Introduction
Management of Multiple Casualty Events (MCE) requires organized mobilization of both prehospital and hospital-based medical systems.Reference Turégano-Fuentes, Pérez-Diaz and Sanz-Sánchez1-Reference Frykberg and Tepas10 The most important aspect of such a response pertains to the care of the critical and moderately injured, whose care is consequential and time-limited.Reference de Boer and Van Remmen11, Reference de Boer12 To date, the disaster medicine literature lacks a comprehensive model for MCE that quantifies acute medical disasters while accounting for both prehospital and hospital-based acute medical systems.Reference Rutherford13-23 The task of quantifying “acute medical disasters” has proven to be challenging for many authors and experts for many years. In 1989, de Boer et al proposed a quantitative model to evaluate the acute medical consequences of events and categorized MCE into medical “disasters” or “incidents.”Reference de Boer, Brismar and Eldar24 Three parameters were proposed: (1) the casualty load (N) defined as the total number of critical and moderate casualties; (2) the severity factor (S) calculated by dividing the critical and moderate injuries by the number of minor injuries; and (3) the total capacity of the medical services (C) defined as the total number of critical and moderate casualties that can be cared for by designated hospitals within eight hours. De Boer et al argued that if (N × S) / C>1, the event is categorized as a “disaster,” and if (N × S) / C ≤ 1, the event is categorized as an “incident.” This model has not been adopted widely by the disaster medicine community, as it faces two major challenges. The first major conceptual shortcoming is that when calculating the total capacity of medical services, de Boer et al accounted only for the hospital component, and did not include the prehospital component, which is an integral part of the total medical capacity in MCE.Reference Newgard, Sears and Rea25-Reference Doyle36 Second, multiplying the casualty load (N) by the severity factor (S) systematically biased the results. This study proposes a major revision to de Boer's model to quantify acute medical disasters by taking into account recent disaster metrics quantitative models proposed by Bayram et al for hospital surge capacity and prehospital medical response in MCE.Reference Bayram, Zuabi and Subbarao37, Reference Bayram and Zuabi38
There is a need for a comprehensive quantitative model for MCE that accounts for both prehospital and hospital-based acute medical systems, and can lead to the quantification of acute medical disasters. Such a proposed model has to be flexible enough in its application to accommodate a priori estimation as part of the decision-making process and a posteriori evaluation for total quality management purposes.
Methods
For each component of the proposed model, a two-step approach was adopted in the methodology. An extensive literature search was performed, followed by mathematical modeling. A literature review of MEDLINE, EMBASE, and CINAHL from 1950 through August 2010 was conducted to identify articles of interest using the following search terms individually and in various combinations: “disaster,” “quantification,” “model,” “trauma,” “multiple casualty,” and “management.” MCE-related studies on quantification of acute medical disasters were identified, with an attention to trauma-related literature. The work of de Boer et al on a medical severity indexReference de Boer, Brismar and Eldar24 and Bayram et al's disaster metrics illustration of hospital surge capacity and prehospital medical responseReference Bayram, Zuabi and Subbarao37, Reference Bayram and Zuabi38 were used as conceptual frameworks for this proposed model. Preliminary validation was achieved by retrospective application of the model to actual events. The North Atlantic Treaty Organization (NATO) triage categories for trauma patients [T1 (critical), T2 (moderate), T3 (minor), T4 (expectant)] were used for modeling simplicity.Reference de Boer and Van Remmen11, Reference de Boer12 Both T3 and T4 were excluded from the model in this study.
Results
Two complementary components of the medical system pertaining to the acute care of critical and moderately injured MCE victims were identified and modeled. These two components represent the hospital and the prehospital medical systems. The quantitative values of these components were used to propose a comprehensive taxonomy model to quantify the acute medical impact of multiple casualty events.
