Introduction
Disasters create a discrepancy between the demand for health care and the capacity of health services to meet that demand. 1 The mismatch is aggravated by an adverse impact on health care services Reference FitzGerald, Capon and Aitken2,Reference Ardagh, Richardson and Robinson3 and professionals. General Practitioners (GPs) have local health care contextual knowledge, strong connections with community, and are usually onsite providing care when disaster strikes. 4,Reference Burns, Douglas, Hu, Aitken and Raphael5 Integrating and optimizing GP contributions may help address the health service demand in disasters, however this has not occurred systematically to date. Reference Redwood-Campbell and Abrahams6,Reference Desborough, Dykgraaf and Phillips7
General Practitioners, also known as Family Physicians, are generalist medical doctors. In Australia and New Zealand, they undergo specialist training to qualify. They provide first contact, non-referred health care in the community for patients presenting with undifferentiated mental and physical health conditions. They may work in large independent, multidisciplinary group practices, or as solo practitioners. In urban areas, there is limited affiliation of GPs with hospitals. In rural areas, this is more common. Generally, GPs are present in most communities across the country. They diagnose, treat, and manage the full range of acute and chronic medical conditions, as well as providing preventative health care. They function as gatekeepers, triaging and referring to other medical sub-specialists when appropriate, to maintain continuity of care.
In both Australia and New Zealand, GPs are linked through regional primary health care networks. This is a key difference. In Australia, these regional primary care groups have not been included in disaster health management (DHM). This is slowly beginning to change. In New Zealand, these groups have been integrated, particularly in Christchurch during the H1N1 pandemic and the 2010/2011 earthquakes. Another key difference relates to funding. The GPs operate on a fee-for-service model, which is variously contributed to by the patient, the national government in Australia, and the local Primary Health Organization through the District Health Board in New Zealand. In Australia, GPs are not usually funded by the state or local jurisdictions who are responsible for local and state disaster management. In New Zealand, funding for local involvement in DHM has come from regional health organizations responsible for DHM.
The disaster literature identifies that the majority of disaster health care needs in the immediate, short term, and longer term fall within the realm of General Practice. Reference Kohsaka, Endo, Ueda, Namiki and Fukuda8–Reference Greenough, Lappi and Hsu10 These health care needs do not disappear during disasters, rather they intensify. Reference Kohsaka, Endo, Ueda, Namiki and Fukuda8–Reference Lee, Gupta and Carr16 However, in most countries including Australia, GPs are poorly integrated into DHM and are poorly prepared for disasters. Reference Redwood-Campbell and Abrahams6
General Practice has defined roles and responsibilities during inter-disaster periods with established lines of communication and interaction with other components of the health care system, but these become blurred and disconnected during disasters. Disasters create dynamic, difficult, dangerous environments in which people’s lives and well-being are at stake. Reference Ardagh, Richardson and Robinson3,Reference Brackbill, Cone, Farfel and Stellman17 Agencies working together under such conditions need a clear understanding of each other’s roles in order to coordinate optimally. 1 In the absence of clear responsibilities or roles for GPs during disasters, Australian GPs have been formulating their own roles Reference Burns, Douglas, Hu, Aitken and Raphael5 and attempting to build linkages to the broader DHM system. Reference Reay and Burns18,19
Disaster Managers (DMs) are the experts in disaster management, providing coordination of, and support for, the multidisciplinary response seen in disasters through Prevention, Preparedness, Response, and Recovery.
The aim of this study was to explore the role and contributions of GPs in all-hazard DHM from the perspective of DMs and to identify barriers to, and benefits of, more active integration of GPs into disaster health care systems.
