Introduction
Acute coronary syndrome affects over 600,000 people in the United States each year, and between 25% to 40% of those affected have ST-elevation myocardial infarction (STEMI).Reference O’Gara, Kushner and Ascheim1 Early percutaneous coronary intervention (PCI) to open occluded coronary arteries decreases mortality from STEMI.Reference Brodie, Hansen and Stuckey2-Reference Zijlstra, Hoorntje and de Boer4 Longer time-to-intervention is associated with increased mortality and morbidity.Reference Brodie, Hansen and Stuckey2,Reference Terkelsen, Jensen and Tilsted5-Reference Terkelsen, Sorensen and Maeng7 National campaigns to reduce the time from hospital presentation to reperfusion (ie, door-to-balloon time) have improved this metric.Reference O’Gara, Kushner and Ascheim1,Reference Krumholz, Herrin and Miller8
More recent interventions have been aimed at decreasing total ischemic time for all patients in a regional health care system.Reference O’Gara, Kushner and Ascheim1,Reference Krumholz, Herrin and Miller8 This goal requires the development of regionalized systems for STEMI care, with an emphasis on initial prehospital triage to a PCI-capable hospital.Reference O’Gara, Kushner and Ascheim1 In an effort to further decrease the time from first medical contact to PCI (ie, first-medical-contact-to-balloon time [FMC2B]), EMS systems have developed protocols to facilitate prehospital activation: the mobilization of cardiac catheterization laboratory personnel prior to patient arrival. A study of prehospital cardiac catheterization laboratory activations under the Los Angeles County (LAC; California USA) EMS protocol found that FMC2B time decreased by 14 minutes, on average, compared to activation from the emergency department (ED). Prehospital activation is also associated with improved patient-centered outcomes.Reference Shavadia, Roe and Chen9 However, the LAC protocol change also increased the rate of activation for patients ultimately determined not to have STEMI.Reference Squire, Tamayo-Sarver, Rashi, Koenig and Niemann10
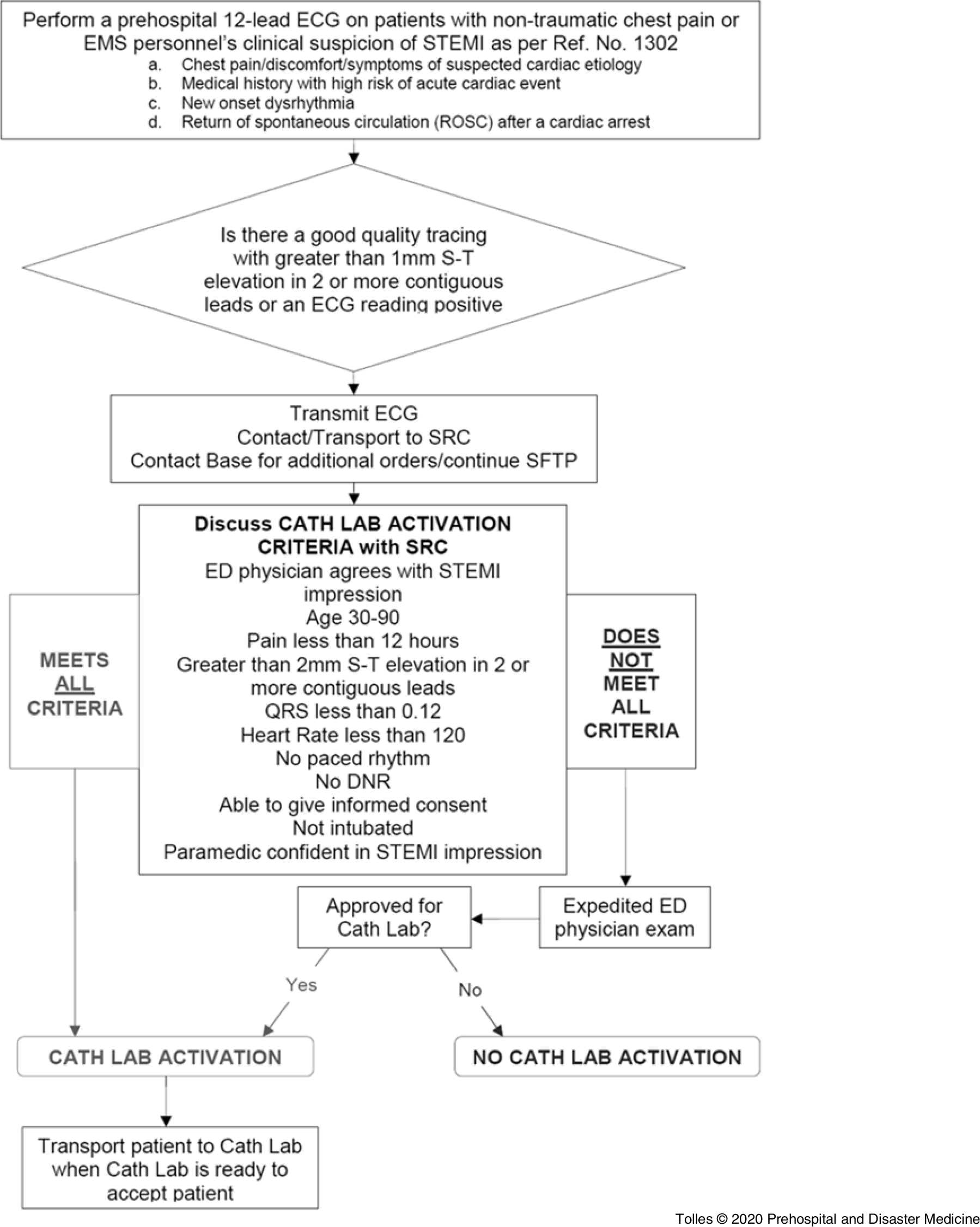
On September 1, 2015, the LAC EMS Agency introduced the American Heart Association (AHA; Dallas, Texas USA) Mission Lifeline PreAct algorithm with the aim of decreasing the rate of “false positive” prehospital activations, defined as activations of the cardiac catheterization laboratory for patients who did not require emergent intervention, thereby increasing the fraction of time that activation of cardiac catheterization laboratory resources resulted in patient benefit (Figure 1). A pre-/post-analysis was conducted to assess the success of this intervention.