Hospital-Based Model Component in MCE
The hospital-based component of our proposed model was expressed as the Hospital Acute Care Surge Capacity (HACSC) defined by Bayram et alReference Bayram, Zuabi and Subbarao37 as the maximum number of critical and moderate casualties that a hospital can adequately care for per hour after recruiting all possible additional medical assets, and above which the quality of care decays and becomes inadequate, even with the recruitment of more assets. The HACSC in trauma-related MCE was quantitatively benchmarked by Bayram et al to be equal to the number of Emergency Department Beds (#EDB) divided by the Emergency Department Time (EDT): HACSC = #EBD/EDT. In trauma-related MCE, EDT was estimated to be 2.5, which is the average ED time (in hours) for both T1 and T2 combined.Reference Bayram, Zuabi and Subbarao37
Prehospital Model Component in MCE
The prehospital component of our proposed model was expressed as the medical rescue factor (R), as modeled by Bayram and Zuabi.Reference Bayram and Zuabi38 R incorporates two parameters: the Time Factor (TF) and the Capacity Factor (CF).Reference Bayram and Zuabi38 The TF was defined as the proportion of critical and moderate patients with Injury to Hospital Interval under the Maximum Time Allowed for that level of acuity, as described in current literature. The benchmark for TF was set at 1, which is also the maximum possible value.Reference Bayram and Zuabi38 The CF was defined as the proportion of T1 and T2 patients received by the designated hospitals without exceeding the per-hour hospital surge capacity (HACSC), compared to the total number of T1 and T2 received by all hospitals. The benchmark for CF was also set at 1, which is also the maximum possible value.Reference Bayram and Zuabi38 The medical rescue factor was estimated by multiplying TF by CF (R = TF × CF) and a numerical value of R = 1 was set as the quantitative benchmark.
Acute Medical Severity Index Model
In order to quantify acute medical disasters, both the prehospital quantitative parameter (R) and the hospital-based quantitative parameter (HACSC) were integrated and incorporated in the final model. The Acute Medical Severity Index (AMSI) is a proposed quantitative parameter that compares the Acute Medical Burden (AMB) generated by the MCE to the Total Medical Capacity (TMC) of the community affected to care for the critical and moderately injured patients. The AMSI is a major revision of de Boer's model described above.Reference de Boer, Brismar and Eldar24
Acute Medical Burden (AMB)
The AMB is the total number of critical and moderate casualties (T1 + T2) generated by the MCE (AMB = T1 + T2). AMB ranges theoretically between 0 and infinity. Note that both T3 (minor) and T4 (expectant) are excluded when calculating the AMB.
Quantitative Modeling of the Total Medical Capacity (TMC)
The Total Medical Capacity (TMC) of the community affected is a function of both the prehospital medical response and the total hospital-based capacity. Numerically, the TMC is modeled as the product of the Total Hospital Capacity (THC) and the medical rescue factor (R):
This methodology of multiplying the THC by R, where R has a maximum value of 1, allows for the weakest link in the medical system to be the rate-limiting step in the model. For example, if the prehospital medical system responds in a very robust manner (i.e., R reaches its benchmark of 1), the Total Medical Capacity would then depend on the Total Hospital Capacity. The lowest value of the TMC by default is set at 1.
Total Hospital Capacity (THC)
The Total Hospital Capacity (THC) represents the hospital-based medical capacity of all designated hospitals to care for critical and moderate patients. THC is equal to the sum of individual Hospital Acute Care Surge Capacity (HACSCi)Reference Bayram, Zuabi and Subbarao37 receiving T1 or T2, multiplied by the number of hours (hi) during which those patients are received by each hospital:
In modeling the THC for trauma-related MCE, and based on the Bayram et al quantitative model of HACSC, the THC = [∑(#EDBi / EDT) × hi],Reference Bayram, Zuabi and Subbarao37 where #EDB is the number of ED beds and EDT is the Emergency Department Time (estimated in trauma-related MCE to be 2.5 hours).