Methods
Study Design
This study used semi-structured interviews with a purposive sample of DMs to explore their experiences with GPs during all-hazard disasters from 2009 through 2016 in Australia or New Zealand, including natural, man-made, and pandemic disasters. This research is part of a larger program aiming to identify the roles of GPs within DHM systems which has already interviewed GPs on their perspectives. Reference Burns, Douglas, Hu, Aitken and Raphael5,Reference Burns, Aitken and Raphael20,Reference Burns, Douglas and Hu21
Taking a constructivist approach, the study used an interpretivist theoretical perspective and inductive reasoning to explore the perspectives of the DMs on benefits and challenges of GP contribution to disaster health care and perceived barriers to their inclusion. A qualitative methodology informed by grounded theory was used to guide the research. An iterative process of data collection through semi-structured interviews, data analysis, and thematic categorization was used throughout the research cycles to enable construction of theories. Reference Gray22–Reference Crotty25
Participants
Disaster management professionals with professional exposure to GPs during all-hazard disasters in Australia or New Zealand from 2009 through 2016, including but not limited to the 2009 Victorian bushfires, the 2010/2011 Eastern Australian floods, the 2010/2011 Christchurch earthquakes, the 2013 Blue Mountains bushfires, the 2014 Hazelwood mine fire disaster, the 2014 Lindt Café Siege, and the 2016 Melbourne thunderstorm, were invited to participate.
Disaster Managers have broad oversight of health care arrangements during disasters and contribute to supporting and coordinating health care professionals in provision of care. They are cognizant of the rules of engagement in disasters, and of the roles and responsibilities of all players. Reference McEntire26 No single accepted definition of DM exists. Reference McEntire26,27 This report utilized the US Federal Emergency Management Agency (FEMA; Washington, DC USA) definition of disaster management to define “Disaster Managers” as:
Professionals from a wide-range of cross-disciplinary fields who are involved in “the managerial function charged with creating the framework within which communities reduce vulnerability to hazards and cope with disasters.” 27 (p4)
Recruitment occurred through purposive snowball sampling, aiming to include a diversity of professional backgrounds and experiences to obtain a more comprehensive understanding across different hazards, interactions with GPs, levels of response, community context, and degrees of community impact.
Data Collection and Analysis
All participants were interviewed by the lead author (R1). Open-ended interviews using broad scoping questions were used to elicit a greater understanding of the subject. The questions were developed with reference to the literature and based on the researchers’ experiences working in both GP and DM disciplines, then piloted with two DMs (Appendix A shows interview questions; available online only).
Interviews were audio-recorded and transcribed verbatim, supported by NVivo Version for MAC 11.4.328 (QSR International; Melbourne, Victoria, Australia), which aided coding and thematic development. Transcripts were analyzed and coded by three researchers (R1, R2, R3) to identify emergent themes. Initially, two researchers (R1, R2) analyzed and coded the transcripts as they were conducted, allowing further investigation of emerging theories in subsequent interviews. This continued until data saturation was reached. Once interviews were completed, two of the research team (R1, R3) further analyzed and coded an initial five transcripts together to confirm inter-coder consistency. Subsequent data analysis was conducted separately. Emergent themes were discussed between all researchers iteratively until final theories were confirmed.
Ethics
Ethical approval was obtained from the Australian National University (Canberra, Australian Capital Territory, Australia) Human Research Ethics Committee - Protocol 2013/659. Informed consent was obtained from all participants.
Results
Twenty-nine DMs were interviewed face-to-face (n = 24) or by telephone (n = 5). Total interview duration ranged from 37 to 233 minutes. Participants’ background professions covered ten different professions (Table 1). Twenty-one DM experts interviewed were predominantly employed within government agencies at the local, state, and national level. All participants had professional experience managing disaster health care provision in Australia and/or New Zealand spanning a range of incidents over the last four decades, including heatwaves; bushfires; drought; flooding; major storms, including dust, hail, and thunderstorms; earthquakes; terrorism; environmental and technological incidents; and infectious disease outbreaks including the H1N1 pandemic.
Table 1. Participant Characteristics

GP Contributions to Disaster Health Management
Participants were asked for their overall view on the involvement of GPs in DHM. The majority of participants identified valuable health care contributions from GPs during disasters and expressed a keenness to involve GPs. However, significantly different perspectives were seen between Australian and New Zealand participants regarding the possibility of achieving integration of GPs into existing disaster management systems.
Australian DMs identified significant barriers to inclusion of GPs in disaster management systems, with a number uncertain if integration was achievable. One felt there was no role, however, the majority felt GPs should be included if barriers could be navigated. Conversely, New Zealand DMs unanimously described GPs as already providing essential valuable contributions to disaster health care. Integration of GPs in New Zealand disaster management systems was seen as essential, feasible, and achieved. The key themes from the research are summarized in Table 2.