Figure 1. Los Angeles County Prehospital STEMI Activation Protocol.
Methods
Study Design
This was an observational study of prospectively collected data compared with historical controls in the pre-intervention period. The study was approved with a waiver of informed consent by the Los Angeles Biomedical Research Institute Institutional Review Board (West Carson, California USA; Protocol Number 30797-01).
Population and Setting
Los Angeles County is a metropolitan area spanning 4,084 square miles with over 10 million inhabitants. The EMS 9-1-1 response is provided by 30 municipal fire departments and one law enforcement agency with over 3,900 licensed paramedics throughout the county. The LAC EMS Agency provides oversight of providers operating within the county, establishes protocols and procedures, and designates specialty care centers. Paramedics in LAC utilize standing treatment protocols for initial management of patients with STEMI and make hospital contact for online medical control and pre-arrival notification.
The LAC EMS Agency established a regionalized cardiac care system in 2006, and today 35 of the 73 9-1-1 receiving hospitals are designated STEMI Receiving Centers (SRCs). These centers are capable of providing immediate coronary angiography and PCI, 24 hours a day, seven days a week.Reference Eckstein, Koenig, Kaji and Tadeo11 All SRCs submit data on patient presentation, in-hospital treatment, and outcomes to the LAC EMS Agency for system quality improvement. Nineteen of the 35 SRCs provide online medical control, meaning they have mobile intensive care nurses (MICNs) who have been trained to provide medical direction to prehospital providers available 24 hours a day. For patients with possible STEMI, based on clinical presentation and with electrocardiographic (ECG) findings, paramedics provide advance notification (STEMI alert) and transport directly to the closest SRC. Indications to perform an ECG in LAC include patient presentation with non-traumatic chest pain, provider suspicion for STEMI, new onset arrhythmia, or return of spontaneous circulation after cardiac arrest.
