, the “not alert” determinant on the Breathing Problems Protocol (6.3%).
Table 1 Acute Myocardial Infarctions Mortality Prior to Hospital Discharge

a All patients age younger than 35 years survived (n=7).
b Asthma.
c One case each (1.6%): Breathing Problems [Ineffective breathing (6-E-1)], Cardiac or Respiratory Arrest/Death [Ineffective breathing (9-D-1)], Chest Pain [Abnormal breathing (10-C-1), Breathing normally ≥35 years (10-C-4), Not alert (10-D-1), Clammy (10-D-4)], Convulsions/ Seizures [Not breathing - after Key Questioning (12-D-1)], Falls [Not dangerous body area (17-A-1), Serious hemorrhage – on the ground/floor (17-B-3G), Not alert (17-D-3)], Heart Problems [Cardiac history (19-C-4)], Hemorrhage/Lacerations [Abnormal breathing (21-D-4)], Overdose/ Poisoning [Not alert – Intentional (23-C-1I)], Sick Person [No priority symptoms (26-A-1), Altered level of consciousness (26-C-1)], Stroke/Transient Ischemic Attack [Not alert – less than some hours since symptoms onset (28-C-1L)], Traumatic Injuries [Possible dangerous body area (30-B-1)], Unconscious/Fainting [Fainting episode(s) and alert ≥35 years – no cardiac history (31-A-1), Alert with abnormal breathing (31-C-1), Fainting episode(s) and alert ≥35 years – with cardiac history (31-C-2), Unconscious – Agonal/Infective breathing (31-D-1)], Unknown Problem [Standing, sitting, moving, or talking (32-B-1), Medical alarm notifications – no patient information (32-B-2), Life status questionable (32-D-1)].
Discussion
As the Task Force on the Management of Chest Pain noted, the purpose of dispatch triage is not (generally speaking) to diagnose a condition, but to prioritize cases into appropriate severity categories, and thus send a case-appropriate response.Reference Erhardt, Herlitz and Bossaert 16 The results of this study indicate that trained EMDs, using a scripted protocol system, triage AMI patients into the ECHO, DELTA, and CHARLIE priority levels (for which ALS, the standard of care, is the recommended response) nearly 90.0% of the time, with a much smaller group assigned to the BRAVO level, which is intended to dispatch a Basic Life Support (BLS)-level response, but quickly (running with lights-and-siren). Very few cases were assigned to the ALPHA priority level, which is consistent with published rates of “missed” AMIs in EDsReference Tatum, Jesse and Kontos 17 —despite the fact that the very high rate of malpractice suits involving missed AMI diagnosis prompt most EDs to substantially over-triage these cases.Reference Rusnak, Stair, Hansen and Fastow 18 For a condition that is notoriously difficult for physicians to identify,Reference Conti, Bavry and Peterson 19 EMDs using the studied protocol system appear to be triaging patients into the highest priority levels effectively.
Emergency medical dispatchers also appear to be selecting appropriate Chief Complaint Protocols for handling the majority of the AMI cases. The fact that EMDs selected Chest Pain as the most frequent Chief Complaint Protocol for these patients, distantly followed by Breathing Problems, is an expected result, as both are commonly reported cardiac symptoms. Emergency medical dispatchers using the MPDS are trained to identify “priority symptoms”—an EMD term which includes chest pain/chest discomfort, abnormal breathing, serious hemorrhage, and “not alert” status—and select the associated chief complaint whenever one of these symptoms is reported for non-trauma patients. Furthermore, EMDs are trained to recognize and select the Chest Pain Chief Complaint Protocol for other potential heart attack symptoms (in non-trauma cases), such as referred pain, pressure, crushing discomfort, tightness, numbness, or heaviness. The EMDs’ somewhat less-common selection of the Unconscious/Fainting (near) and Heart Problems Chief Complaint Protocols is also expected. Depending on the specific symptoms of the patient, 911 callers often report these conditions first when they exist because they sound very critical or more attention-grabbing to layperson observers.
Cases that ended in death reflected a similar distribution of Chief Complaint Protocols, priority levels, and determinant descriptors compared to the study group overall. The most common single determinant descriptor for cases that ended in death was 9-E-1, which is appropriate, as this reflects an immediate ALS response with a report of the patient as “not breathing at all.” However, across all the Protocols, cases that ended in death were most often reported as “not alert” or having “difficulty speaking between breaths.” These are almost always DELTA-level codes and are always in priority levels standardly calling for an ALS response. Thus, although the progressive course of AMI means that the symptoms reported at the time of dispatch are not always reflective of the eventual severity or course of the incident, cases that did end in death were overwhelmingly identified as being ALS-level events.
The vast majority of AMIs occurred in patients aged 35 years and older, and all deaths were found to be in patients in that age group. This is strong evidence that the age cutoff used in the MPDS for suspected AMI (≥ 35 years) is highly reliable. A lower priority level (OMEGA, ALPHA, or BRAVO) can only be achieved when the patient is under 35 years of age and has no other priority symptoms, for both the Chest Pain and Heart Problems chief complaints; otherwise, one of the higher priority (CHARLIE, DELTA, or ECHO) levels were automatically assigned. These results are very consistent with findings of the Framingham Study,Reference Kannel and Abbot 20 a landmark, long-term, prospective study on cardiovascular disease.