Table 2. Summary of Key Themes from the Research in Decreasing Frequency of Occurrence
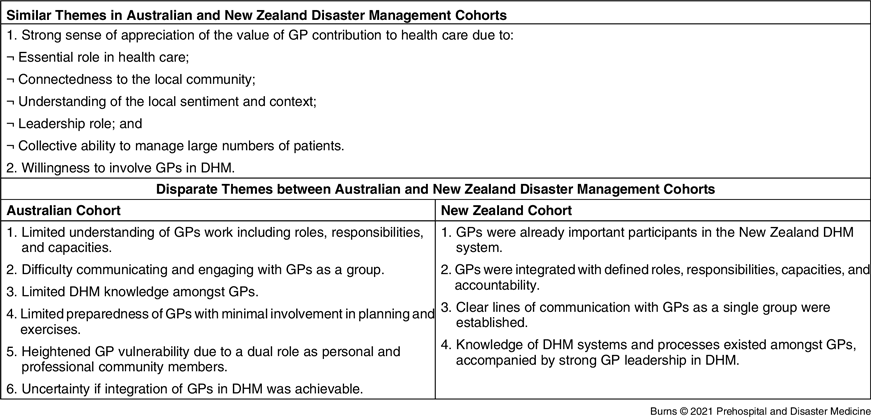
Abbreviations: DHM, disaster health management; GP, general practitioner.
Detailed analysis suggested most Australian and New Zealand DMs felt the value GPs contributed could be ascribed to their essential role in health care, connectedness to the community, leadership, knowledge of the community needs, and collective ability to manage large numbers of patients:
A strong sense of appreciation of GP contribution to health care existed amongst DMs. “Following the earthquake, there were significant areas of the city without the sort of infrastructure that a hospital-based clinician would expect. GPs adapt more easily to that sort of environment than anyone else, so I think they were probably more effective more quickly.” [NZ]
One critical element was GPs connectedness to the local community and their understanding of the local sentiment and context, described by several as the “eyes and ears of the local community”:
The strongest role GPs play is their connectedness to people and community. They have strong linkage locally… They become our eyes and ears… What’s the impact on the community? Which patients might be at greatest risk? They’re the sorts of things the GP knows better than anyone else. [AUS]
This connectedness enhanced their value as community leaders in times of crisis:
…Because the community already knew them, the community listened. If the GP had some advice or a warning… they would listen. It was very different to someone who is part of an emergency response team who comes into town. GPs had this big standing already in the eyes of the community. [AUS]
The GPs’ knowledge of the local people meant knowledge of who might need assistance, the type of assistance, and crucially, how to reach them:
It’s all very well me saying… people who live in that street [need to be] supported. Well, how do I touch that person to make sure they’re supported? The most obvious answer is through the GPs because people go to the doctor when they can’t sleep. [AUS]
They know who their vulnerable patients are, they can provide outreach. [NZ]
The GPs were seen as having the capacity to manage large numbers of patients, particularly regarding continuity of care. This was important in allowing emergency departments (EDs) to continue to manage higher acuity presentations:
…Patient continuity of care really is the GP’s role. [NZ]
Having general practices open released acute facilities to care for acute patients. It meant EDs weren’t blocked… So, it was a godsend. It was very useful. [AUS]
Barriers to GP Inclusion in Australian Disaster Health Management
Perspectives on GP inclusion contrasted significantly between Australian and New Zealand DMs; therefore, they are discussed separately. Australian DMs reported significant, potentially insurmountable barriers to integration. In considering their own impediments, DMs felt they had little understanding of GPs’ work or how to engage with them as a unit. In considering GPs, DMs felt GPs had little DHM knowledge, limited preparedness, and heightened vulnerability (Table 1).