Prior to 2015, paramedics relied solely on the monitor’s software interpretation of the ECG to identify a possible STEMI. If the software generated the STEMI statement, the paramedics notified online medical control of the ECG findings, relayed the patient’s clinical presentation, and attempted to transmit the ECG for review. If online medical control was not based at the receiving SRC, this information was then reported to the receiving SRC by online medical control. The decision to activate the catheterization laboratory at the SRC was made according to highly variable local policy (eg, some SRCs activated the catheterization laboratory for all STEMI alerts, others involved a physician in the decision). There was no guidance from the LAC EMS Agency regarding when a STEMI alert should be activated.
In 2015, the LAC EMS Agency introduced a prehospital STEMI activation protocol (Figure 1), which was a systems intervention adapted from the AHA Mission Lifeline PreAct algorithm, in order to address the high proportion of STEMI alerts that did not result in emergent coronary angiography due to “false positive” software interpretation.Reference Bosson, Kaji and Niemann12 Since this policy change, paramedics in LAC identify a STEMI in one of two ways: (1) the cardiac monitor’s software algorithm reads ***STEMI*** or manufacturer equivalent; or (2) the paramedic interpretation is STEMI, defined as at least 1mm of ST elevation in two contiguous leads. If one of these two conditions apply, paramedics transmit the acquired ECG and provide advanced notification directly to the receiving SRC, addressing a series of criteria to determine whether field activation of the catheterization lab is appropriate (Figure 1). The final decision to activate the catheterization lab is at the discretion of the receiving ED physician at the SRC.
At its inception, all paramedics and hospital-based EMS medical control personnel received training on the new policy. In addition, all paramedics in LAC received continuing education on STEMI identification. This one-hour didactic educational module reviewed the importance of early STEMI detection, ST-segment identification, and ECG interpretation specific to identification of STEMI. Paramedics continued to use the monitor’s software interpretation to assist. Methods to improve ECG quality and reduce misinterpretations were also reviewed.
There were a variety of cardiac monitors in service in LAC during the study period, according to the various provider agencies, including: Medtronic Lifepak 12 and Medtronic Lifepak 15 (Medtronic; Fridley, Minnesota USA); Philips HeartStart MRX (Philips; Amsterdam, Netherlands); and Zoll “E” and Zoll “X” (Zoll; Chelmsford, Massachusetts USA).
Patient Population
Patients who were transported via EMS to one of the five participating SRCs, and who received an ECG in the field by paramedics that was interpreted by monitor software as STEMI, were included. Patients with STEMI complicated by out-of-hospital cardiac arrest were included. Exclusion criteria were patients with a primary traumatic mechanism, patients <18 years old, those transferred from another acute care facility, and those who did not arrive via EMS. Consecutive patients were collected from the five participating centers starting on March 1, 2016 and ending April 31, 2017. The post-intervention data were compared to historical data from the pre-intervention period abstracted from the LAC SRC database from April 2011 to December 2014, employing the same inclusion and exclusion criteria (see “Data Collection”).
Measurements
The primary goal of the intervention was to increase the positive predictive value (PPV) of activation. A “true positive” was defined as an activation for a subject who underwent PCI or coronary artery bypass graft (CABG) during the index visit. In the PPV calculation, the denominator was all patients who came to the ED via EMS and were found to have possible STEMI on ECG. The numerator was the subset of those patients who underwent PCI or CABG; PCI was defined as intervention via balloon angioplasty or stent placement. “True positive” disease was not defined by activation of the catheterization laboratory alone, because such a definition would be subject to anchoring bias in that the decision to take the patient to catheterization could be influenced by the activation itself. Because troponin data were unavailable for patients in the pre-intervention period, a definition of disease was selected that could be applied uniformly pre- and post-intervention, and captured whether the patient benefitted from the catheterization.
Given the paramedic’s ECG interpretation was not part of the pre-intervention definition of suspected STEMI, the primary analysis was limited to patients whose ECG was positive by software interpretation for STEMI.
Secondary outcomes included FMC2B time for subjects who underwent emergent coronary angiography during their index hospitalization, and measures of protocol adherence to the PreAct algorithm.
