Introduction
Natural disasters (NDs) are calamitous phenomena with different origins, including atmospheric, hydrologic, and geologic. Earthquakes, floods, volcanic eruptions, droughts, landslides, and tsunamis are among important NDs with catastrophic consequences. Reference Watson, Connolly and Gayer1 Due to poor infrastructures and resources, the disastrous effects of these events are more notable in developing countries. The health system preparedness for NDs is not enough to prevent infectious diseases dispersion among inadequately equipped regions. Reference Viswanathan, Chakrabarty and Basu2 In the situation of chaos that follows NDs and the displacement of a large number of people in affecting areas, the potential impact of communicable infections is quite high, and poor living conditions, crowding, inadequate sanitation and water, and difficulty of access to health services increase the risk of infectious diseases transmission in disaster-affected regions. Reference Watson, Connolly and Gayer1,Reference Kouadio, Aljunid and Kamigaki3
Among infectious agents associated with post-disaster conditions, parasitic infections have been considered as the main health-threatening diseases in disaster-affected areas. Reference Kouadio, Aljunid and Kamigaki3–Reference Watson, Gayer and Connolly6 Malaria is a health challenge caused by Plasmodium parasites that are transmitted to people via the bites of infected vector mosquitos. According to World Health Organization (WHO; Geneva, Switzerland), approximately 241 million cases and 627,000 deaths from malaria were reported in 2020.
Leishmaniases is a group of infections with Leishmania parasites transmitted to humans by sand fly vectors throughout the world. Reference Gradoni7 More than one billion people are at risk of infection and more than one million new cases of leishmaniases are reported annually. Reference Gradoni7 The potential impact of NDs on malaria and leishmaniasis frequency and vector population dynamics is usually presumed to be very high in post-disaster conditions. Reference Abdolahnejad, Mousavi and Sofizadeh8–Reference Shortus, Musto and Bugoro10
As a disaster-prone region, out of the 44 types of natural disasters that occur in the world, 33 of them are identified in Iran. During the past decades, the most frequent NDs in Iran were floods, earthquakes, and droughts. Reference Mo11 Although there are several reports on the frequency of malaria and leishmaniases in post-disaster conditions of stricken areas of Iran, Reference Abdolahnejad, Mousavi and Sofizadeh8,Reference Rostamian, Rezaeian and Hamidouche12 the relationship between NDs and the incidents of these infections is not clearly understood. Due to the importance of cutaneous leishmaniasis (CL) and malaria and frequent NDs in Iran, the relationship between them should be evaluated. This study aimed to evaluate the prevalence of malaria and CL before and after earthquakes, floods, and droughts during the past four decades in Iran. The results obtained from this study can provide evidence-based information to authorities to manage these diseases in stricken areas of the country.
Methods
Malaria and CL Data
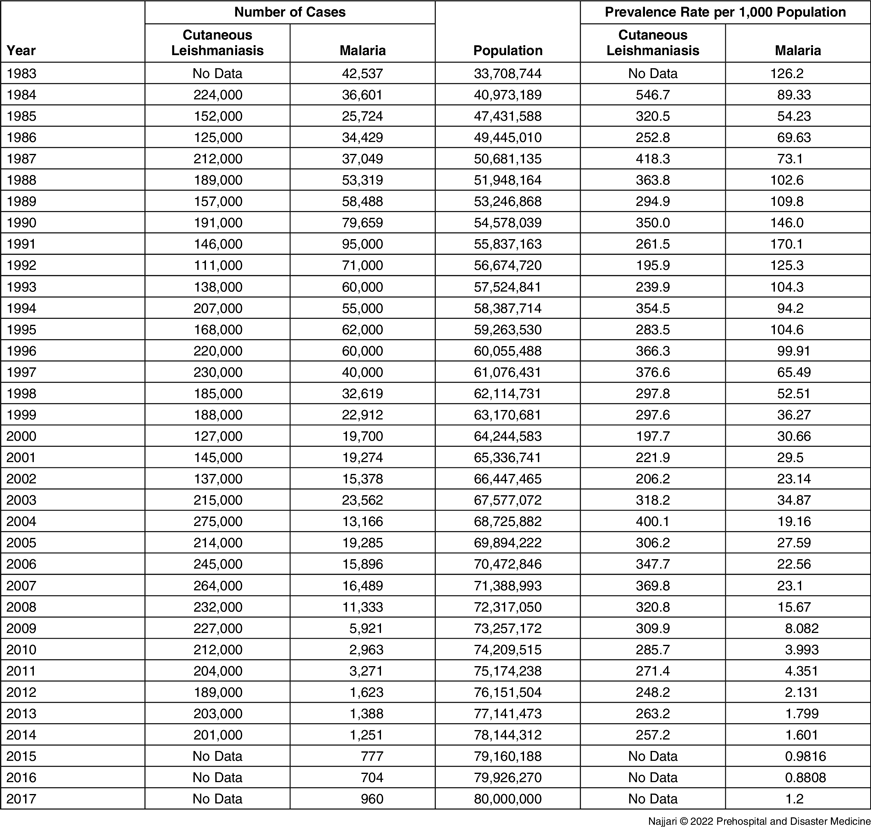
The prevalence of malaria and CL diseases in Iran was considered during the time period from 1983 through 2017. These data were obtained from the reports of the Ministry of Health and Medical Education in Iran (Tehran, Iran) and provincial centers for malaria and CL control (Table 1). For getting a better evaluation, a comprehensive search was done on the literature to find cross-sectional studies which reported the frequency of malaria and CL diseases in Iran for the mentioned years. The data about these infections from review articles, as well as unpublished and academic reports, were also included in the recent study.
Table 1. Main Numerical Data of Cutaneous Leishmaniasis and Malaria in Iran for the Years 1983 through 2017
ND Data
Natural disasters including geological (earthquakes), hydrological (floods), and climatological (droughts) in Iran were the focus in the current study. The list of devastating NDs of Iran was obtained from the Centre for Research on the Epidemiology of Disasters (CRED; Brussels, Belgium) database and the leading humanitarian information source on global crises and disasters, ReliefWeb (United Nations Office for the Coordination of Humanitarian Affairs [OCHA]; New York USA). The data from the National Disaster Management Organization of Iran (NDMO; Tehran, Iran) also was considered. The earthquakes with a magnitude more than 6.0, flash floods, and devastating droughts during the time period from 1983 through 2017 were selected for this study. The frequency occurrence and location of NDs during the mentioned period are depicted in Figure 1.