Australian DMs revealed they had little to no understanding of how GPs and their practices functioned, their responsibilities, and capabilities:
What’s missing for us is understanding what a practice is. What is important to the practice and how does a practice work and communicate? [AUS]
The DMs particularly wanted to know how to establish communication channels with GPs as a unified group, something that had not been achievable due to GP membership of diverse General Practice Organizations (GPOs):
I’d say the main obstacle to getting GPs integrated into disaster management is structure. If say I’m a state level player – who do I go to at state level? Who is the coordinator of all the local levels? Who do I need to talk to, to say this is what we want to know? [AUS]
Use of different vernacular in communication between GPs and DMs was highlighted:
Having a GP in our EOC [Emergency Operations Centre] who can connect to a network, who knows the language, who understands the implications, that’s critical because it’s about creating a pathway to be able to speak. [AUS]
Lack of understanding of DHM systems was perceived as a non-negotiable barrier to inclusion, critical for involvement of all agencies working in DHM:
GPs are missing that little bit in the puzzle that sets the core foundations [in disaster management] for them. It doesn’t matter what I think the roles and responsibilities of a GP should be, without the core foundations… I don’t think it would ever successfully work. [AUS]
It certainly was a lot of stress for some people at a very busy time having discussions on the phone with GPs who really weren’t understanding what was going on. [AUS]
Lack of understanding fed into a lack of preparedness with limited involvement in planning or exercising where relationships and trust are built. It was felt ill-advised to be attempting to work with strangers during the chaos of the acute event:
What GPs are not prepared for is the barrage… They don’t understand the system, they don’t understand why all of a sudden I’m saying, I need you to do this. We don’t want to change what it is they do, we just want them to be enabled to do what they do well. [AUS]
There was particular concern about the professional exposure of GPs finding themselves in difficult situations treating patients outside their usual scope of business:
The reality is mistakes happen when you’re out of your space… to protect the GPs… don’t take them out of their usual roles. [AUS]
Similarly, concern was expressed about the capacity of GPs to reliably accommodate a health care surge and excess requests from other responders, potentially disrupting usual patient care and secondarily increasing the pressure on EDs. This culminated in concern for GPs vulnerability due to dual involvement as affected community members and professional health care leaders. Participants observed GPs contributed professionally beyond what was safely sustainable:
The local GPs up there… were all so keen to volunteer, but months down the track, they’re like, this is so draining dealing with emotion continually… The doctors didn’t have to go to excessive hours, 24 hours on call. That has probably been a mistake. [AUS]
Participants noted the lack of established professional disaster support systems for GPs, considered essential amongst other responder groups. However, the same factors that created vulnerability were seen to contribute the greatest value. Stories emerged of GPs stepping up to lead their community as trusted local leaders, assisting the DMs:
I’ve had good involvement with them rurally during floods. We had fantastic GPs there. They were very involved in the communities already. They were well-known. They had been there for some time. They were quite embedded within their communities as community leaders. They were absolutely amazing. [AUS]
Despite significant barriers, the majority of Australian DMs were united in their desire to facilitate inclusion of Australian GPs. Figure 1 outlines the tension between the barriers to, and benefits of, GP inclusion. The DMs suggested that to facilitate inclusion, they needed clarification on:
-
The scope of GPs’ usual business and practice functions;
-
How to engage with GPs as one group;
-
How to communicate clearly with GPs (ie, understand “GP speak”);
-
Specific accountable roles and contributions from GPs in disaster health care; and
-
Support GPs need to provide health care and build capacity during disasters.

Figure 1. Tension Expressed by Australian DMs between Barriers to, and Benefits of, General Practice Inclusion in DHM.
Abbreviations: DM, Disaster Manager; DHM, disaster health management; GP, general practitioner.
The DMs felt GPs needed to develop several standards and processes before DMs felt they could be safely integrated into the overarching DHM system. These included:
-
Routine education, training, and language in DHM;
-
On-going contribution to planning and preparedness committees, including involvement in scenario exercises; and
-
Development of clear definitions of GP capacity, capabilities, and commitment for inclusion in planning documents.