Several exploratory analyses of the post-intervention data were planned in advance. The effect of each element of the PreAct algorithm on PPV was analyzed, as well as the change in rate of activation by medical center. Additional data points were collected to facilitate analysis, for the post-intervention subjects only, of the PPV and negative predictive value (NPV) of the decision not to activate the catheterization team for the composite outcome of PCI, troponin elevation, CABG at the index hospitalization, discharge diagnosis of STEMI, or death from a cardiac cause during the index hospitalization.
Data Collection
For the pre-intervention period, author JT abstracted data from the LAC EMS Agency SRC database. Staff at the SRCs abstract the data points for entry into the database from the medical record, including the prehospital care records. Greater than 90% of staff responsible for the data are registered nurses in the departments of emergency medicine, cardiology, and quality improvement. Completeness and accuracy of the entered data are continually reviewed by the LAC EMS Agency Data Management Section, with verification performed during annual site visits. Bi-annual system-wide meetings are held for data review.
In the post-intervention period, MICNs and prehospital care coordinators prospectively recorded data at each of the five sites. Each site entered data into the SRC database as required by LAC EMS standards and, at the same time, entered additional data points necessary to evaluate post-intervention outcomes into a supplementary RedCap database, including: peak troponin value, discharge diagnoses, paramedic interpretation of the ECG (recorded as a binary STEMI/not STEMI), and data regarding ED physician review of ECG and communication with the paramedic.
All data were combined into a single de-identified research database and analyzed using R software for statistical computing (R Foundation for Statistical Computing; Vienna, Austria).13 The FMC2B time was calculated by measuring the time between the timestamp on the first paramedic-performed ECG and the time that the coronary lesion was intervened upon, “balloon time,” in the cardiac catheterization lab. The first ECG timestamp was used as a surrogate for first medical contact time because the time of paramedic arrival on scene was not consistently available for all subjects in pre-intervention period. Further, the ECG timestamp is generated automatically by the software and therefore more likely to be accurate than paramedic self-reported times. Dispatch 9-1-1 call times were not available in the SRC database. Information about whether patients received PCI was abstracted from the SRC database for the pre-intervention period and collected prospectively in the post-intervention period.
Sample Size Calculation and Analytic Methods
A prospective calculation was performed to determine the sample size necessary for a power of .80 to detect what was determined to be a clinically significant change in the PPV of 0.1 (from a pre-intervention baseline of 0.38 to post-intervention 0.48), assuming a Type I error of 0.025, and determined that a sample size of 700 patients with suspected STEMI in each group would yield approximate power of 0.85 with a Type I error of 0.025.
The statistical significance of differences in demographic characteristics were calculated using chi-square tests. The differences between the PPV of cardiac catheterization lab activation and FMC2B time in the pre- and post-intervention periods were compared using a generalized estimating equation (GEE) with a logit link function and an exchangeable correlation structure, which accounted for clustering by hospital, as well as secular trends, and patient age and gender.
For the analysis of FMC2B time, all times greater than four hours were excluded in the statistical analysis because this truncation allowed for a valid statistical analysis relying on the assumption of normally distributed outcomes and also reflects the FMC2B time for patients who went emergently to the catheterization laboratory for suspected STEMI. This resulted in the exclusion of two subjects from the pre-intervention period and two subjects from the post-intervention period.
On review of data at the conclusion of the study, 100 subjects in the SRC database did not have data recorded in the supplementary RedCap database. Because supplementary information (eg, ED physician review of ECG) necessitated collection in real-time for accuracy, it was not possible to reconstruct these data after the fact. A post-hoc sensitivity analysis for the primary outcome was performed, excluding the 41 subjects who had catheterization laboratory activation, but for whom supplementary data were not available such that it could not definitely be determined that the software interpretation of the ECG was STEMI, rather than the paramedic interpretation alone.