Figure 1. Spatial Occurrence of Natural Disasters in Iran: (a) Number of Earthquakes with a Magnitude more than 6.0 per Iranian Provinces from 1983 through 2017; (b) Number of Flash Floods per Iranian Provinces from 1983 through 2017.
Data Analysis
In this study, two sources of frequency data (national data and published articles) were used for malaria and CL diseases. The rate of diseases per 100,000 populations was calculated as the number of cases in each year divided by population in that year. The data of the population was obtained from the Population and Housing Censuses of Iran. A total of 35 time points for malaria and 31 time points for CL were used in this study. Interrupted time series analysis with linear regression modeling was used to estimate time trends of mentioned diseases before and after disaster based on the national annual rates. Reference Bernal, Cummins and Gasparrini13 This analysis was done by STATA 14 software (StataCorp; College Station, Texas USA) at 95% confidence level. In addition, Microsoft Excel (Microsoft Corp.; Redmond, Washington USA) was used to draw the trends in the frequency of floods and earthquakes occurrence and diseases rate (CL and malaria rates per 1,000 population) during the studied time period in Iran (Figure 2 and Figure 3).

Figure 2. Trends in Occurrence of Natural Disasters and CL Rate (per 1,000 population) in Iran.
Abbreviation: CL, cutaneous leishmaniasis.

Figure 3. Trends in Occurrence of Natural Disasters and Malaria Rate (per 1,000 population) in Iran.
Results
Description of ND-Malaria Relationship
The time trends of malaria rate per year in the pooled national data by NDs are shown in Figure 4. A similar time trend preceding and after the intervention was found for the disasters droughts and floods (Figures 4a and 4c). For the period preceding the disasters drought and flood, a decreasing time trend was found over time, and during the period after disasters, the time trend continued to decline. There are two time points in Figure 4b. The time trend of malaria rate preceding the 1990 earthquake was stable, a downward trend was found after 1990 disaster until 1997 (β coefficient: −10.7; P = .001), and this declining trend was continued after 1997 disaster (β coefficient: −2.7; P = .001).

Figure 4. The Effects of (a) Drought, (b) Earthquake, and (c) Flood on Malaria Rate per 100,000 Populations in Iran.
Note: The y axis is the malaria rate and the x-axis is the year.
Description of the Relationship between NDs and CL
The time trends of CL rate per year in the pooled national data by NDs are shown in Figure 5. For the period preceding the droughts (Figure 5a), a decreasing time trend was found over time (β coefficient: −5.6; P = .261), and during the period after droughts, a slightly upward trend was found (β coefficient: +1.16; P = .799). Based on the two time points of disaster (two powerful earthquakes in Iran) in Figure 5b, the time trend of CL rate preceding the 1990 earthquake had a declining trend, an upward trend was found after 1990 earthquake until 1999 (β coefficient: +8.7; P = .293), and a slight upward trend also appeared after 1999 earthquake (β coefficient: +0.75; P = .839). A declining trend was found before and after the flood disasters, which was not statistically significant (Figure 5c).