GP Inclusion in New Zealand Disaster Health Management
Four key divergent themes emerged from the perspectives of the New Zealand cohort. The GPs were seen as already important participants in DHM, with clear roles, lines of communication, and knowledge of DHM systems (Table 1). New Zealand GPs were seen as important participants in DHM already included in their DHM system:
We were planning together before the earthquakes, which is why we got through it as well as we did. We’d already built-up relationships…. We had connections, we had trust, we’d developed relationships so you could work alongside each other. And I think if we hadn’t had that, I don’t think we would have done as well. [NZ]
Several New Zealand interviewees discussed the history of New Zealand GP involvement in disasters. As a consequence of the 2003 SARS outbreak in Asia, extensive work had been undertaken in New Zealand to link GPs into the DHM systems. On the southern island of New Zealand, the GP-led Canterbury Primary Response Group (CPRG; Christchurch, New Zealand) was established to meet weekly and incorporate General Practice into emergency planning sessions, policies, and exercises. Local DMs travelled around many General Practices to assist in the development of disaster plans and facilitate GP understanding of roles in DHM as part of a united response. This strong inclusion of GPs was then enacted during the H1N1 pandemic, the two Christchurch earthquakes, the Christchurch Mosque shootings, and subsequently:
When 2009 H1N1 pandemic arrived, the response was led by primary care, so it made a huge difference. All the GPs were engaged and had a strong leadership. [NZ]
Setting up our disaster primary care response hasn’t happened overnight. I’m talking about a 10-year journey. When the earthquake struck us, our systems worked quite well. A lot of people left Christchurch without medications. So, we had a huge problem… We went from a population of 900 overnight to 10,000. All had left without their medications. So, it was a simple call to several nearby GPs who went… and helped the local practice up there cater for the demands. [NZ]
New Zealand DMs considered themselves well-informed on GPs’ roles and capabilities, and conversely felt the GPs they worked with had a good understanding of DHM systems. Some had worked with individual practices to help develop their emergency processes prior to the 2010/2011 earthquakes:
My role with the local District Health Board was the business continuity side of GPs in emergency. I went to the individual practices and helped them write their plans. We got coverage of about 95% of practices. Five out of six Primary Health Organizations coordinate the primary health response okay. They set up their own EOCs and have relationships with GPs and pharmacies. We do a lot of disaster management training with GPs and pharmacies. [NZ]
Clear lines of communication into the DHM systems existed with General Practice as a single group through strong GP leadership within the CPRG:
The [CPRG lead] would’ve told you, in the EOC he had the chart of which practices were open and closed over that first week or two. [NZ]
New Zealand DMs felt the GPs were well-integrated and accountable with defined roles, responsibilities, and capacities:
GPs were part of an integrated health response; visible and accountable. [NZ]
Discussion
This research examined the functions and contributions of GPs during all-hazard disasters, including natural, man-made, and pandemic outbreaks, from the reflection and standpoint of DMs, experts in DHM. Key findings from this research demonstrated most DM participants valued GP health care contributions during disasters and were willing to support GP integration into existing DHM systems. However, before that was considered achievable, GPs needed clearly defined, accountable roles supported by clear lines of authority/responsibility and pathways of communication written into health care plans, as well as an understanding of the same disaster management content required of other disaster responders. In New Zealand, both of these had already been undertaken through strong collaboration and effort between GP and DM leaders over many years, and GPs were considered an integral part of the DHM system.
In Australia, DMs’ assistance towards effective GP integration was hampered by two key issues: (1) difficulty identifying a single point of engagement with GPs and GPOs for planning and practicing for disasters; and (2) the DMs’ limited understanding of the ways GPs work, their scope of practice, and therefore how to support their contribution.
The DMs in both countries recognized GPs’ dual vulnerability from personal and professional exposure to disaster. However, their embeddedness in the disaster-affected community was also seen as enhancing the strength of their contribution: their central role in local health care, leadership, connectedness, and in-depth knowledge of their local community. Bringing GPs into the DHM network and teams, as achieved in New Zealand, rather than leaving them invisible and isolated outside the system, was one way of reducing isolation, risk, and vulnerability.
The New Zealand DM’s perspective that GP integration had been achieved in New Zealand through close collaboration between GPs and DMs was corroborated by the perspectives of New Zealand GPs. Reference Burns, Douglas, Hu, Aitken and Raphael5 In Australia, the Royal Commission into National Natural Disaster Arrangement’s recommendation 15.2 suggested better integration:
Inclusion of primary care in disaster management: Australian, state, and territory governments should develop arrangements that facilitate greater inclusion of primary health care providers in disaster management, including: representation on relevant disaster committees and plans and providing training, education, and other supports. 4
Over a decade earlier, the Review of Australia’s Health Sector Response to Pandemic (H1N1) 2009: Lessons Identified 29 suggested that GPs had not been considered enough in pandemic planning, and that: “structures… in place to liaise with, support, and provide information to GPs were not well-developed.” 29 Progress towards integration of GPs in DHM in Australia fluctuates with the urgency of current disasters; what is required is sustained inclusion of GPs in formal planning and preparedness before the event. Reference Desborough, Dykgraaf and Phillips7 Failure to do so leaves GPs and their patients exposed. Reference Burns and Manderson30
This research contributes to the scant literature available on General Practice in DHM Reference Redwood-Campbell and Abrahams6,Reference Desborough, Dykgraaf and Phillips7,13 and provides a unique perspective through the lens of experts in this field, DMs. The contrast provided between two jurisdictions with differing experiences provides an opportunity to further assess barriers and facilitators. An essential contextual difference is an extra level of governance in Australia. In New Zealand, direct linkage exists between policy at a national level and operational management at a local level. In Australia, GPs operate under a nationally funded framework, while the hospital system is managed at a state level, therein creating an extra layer of difficulty in building an integrated DHM system.