Several exploratory analyses on the post-intervention dataset were also performed. The effect of the individual elements of the PreAct algorithm—successful transmission of the ECG, ED physician review of the ECG prior to activation, and ED physician discussion with the paramedic prior to patient arrival—on PPV was assessed using a GEE including the covariates listed above. The PPV for the subset of ECGs that were interpreted as STEMI based on paramedic read alone was calculated. A more liberal criteria for “true positive” was explored by analyzing both the PPV and NPV of activation under the PreAct algorithm for the composite outcome of abnormal troponin, PCI during the initial visit, CABG during the initial visit, discharge diagnosis of STEMI, or death from a cardiac cause during the initial visit.
Results
Data on 3,413 subjects were abstracted from the SRC database for the pre-intervention period and 1,108 subjects for the post-intervention period. After exclusions (Figure 2), 3,642 subjects were included in the study, of whom 2,281 had a cardiac catherization laboratory activation and therefore were included in the primary analysis of the PPV of catheterization laboratory activation. In the exploratory analysis of secondary outcomes, an additional 100 subjects were excluded for missing supplementary data.

Figure 2. CONSORT Diagram.
The demographics of the population of patients with suspected STEMI transported via LAC EMS are shown in Table 1, whereas the demographics of the subset of patients who had catheterization laboratory activation are shown in Table 2. For patients with suspected STEMI, there was an overall decrease in the number of activations of the cardiac catheterization laboratory between the pre- and post-intervention periods (67% versus 49%; 95% CI, -14% to -22%). The rate of cardiac catheterization declined overall between the pre-intervention and post-intervention subjects (34% versus 30%; 95% CI, -7.6% to 0.4%), but actually increased for subjects who had activation (48% versus 58%; 95% CI, 4.6-15.0%). Among subjects who underwent catheterization during their index visit (both those who had laboratory activations and those who didn’t), the proportion with intervenable lesions on PCI or lesions determined to require CABG during the index hospitalization decreased from 26.1% in the pre-intervention period to 24.7% in the post-intervention period (95% CI, -4.8% to 2.0%). However, among subjects who had the catheterization laboratory activated for their care, the proportion with intervenable lesions on PCI or lesions determined to require CABG increased, corresponding to an increase in the PPV.
Table 1. Characteristics of Subjects with Suspected STEMI transported via EMS

Abbreviations: EMS, Emergency Medical Services; SRC, STEMI Receiving Center; STEMI, ST-elevation myocardial infarction.
Table 2. Characteristics of Subjects Analyzed for Primary Outcome (Activated Subjects)

Abbreviations: SRC, STEMI Receiving Center; STEMI, ST-elevation myocardial infarction.
The overall PPV of activation of the cardiac catheterization lab for PCI or CABG during the index visit in the pre-intervention period, averaged across all five hospitals, was 37.9% (95% CI, 36.1%-39.7%). In the post-intervention period, it increased to 48.6% (95% CI, 45.2%-52.0%). This yields an unadjusted odds ratio (OR) of 1.5 (95% CI, 1.2-1.9), corresponding to an unadjusted number needed to treat (NNT) of 9.4 to avoid one inappropriate activation. In this setting, “treatment” is defined as use of the PreAct algorithm compared to standard practice in the pre-intervention period. After correction for secular trends, gender, age, and clustering by hospital, the odds of a “true positive” activation, as defined by the above criteria, increased by a statistically significant amount in the post-intervention period, OR 1.4 (95% CI, 1.1-1.8), although the effect varied substantially between participating medical centers (Figure 3). Applying this adjusted OR to the pre-intervention baseline “true positive” rate of 37.9% yields an adjusted NNT of 12.1. A sensitivity analysis, which excluded an additional 41 patients for whom the ECG monitor software read was not clearly documented as positive in the supplementary database, did not yield qualitatively different results.

Figure 3. Positive Predictive Value of Prehospital Activation Pre- vs Post-Intervention: Overall Odds Ratio and Odds Ratio by Medical Center.
There was substantial heterogeneity between hospitals in their pre-intervention PPV for activation (Supplementary Figure 1; available online only). Post-intervention there was still some heterogeneity, with PPV ranging from 34.6%-76.2% between medical centers, but the degree of variability decreased. The hospital with the highest pre-intervention PPV decreased the PPV of its activations post-intervention, whereas hospitals with low pre-intervention PPV of activation increased. The rate of activation of suspected STEMIs was inversely correlated with the change in a particular hospital’s PPV.