One less-expected, but not surprising, finding is the relatively high incidence of AMIs within the Sick Person Protocol, especially the incidence of ALPHA-level coding on this protocol. This suggests that a number of acute cardiac conditions are reported initially by the 911 caller without mentioning any of the more common symptoms of an AMI, which is consistent with the well-documented phenomena of “silent ischemia” and AMIs presenting with atypical symptoms.Reference Valensi, Lorgis and Cottin 21 , Reference Lusiana, Perrone and Pesavento 22 In particular, calls handled on the Sick Person Protocol often noted dizziness, fever/chills, and nausea as symptoms reported by the caller—symptoms commonly associated with “missed” or atypical AMIs. The Sick Person Protocol already prompts the EMD to ask whether the patient has any pain and to “shunt” (immediately switch) to the Chest Pain Protocol if any chest pain or discomfort is reported. However, if the patient is experiencing atypical symptoms, chest pain (and other identifiable AMI symptoms) may not be present. Audio review of AMI calls assigned to the Sick Person Protocol, especially those prioritized at the ALPHA level, may be very useful in determining any patterns in reported symptoms that could indicate when a patient is experiencing an AMI with an atypical presentation.
Cases reported as falls may represent a special case for the EMD because a fall is often the first, or only reported situational condition, with the caller often not reporting, or not knowing, the cause of the fall. As a result, the MPDS differentiates between falls that represent traumatic events (such as falls from ladders or buildings) and those that may reflect underlying medical causes (sudden collapses reported as falls by bystanders). Some evidence suggests that cardiac causes might be very common in falls, especially among older people; in particular, cardiac syncope may accompany serious cardiac problems and cause the patient to collapse.Reference Tan and Kenny 23 The critical point in this situation is not so much to diagnose an underlying cardiac cause, if one exists, but to ensure that patients with serious medical causes for their falls receive high-acuity prioritization.
The results in this study indicate that AMIs handled on the Falls Protocol are triaged into the ALPHA level more commonly than AMIs handled on any other Protocol except Sick Person, suggesting that adding a “safety net” for cardiac-caused falls, when suspected, may be appropriate. As a history of cardiovascular disease has been shown to be a very strong predictor of cardiac syncope in falls in older adults,Reference Alboni, Brignole and Menozzi 24 one possibility is to add a question about cardiac history to the Falls Protocol. Such a question is already asked on a number of other Protocols and could easily be added here. A follow-up study is planned to determine the effectiveness of this addition in capturing AMIs reported as falls (without creating excessive over-triage), as well as the patient age range for which it is most relevant.
Limitations
This study had some limitations. In general, record linkage methods are imperfect. The fuzzy logic methodology does not guarantee a 100% match, even for cases with high-matching scores—despite the multiple runs with a variety of weights and combinations of matching data attributes used.
It was also not possible to review audios of the cases studied to establish the exact description of the problem by the caller/patient or the veracity of what the EMD entered for the description. One important element that cannot be determined without listening to audio is how, and how long, the EMD listens after asking the initial problem question, “Okay, tell me exactly what happened.” A common cause of incorrect problem identification or chief complaint selection is cutting off the caller and thus truncating the communication necessary to make the correct determination. However, the demonstrated high compliance to scripted protocols in the centers studied here makes this less likely.
Additionally, the study was conducted using data from only two emergency communication centers, which may impact the generalizability of the study findings.
Conclusion
Approximately 90.0% of hospital-confirmed AMI patients were correctly triaged by EMDs into the higher priority levels where ALS service is the standard, recommended response type. Emergency medical dispatchers significantly more often selected the Chest Pain and Breathing Problems Protocols to handle these calls. However, there were a number of different Chief Complaint Protocols selected in a sizeable minority of AMI cases, most notably Sick Person and Falls. Future studies should examine the reasons for the selection of such other, non-cardiac-specific Chief Complaint Protocols, and test proposed additions to at least one protocol (eg, Breathing Problems, Sick Person [Specific Diagnosis], Unconscious/Fainting [Near], Heart Problems/A.I.C.D., or Falls) to increase identification of “atypical” AMIs. Finally, the vast majority of AMI cases, and all deaths, were of age 35 years and over, verifying the results from previous research. Overall, EMDs using scripted, clinically-based protocols are able to effectively triage these time-sensitive incidents.
Acknowledgements
Thanks to VECC, SLCFD, and UDoH Bureau of Emergency Medical Services & Preparedness for the data studied. Special thanks to Shari Hunsaker of UDoH, Lin M. Shaffer of VECC, and Lisa Burnette of SLC911 for their immense input in preprocessing of the datasets. Thanks to Denise Jorgensen, IAED Administrative Assistant, for study logistics coordination. There was no source of funding for this study. The study was approved by the UDoH Institutional Review Board and the IAED Institutional Review Board.