Final Quantitative Modeling of the Acute Medical Severity Index (AMSI)
The Acute Medical Severity Index (AMSI) is directly proportional to the AMB and inversely proportional to the TMC. Substituting the values of AMB and TMC modeled above results in the final quantitative model of AMSI:
Discussion
Quantification and definition of acute medical disasters has been a daunting task in the field of disaster medicine.Reference Rutherford13-Reference de Boer, Brismar and Eldar24 The proposed model described above leads to a specific definition of acute medical disasters that is both qualitative and quantitative. Qualitatively, acute medical disaster is defined as a state after a Multiple Casualty Event where the Acute Medical Burden (AMB) exceeds the Total Medical Capacity (TMC) of the community affected (AMB / TMC > 1). Since AMSI = AMB / TMC, the higher the AMB or the lower the TMC, the higher the AMSI would be.
New Taxonomy Model for the Quantification of Acute Medical Disaster, Crisis, Emergency, and Incident
The authors propose the following new taxonomy model to quantitatively categorize MCE. If the AMB > TMC (AMSI > 1), the medical system cannot cope with the acute medical consequences of the event in spite of medical surge, and the situation is classified as an acute medical disaster. If AMB ≤ TMC (AMSI ≤ 1), the medical system can cope with the acute medical consequences of the MCE and the situation is not classified as an acute medical disaster. If AMSI <0.9 and the surge capacity (hospital or prehospital) is not utilized, the situation is an acute medical incident. If AMSI <0.9 and the surge capacity (hospital or prehospital) is actually utilized, the situation becomes an acute medical emergency. If AMSI is between 0.9 and 1, the medical system is critically strained, and the situation is classified as an acute medical crisis (pre-disaster) (Figure 1).
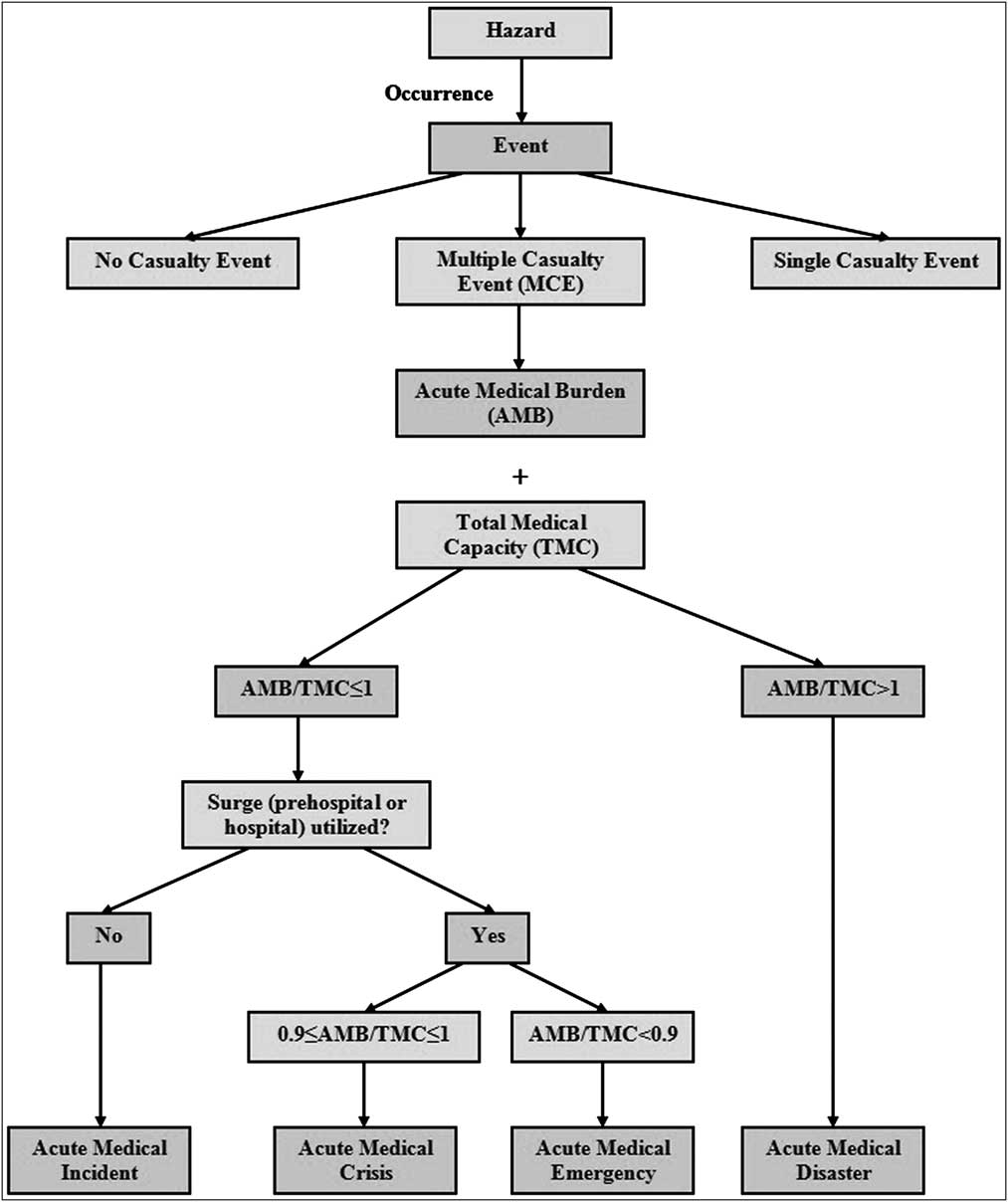
Figure 1 Categorization of the Acute Medical Severity Index
Expected (a priori) vs. Observed (a posteriori)
It is important to highlight the applications of AMSI in both the expected (during an MCE) and observed (after an MCE) settings. If the objective is to predict a priori (shortly after the occurrence of an MCE) whether the expected Total Medical Capacity (TMC) can adequately cope with the “preliminary” Acute Medical Burden (AMB) for the purpose of deciding whether to recruit more resources (hospital and prehospital), the expected values of AMB and TMC would be applied to the AMSI model. If the objective is to evaluate how the Total Medical Capacity (TMC) functioned a posteriori (after the conclusion of an MCE) in response to the Acute Medical Burden (AMB) for total quality management purposes,Reference Donabedian39 the observed AMB and TMC would be applied to the AMSI model.