Median FMC2B time was 79 minutes (IQR 66-90 minutes) in the pre-intervention period and 72 minutes (IQR 55-85 minutes) in the post-intervention period for all subjects identified in the field as potential STEMI, including both subjects for whom the cardiac catheterization laboratory was activated from the field and those for whom it was not. After accounting for confounders, there was no significant difference in FMC2B time between the pre-intervention and post-intervention periods (-2.6 minutes—shorter in the pre-intervention period—95% CI, -9.6 to 4.4), although there was heterogeneity between medical centers (Figure 4).

Figure 4. Change in First Medical Contact to Balloon Time: Pre- vs Post-Intervention.
Exploratory Analysis of Secondary Outcomes
While this was a systems intervention that did not require completion of any particular component, an analysis was performed regarding the frequency with which each element of the STEMI prehospital activation protocol was utilized for the 721 subjects for whom supplementary data were available in the post-intervention period. Two hundred sixty-seven subjects (37.0%) had their field ECG successfully transmitted to the hospital, 180 subjects (25.0%) had their field ECG reviewed by an ED physician, and in 38 cases (5.3%), the ED physician and paramedic discussed the case on the radio prior to patient arrival. The PPV of activation was 50.1% (95% CI, 43.0%-57.1%) for cases in which the field ECG was successfully transmitted to the ED, 50.0% (95% CI, 42.7%-57.3%) for cases in which the transmitted field ECG was review by the ED physician, and 76.3% (95% CI, 62.8%-89.9%) for cases in which the ED physician spoke to the paramedic on the radio. However, in a regression analyses accounting for the same covariates as the primary analysis, the OR of “true-positive” activation was not significantly increased by any of the elements of the algorithm (OR associated with ECG transmission 1.3 [95% CI, 0.6-2.8]; OR associated with ECG review 1.3 [95% CI, 0.8-1.9]; OR associated with conversation between the ED physician and paramedic 2.4 [95% CI, 0.9-6.6]).
For the post-intervention subjects, for whom troponin values and discharge diagnoses were available, the positive PPV of activation was evaluated using a more liberal definition of cardiac ischemia, considering an activation to be a “true positive” activation if subjects had an abnormal troponin, PCI during the initial visit, CABG during the initial visit, discharged diagnosis of STEMI, or death from a cardiac cause during the initial hospital admission. Using this definition, the PPV of activation averaged 77.2% across the five medical centers studied and ranged from 67.7% to 100.0%.
The NPV of cardiac catheterization laboratory activation was also explored the using the same, more liberal definition of “true positive.” The overall NPV was 59.5%, (95% CI, 54.6%-63.4%) ranging from 47% to 73% between hospitals. The vast majority of subjects who were counted as “false negatives” (94%) had only an abnormal troponin, whereas the remaining six percent were judged to be “false negative” because they either underwent PCI, had a discharge diagnosis coded as STEMI, or both. The distribution of abnormal troponin values for this population is shown in Supplementary Figure 2 (available online only).
Discussion
The results of this study show an increase in the PPV of prehospital cardiac catheterization laboratory activation for suspected STEMI associated with implementation of AHA’s Mission Lifeline STEMI PreAct algorithm in LAC. Although the study was observational in nature, the analysis accounted for confounders, such as secular trends in the LAC EMS system. The PPV could have potentially been influenced by change in disease prevalence. However, there is no evidence that there was a change in prevalence of acute coronary syndrome requiring intervention in the study population during the period of the study. Nationally, there was a decrease in the incidence of STEMI during the study period.Reference McManus, Gore, Yarzebski, Spencer, Lessard and Goldberg14,Reference Ward, Kripalani and Zhu15
The intervention effect size was modest and the overall post-intervention PPV was still relatively low at 48%. Previously published studies of prehospital activation from other EMS systems report PPVs ranging between 72%-88%.Reference Barnes, Katz and Desmond16,Reference Potter, Matteau and Mansour17 However, their results are not directly comparable to these, because their authors used more liberal and less patient-centered definitions of “true positive” activations, including the composite outcome of cardiac catheterization, or “emergent cardiology evaluation in the ED”Reference Barnes, Katz and Desmond16 or “electrocardiographically appropriate activations.”Reference Potter, Matteau and Mansour17 One possible explanation for the modest effect size is that there were barriers to implementation of the algorithm that were not considered during its development. The algorithm required that an ECG be transmitted by EMS providers, reviewed by an ED physician, and that the ED physician discuss the case with the paramedic prior to patient arrival in the ED. In only a small proportion of cases (5.3%) were all three steps completed.