Despite DMs reporting significant obstacles to GP integration in Australia, both cohorts proffered four key principles for greater integration, consolidated by the New Zealand experience.
Firstly, clarifying GPs’ roles, responsibilities, and accountability will build safe, effective involvement in the “Right way, Right place, Right time,” reflective of the DHM mantra. 1 To effect this, collaboration between DMs and GPs will be crucial to clarify GP roles, Reference Burns, Douglas, Hu, Aitken and Raphael5 accountability, interface with other responders, 31 and incorporation into disaster planning and preparedness. Integration of GPs requires not only support and guidance from DMs during planning and preparedness, but strong collaboration during response, when pre-existing relationships, trust, and reliance will be essential. Reference Ardagh, Richardson and Robinson3
Secondly, clarification of communication channels with GPs, in planning, preparing, and responding to disasters is fundamental, existing in New Zealand through the CPRG group. 32 In Australia, this is beginning to occur through local Primary Health Networks, 4 intermittent invitation of GP liaison officers into EOCs, and positions on planning committees at all levels of government.
Thirdly, knowledge of DHM systems and concepts is a basic requirement for all professionals who wish to be involved in DHM. 1 This has yet to become easily available to GPs in Australia, in contrast to New Zealand. Reference Schroeder, Roseveare and Coll33
Finally, safeguarding the well-being of GPs will build resilient local health services themselves that can sustain health care for the community in the years to come.
Strengths and Limitations
One of the strengths of this study is the depth and diversity of experience amongst the 29 DM participants from a range of background professions across different locations in two countries.
The professional status of the lead researcher (R1) as a GP may have skewed sampling and responses offered to those more positively disposed to GP inclusion. However, use of purposive sampling for divergent views and critical inquiry supported the primary researcher’s genuine openness (with lack of preformed opinion) to include a wide-range of views on exclusion or inclusion of GPs in DHM. The use of non-probability sampling in both purposive and snowball sampling, however, has its own disadvantage of sampling bias. The use of purposive sampling creates a potential sampling bias due to participants being more likely to be those reachable or known in some way to the researcher. The use of snowballing creates further sampling bias with potential selection of like-minded participants.
Most of the DMs interviewed worked on the eastern seaboard of Australia and the South Island of New Zealand, although their experience covered more extensive geographical areas nationally and internationally. Transferability to disasters in different geographical regions with differently structured health care systems may therefore be limited. However, there are rich insights from the breadth of experience of these DHM experts.
Implications of Findings for Future Research and Policy
Disaster health service provision by EDs, ambulance, disaster response teams, and hospitals, as well as at a population health level, continues to be evaluated and researched. Disaster health service provision by GPs is rarely included in evaluation and research. To improve GP integration in DHM, evidence of GP disaster health care service contributions during the acute catastrophe and over the longer-term recovery is essential.
Conclusion
The world is contending with increasing frequency and severity of disasters. 34 To manage these challenges requires a resilient health care system that maximizes capacity of all available local health resources, accommodates the surge in demand, and continues to sustain the local health services response in the aftermath. Reference FitzGerald, Capon and Aitken2
It is increasingly apparent that supporting sustained integration of GPs into a more whole-of-health service DHM response is part of the solution. The experience from New Zealand shows it is achievable. The first step is collaboration between DMs and GPs at local, state, and national levels in DHM planning, and practicing before the next disaster event.
Conflicts of interest/funding
Funding for this research was provided by the Royal Australian College of General Practitioners Family Medical Care Education and Research Grant. The authors have no conflicts of interest to declare.
Supplementary Materials
To view supplementary material for this article, please visit https://doi.org/10.1017/S1049023X21001230