Applying the Enschede MCE to the Proposed Model
On May 13, 2000, an MCE occurred in the town of Enschede (the Netherlands), where a fireworks warehouse exploded.Reference de Boer and Debacker40 In total, there were 947 casualties, of which 11 were triaged as T1 and 63 as T2 (AMB = 11 + 63 = 74). It was reported that the ambulance response in the first hour was uncoordinated and unrecorded. Hence, it is reasonable to estimate that the value of R was suboptimal (R = 0.9). According to authorities in the Netherlands, five hospitals with a cumulative bed capacity of approximately 2,493 beds received all T1 and T2. Assuming the cumulative number of ED beds in the five hospitals was approximately 191, and that all five hospitals actually received patients over four hours, then the observed THC would have been ∑HACSCi × 4 = [(∑(#EDBi / 2.5) × 4] = [(191 / 2.5) × 4] = 305. Hence, the observed AMSI can be calculated a posteriori to evaluate and categorize the Enschede MCE; AMSI = (74) / [(305) × 0.9] ≈ 74 / 274 ≈ 0.27 (<1) which means that the Total Medical Capacity was higher than the Acute Medical Burden generated by the MCE, and the event would be categorized as an acute medical “incident.” A priori, assuming the initial reports indicated the AMB is about 143 (T1 + T2), and since the expected period of time during which patients arrive to hospitals is six hours,Reference Greenberg and Hendrickson41 the expected THC (for T1 and T2) of all five hospitals would be equal to (191 / 2.5) × 6 = 458. In addition, since the R in urban Netherlands is expected to be 1 (benchmark), the expected AMSI = [143 / (458 × 1)] = 0.3 and hence the expected MCE would also be an acute medical “incident.” This is critical in deciding whether to recruit hospital and prehospital services. If the expected AMB is more than 458, more hospitals need to be designated to receive patients. If there are expected complex search and rescue, extrication, or decontamination efforts by the prehospital systems (e.g., expected R = 0.7), more resources related to the delaying factors, along with even more ambulances, are required to participate in the prehospital response.