The first step in the algorithm, after identification of suspected STEMI, was for paramedics to transmit the ECG to the base hospital. In previously published work, the rate of successful ECG transmission in LAC was 28%.Reference Bosson, Kaji and Niemann12 Other systems have reported similar challenges to ECG transmission with success rates as low as 20%.Reference Adams, Abusaid and Lee18 The observed rate of transmission in this study is slightly greater at 37%, but still remains low. This suggests that any algorithm for prehospital activation that relies upon the availability of the ECG for interpretation at the receiving hospital must find a way to address the low rate of successful ECG transmission to receiving facilities. Previously identified barriers to ECG transmission include technical failures, such as failure of the monitor to connect to the wireless network; human error, such as failure of paramedic to select the correct receiving hospital; and protocol noncomplaince.Reference D’Arcy, Bosson and Kaji19 However, efforts directed specifically at improving ECG transmission have been shown to be effective. At a single center in LAC, a quality improvement initiative involving weekly ECG test transmissions resulted in 73% successful ECG transmission at that facility.Reference D’Arcy, Bosson and Kaji19
There are several possible explanations for the low rate of ED physician communication with paramedics. Feedback elicited from participating sites during the study reported that ED physicians found it impractical to take time away from caring for other ED patients to speak to the paramedics on the radio. It is also possible that, in the approximately 45% of cases where the physician reviewed the ECG but did not speak to paramedics, the physician felt that further history would not contribute to the decision to activate.
Overall, improvement in PPV when the LAC EMS adaptation of the PreAct algorithm was prospectively implemented was modest compared to the benefit estimated by retrospective or single-center studies of PreAct and other similar algorithms.Reference Goebel, Vaida, Kahn and Donofrio20,Reference Baran, Lange and Ajoku21 This supports the notion that operational barriers such algorithms must be prospectively explored at multiple sites to understand their real-world effect size.
In this study, the rate of activation decreased after the PreAct algorithm was introduced in the EMS system and the PPV increased, suggesting that the algorithm may have reduced activations for patients less likely to benefit from that activation. Another important effect of the PreAct algorithm was to decrease interfacility variability. The center with the highest pre-intervention PPV actually decreased its PPV as a result of the intervention and increased its overall rate of activation, whereas centers with lower pre-intervention PPV did the opposite. This may suggest that, rather than increasing specificity uniformly, the algorithm effectively increased the standardization of care between centers, at the expense of specificity in the case of one of the participating centers.
The exploratory analysis of the NPV of the decision not to activate the cardiac catheterization laboratory for the composite outcome of abnormal troponin, PCI during the initial visit, CABG during the initial visit, discharge diagnosis of STEMI, or death from a cardiac cause during the initial visit on its face value, appears to be rather low at 59.5%. However, the vast majority of “false negative” decisions judged by these criteria were due to an abnormal troponin only, which can be seen in many conditions for which emergent coronary angiography is not indicated, such as sepsis, hypertensive emergency, myocarditis, or NSTEMI. Overall, this result suggests the sensitivity of the decision to activate the catheterization laboratory for emergent indications is high.
Limitations
This study has several limitations. It is an observational study of a single urban EMS system. The protocol studied here adapted the PreAct algorithm as originally conceived by Mission Lifeline, modifying it to meet the needs of the LAC EMS system, and thus the results may not be generalizable to implementations in other EMS systems. In fact, the Mission Lifeline continued to update their algorithm after the initiation of this study (Supplemental Figure 3; available online only).