Figure 5. The Effects of (a) Drought, (b) Earthquake, and (c) Flood on CL Rate per 100,000 Populations in Iran.
Note: The y axis is the CL rate and the x-axis is the year.
Abbreviation: CL, cutaneous leishmaniasis.
Discussion
Natural disasters can cause great changes to animal and human habitats, which increase people’s exposure to infectious diseases in disaster-affected areas. Reference Ligon14,Reference Waring and Brown15 Due to displacement and chaos, vector-borne parasitic diseases such as malaria and leishmaniasis are important potential risks for human health in stricken regions. Reference Kaur, Habibullah and Nagaratnam16,Reference Zhang, Lu and Liu17 Populations living in endemic regions for malaria and CL are at risk of outbreaks after potential NDs.
Even though malaria is eliminated in central and northern areas of Iran, it remains an important health problem in the south-eastern tropical regions of the country. Reference Azizi, Davtalab-Esmaeili and Farahbakhsh18–Reference Ebrahimipour, Nateghpour and Hajjaran20 The results of the current study showed a decreasing time trend of malaria cases after earthquakes, floods, and droughts in Iran. One study in China showed due to no indigenous transmission of malaria in Gansu Province, the earthquake had no effect on malaria incidence over three years after that. Reference Zhang, Lu and Liu17 It was in accordance with the results of the current study that no significant relationship between earthquakes and malaria frequency was found. This could be due to the restriction of malaria foci in south-eastern areas of Iran that are far from the epicenter of earthquakes. Reference Azizi, Davtalab-Esmaeili and Farahbakhsh18 The ND-malaria relationship has been evidenced using the Generalized Method of Moment (GMM) model and the impact of total disaster and floods on malaria frequencies examined from 2008 through 2014 for 79 countries. The results demonstrated that NDs significantly increased the rates of malaria cases across the globe. Reference Kaur, Habibullah and Nagaratnam16
Although floods and droughts are continuous disasters in the residual foci of malaria, there were no increases in the total malaria cases in Iran. This showed that strategies for the control and elimination of malaria in Iran have been well done by authorities. Malaria elimination in Iran was started with a national political mandate, inter-sectoral collaboration, and evidence-based studies in 2009. Reference Vatandoost, Raeisi and Saghafipour19 However, in the regions with frequent NDs, public health interventions and massive use of antimalarial drugs caused the development of drug resistance, which can impede malaria eradication. Reference Weinstein, Goff and Skelly21
The most frequent form of leishmaniasis is CL and most cases are reported from Afghanistan, Algeria, Brazil, Colombia, Iran, Iraq, Pakistan, Peru, Syria, Tunisia, and Yemen. Reference Inceboz22 Natural disasters lead to population displacement, poor housing, and environmental changes, which can increase the risk of exposure to vectors of Leishmania parasites. Reference Fakoorziba, Baseri and Eghbal23 In the current study, the frequency of CL throughout Iran in pre- and post-disaster conditions was evaluated. Iran is classified as a highly endemic region for CL, Reference Shirzadi, Esfahania and Mohebalia24 and the occurrence of NDs is a constant threat in the country. Most regions of Iran are prone to earthquakes, and due to long-term global climate change, the possibility of floods is quite high across the country. Global patterns of air circulation within the belt form 30° North to 30° South latitude lines lead to a great deal of sunlight, minimal precipitation, high levels of evaporation, and devastating droughts in the countries in this belt, such as Iran.
The effect of NDs on leishmaniases incidents has been systematically reviewed and the different frequencies of the diseases before and after NDs were compared. The results demonstrated increases in the leishmaniases frequencies in post-disaster conditions, but not robustly, and the authors emphasized that the effects of NDs on leishmaniases needed more meticulous and comprehensive studies. Reference Rostamian, Rezaeian and Hamidouche12
Several studies in Iran have stressed out the frequency of CL after NDs. A significant increase in the number of CL cases and creating new foci of transmission after the Bam Earthquake of 2003 has been indicated in a previous study in Iran. Reference Aflatoonian, Sharifi and Aflatoonian25 The frequency of human CL was compared in pre- and post-disaster situations in the rural town of Zarindasht, Fars Province, Iran. The results demonstrated that the possibility of outbreak of CL is quite high after NDs and the annual incidence of CL increased from 58.6/100,000 to 864.0/100,000 cases before and after the earthquake, respectively. Reference Fakoorziba, Baseri and Eghbal23 Another study in Iran showed that the mean annual incidence of CL increased in the post-earthquake period (from 1.9/1,000 cases before to 7.6/1,000 cases after ND). The results emphasized that in post-earthquake conditions, the propagation of sand flies and subsequently the transmission of CL could be facilitated. Reference Sharifi, Nakhaei and Aflatoonian26 In the current study, the overall prevalence of CL was analyzed before and after NDs in Iran, and despite founding upward and declining trends in the frequency of CL in post-disaster conditions, the differences were not statistically significant. This may be due to prevalence analysis of the entire country instead of the stricken areas. Reference Abdolahnejad, Mousavi and Sofizadeh8
Limitations
Although this study is the first to evaluate the variation of the overall frequency of malaria and CL diseases before and after NDs in Iran, it does have its restrictions. The most important limitations are lack of access to malaria and CL cases for all years and collecting some specialized resources from gray resources, including reports of the Ministry of Health and some government agencies on diseases, as well as some unpublished or academic reports. Considering overall frequency instead of frequency in stricken areas could be another limitation of the current study.
Conclusion
The results of the current study indicated the occurrence of earthquakes, floods, and droughts has no significant effect on the frequency of malaria and CL in Iran. More comprehensive and in-depth investigations are needed to better evaluate the effect of NDs on malaria and CL frequencies.
Conflicts of interest
The authors declare none.