Turning an Expected “Incident” into an Observed “Disaster”
Using the example above, consider a different scenario where all of the 74 casualties (T1 + T2) were actually taken to the two closest hospitals (theoretical hospitals A and B with HACSC of 10 and 6 respectively), instead of being distributed among all five hospitals. If 44 (T1 + T2) were taken to hospital A over 4 hours, and 30 (T1 + T2) were taken to hospital B over 3 hours, the observed THC would be equal to (10 × 4) + (6 × 3) = 40 + 18 = 58. The THC has been reduced dramatically from 458 to 58 because all patients were taken to only two hospitals instead of five. Since the HACSC was exceeded in both hospitals, the CF is now 0.82 (61/74). So assuming the TF was 0.9, the R in this scenario would be 0.9 × 0.82 = 0.74. In this case, AMSI = (74) / [(58) × 0.74] ≈ 74 / 43 ≈ 1.7. This example illustrates a situation that was expected to be an acute medical incident, and not to pose a burden on the medical system, that was turned into an actual acute medical disaster by not distributing the patients among the five available hospitals and exceeding the HACSC in both hospitals receiving patients (Table 1).
Table 1 Comparative scenarios on categorization of MCE through AMSI modeling

Strengths and Limitations of the Proposed Model
There are several major strengths of the newly-described, comprehensive model. First, it accounts for both the prehospital medical response, by incorporating the newly described medical rescue factor (R), and the hospital-based medical response, by incorporating the cumulative Hospital Acute Care Surge Capacities (HACSC). Second, it allows for the weakest link (hospital or prehospital) to determine the Total Medical Capacity, which is calculated as TMC = THC × R with the maximum value of R = 1. Third, it allows for a new taxonomy of MCE by comparing the Acute Medical Burden to the Total Medical Capacity to categorize the acute medical consequences of trauma-related MCE. Fourth, it allows both a posteriori evaluation of model components for total quality management purposes (observed AMB, THC, and R) and a priori estimation of parameters as part of the decision-making process (expected AMB, THC, and R). Fifth, this model maybe applied to non-traumatic MCE once the Maximum Times allowed for T1 and T2 (MTA1 and MTA2) and the Hospital Acute Care Surge Capacities (HASC) are established.
There are several limitations to the proposed AMSI model, mostly related to the estimation of its components Hospital Acute Care Surge Capacity (HACSC) and medical rescue factor (R). Predication and measurement of the AMSI components (R, Total Hospital Capacity) are not yet standard practices, and information regarding these parameters may not be readily available in complex events or may be difficult to collect.
Conclusion
A new quantitative taxonomy model for trauma-related MCE has been proposed, quantifying acute medical disasters and differentiating them from acute medical crises, emergencies, and incidents. This model includes both the hospital-based and prehospital medical systems in estimating the Total Medical Capacity to care for the critically and moderately injured. Prospective applications of various components of this model are needed to further verify its applicability and validity, through simulation studies and during actual Multiple Casualty Events.
Abbreviations
- AMB:
Acute Medical Burden
- AMSI:
Acute Medical Severity Index
- ED:
Emergency Department
- EDB:
Emergency Department Beds
- EDT:
Emergency Department Time
- HACSC:
Hospital Acute Care Surge Capacity
- IHI:
Injury to Hospital Interval
- MCE:
Multiple Casualty Events
- MTA:
Maximum Time Allowed
- R:
medical rescue factor
- THC:
Total Hospital Capacity
- TMC:
Total Medical Capacity
Acknowledgments
The authors would like to acknowledge Professor Jan de Boer for his pioneering work; Michel Debacker, Kobi Peleg, Italo Subbarao, and Jomana Musmar for their editing efforts; and Ahmad Bayram for his technical assistance.