The limitation of using PPV as the primary outcome is that it is influenced prevalence, which was not directly measured. Additionally, this study could not address sensitivity and specificity. Although the analysis controlled for known confounders and clustering by hospital in the analysis for the primary outcome, it is possible that there were unmeasured confounders that influenced subject outcomes. Given the observed variability between the five medical centers studied, it is possible that the results would have been different if more medical centers in the EMS system had been analyzed.
The STEMI-detection algorithms associated with the monitors used by provider agencies that transported the vast majority of patients in this study changed between the pre-intervention period and the post-intervention period, primarily from the Marquette GE 12SL algorithm (associated with the Zoll “E” series and the Lifepak 12) to the Inovise 12L algorithm (Zoll “X” series) or the Glasgow algorithm (Lifepak 15). However, both new algorithms increased sensitivity over Marquette 12SL while maintaining the same specificity.Reference Sanko, Eckstein and Bosson22,23 The likely effect of this change would have been to decrease PPV, rather than to increase it.
The definition of “true positive” in activations of the catheterization laboratory has been variable in the literature and was the subject of extensive discussion among the authors. Because troponin values were not available for the pre-intervention population and because an elevated troponin is controversial as an indication for emergent revascularization, this study included only the PCI or CABG in its definition of “true positive.” This study did not attempt to distinguish between PCI of culprit versus bystander lesions. Limited clinical trial data suggest that bystander PCI may be associated with a decrease in major adverse cardiac events.Reference Gershlick, Khan and Kelly24,Reference Wald, Morris and Wald25
For 100 subjects in total, supplementary data were not available, and thus it cannot be determined with certainty that their ECGs were interpreted by the software as a STEMI, rather than by paramedic interpretation alone. However, data collection for the study as a whole captured only 87 patients whose ECG was recorded as positive by paramedic read alone (and these were excluded from the primary analysis) versus 721 who were documented as positive by software read. Thus, it is unlikely that a significant fraction of the missing supplementary data was not interpreted by the software as potential STEMI.
This observational, pragmatic study was not designed to assess the value of the individual criteria included in the PreAct algorithm. Although this study found that the algorithm increased PPV, the algorithm was implemented as a bundle, meaning that this investigation cannot identify which elements were responsible for this improvement. Rather, the results reflect the real-world effect size under the “intention to treat” principle.
Regarding the secondary outcome of FMC2B time, there are several limitations. First, the study was conducted in an urban/suburban setting with short transport times and is unlikely to be applicable to rural settings. The decision was made to truncate the FMC2B analysis at four hours, which allowed for a valid statistical analysis but runs a small risk that patients, for whom the intervention was responsible for a prolonged delay in cardiac catheterization, were ignored. However, only four patients were excluded from the FMC2B analysis for this reason. The ECG timestamp was used to estimate the first medical contact time rather than time of the 9-1-1 call, because linked 9-1-1 data were not available. This may have caused systematic under-estimation of FMC2B times, although the metric was consistent between the pre-intervention and post-intervention periods.
Conclusions
After implementation of the PreAct STEMI algorithm in LAC, the average PPV of field cardiac catheterization lab activation for PCI completion increased at the five medical designated SRCs studied, without a significant change in FMC2B time in the post-implementation period.
Acknowledgements
The authors would like to acknowledge Victoria Barbara, Alina Candal, Kristina Crews, Yvonne Elizarraraz, Jose Garcia, David Hildebrandt, Sandra Jaquez, Dawn Marie Kay, Vivienne Kimmel, Shelly Martin, Laurie Mejia, Effie Pappas-Block, Paula Rosenfield, and Samantha Verga-Gates for their work on protocol implementation and data collection.
Conflicts of interest/disclosures
Michael Gunderson was employed by the American Heart Association (AHA) during the development of the study design. He is currently a consultant for the American College of Cardiology, Pulsara, and Revidus. Timothy Henry and William French served as uncompensated consultants on the AHA Mission Lifeline committee.
Supplementary Material
To view supplementary material for this article, please visit https://doi.org/10.1017/S1049023X20000606