Introduction
In the United States, the geriatric population represents an expanding proportion of patients within the healthcare system. Currently, adults older than 65 years constitute approximately 12% of the US population and it is estimated that by 2020, this age group will account for >16% of the population.1 Geriatric patients also comprise a significant number of patients suffering severe trauma-induced injuries. From 2002–2006, 18.6% of trauma patients in the National Trauma Data Bank (NTDB) were ≥65 years of age.Reference Clark and Fantus2
Elderly patients have several distinct characteristics from other trauma victims. Geriatric patients have different mechanisms of injury, with falls making up a large proportion of severe trauma.3 The number of co-morbidities generally is higher in the geriatric population, and this appears to contribute directly to poorer outcomes.Reference Morris, MacKenzie, Damiano and Bass4–Reference Milzman, Boulanger, Rodriguez, Soderstrom, Mitchell and Magnant6 Associated with the high rate of co-morbidities is the increased use of multiple pharmaceutical agents.Reference Fulton and Allen7,Reference Ballentine8 Of great significance is the increased rates of anti-platelet medications (aspirin or clopidogrel) and anticoagulants (warfarin). These agents have a direct impact on mortality in victims of trauma.Reference Pieracci, Eachempati, Shou, Hydo and Barie9,Reference Mina, Knipfer, Park, Bair, Howells and Bendick10 Finally, when compared to other adult patients with a similar spectrum of injuries, elders have higher morbidity and mortality.Reference Perdue, Watts, Kaufmann and Trask11,Reference Smith, Enderson and Maull12 While geriatric patients make up only 18.6% of the trauma population, they account for 28% of trauma deaths in the US and consume approximately 1/3 of healthcare dollars spent on trauma.Reference Lonner and Koval13,Reference Mueller and Gibson14
The American College of Surgeons (ACS) has recognized that the threshold for transporting patients to a trauma center must be lower for older populations.15 Studies have suggested, however, that standard ACS criteria do not accurately triage older patients for transport to a trauma center.Reference Phillips, Rond, Kelly and Swartz16,Reference Chang, Bass, Cornwell and MacKenzie17 In fact, a significant number of older adult trauma patients die outside of trauma centers.Reference Ma, MacKenzie, Alcorta and Kelen18 Unfortunately, there have been no previously published efforts to develop geriatric-specific triage transport criteria that might reduce under-triage and improve geriatric patient outcomes. This paper describes the development of geriatric-specific field destination criteria for the state of Ohio.
Methods
The Ohio Department of Public Safety's (ODPS) Trauma Committee consists of 24 members who are appointed by the Director of the ODPS and serve under the authority of the Ohio EMS Board within the Department of Public Safety as defined in Ohio Revised Code 4765.04. Among the Board's statutory responsibilities is the development of statewide trauma triage criteria (Table 1). In addition, the law mandates that the Board periodically review the triage criteria to assure that it “minimizes overtriage and undertriage, and emphasizes the special needs of pediatric and geriatric trauma patients.”
Table 1 Current Ohio trauma triage criteria for adults age 16–59 years (Ohio Administrative Code 4765-14-02)

As part of the most recent review of existing criteria, the Trauma Committee was asked to consider whether development of geriatric-specific criteria was necessary. A task force was established to evaluate the need for geriatric-specific criteria and if needed, to determine the appropriate criteria. The task force was to bring recommendations for modification back to the full Committee for consideration.
A literature search was conducted by the members of the Task Force on all relevant literature between 1966 and 2005 to determine if geriatric-specific criteria either were suggested or validated in previous studies to identify potential criteria at variance from those currently in use in Ohio. The following databases were utilized: (1) PubMed; (2) Ovid Medline; (3) NINAHL, Cochrane Database of Systematic Reviews; and (4) the reference sections from each of the relevant articles. Search term “geriatric”, “elderly”, “trauma”, and “triage” initially were used. The broad time period was used to identify potential risk factors for further investigation. These risk factors were validated in a population of the Ohio Trauma Registry from the past decade. Thus, articles that were no longer applicable were not included in the new guidelines. Several studies from 1992 to the present identified potential field triage criteria for geriatric patients.6,16,19–26
Review of Empiric Studies
The Task Force started with an investigation to address the appropriate age defining “geriatric” trauma patients. A comprehensive review of the literature showed that various authors
have defined the threshold for “elderly” as between 45 to 80 years of age.Reference Jacobs, Plaisier, Barie, Hammond, Holevar, Sinclair, Scalea and Wahl27 For example, in an analysis of the Major Trauma Outcome Study (MTOS) database from the 1980s, Finelli et al found that mortality began to rise in patients >45 years of age. Reference Finelli, Jonsson, Champion, Morelli and Fouty28 An analysis of more recent data in the Ohio Trauma Registry indicated that for all ranges of injury severity score (ISS), mortality rose abruptly at 72 years of age. This was confirmed in a separate analysis of Ohio's trauma data.Reference Caterino, Valasek and Werman29 For practical considerations and based on these published data, the Task Force chose to define geriatric trauma patients as those ≥70 years of age.
Several studies identified potential criteria associated with an increased risk of mortality and morbidity among geriatric trauma victims. Milzman et al examined patients admitted to a statewide Level-1 Trauma Center who survived the first 24 hours.Reference Milzman, Boulanger, Rodriguez, Soderstrom, Mitchell and Magnant6 The authors found that the presence of pre-existing medical conditions (cardiovascular disease, diabetes, liver disease, kidney disease, malignancy, pulmonary disease, neurologic disease, and obesity) was an independent predictor of increased mortality risk, and that the magnitude of the risk was related directly to the number of underlying medical conditions. Moreover, patients 65–74 years had an 8-fold increase in mortality with any underlying disease, and those ≥75 years of age experienced a 12-fold increase in mortality compared to younger patients. McGwin et al also showed an association between co-existing medical conditions and increased mortality risk, but noted that the effect decreased as injury severity increased in elderly patients.Reference McGwin, MacLennan, Bailey, Davis and III23
Phillips et al analyzed a statewide trauma registry to determine under-triage and over-triage rates for elderly patients (age >55 years) using state-mandated trauma triage criteria.Reference Phillips, Rond, Kelly and Swartz16 They found an overall under-triage rate of 71%, and that isolated falls had an under-triage rate of 94.3%. They suggested that falls be specifically considered in the triage of the geriatric trauma patient. Champion et al reviewed data in the MTOS database in order to define differences in patients >65 years of age.Reference Champion, Copes, Buyer, Flanagan, Bain and Sacco19 Their findings emphasized the importance of falls, pedestrians struck, and gun violence in the geriatric population. They found a high number of unexpected deaths among this population, and suggested development of age-specific criteria for elderly trauma patients.
Tornetta et al studied injured patients >60 years of age admitted to four Level-I Trauma Centers.Reference Tornetta, Mostafavi, Riina, Turen, Reimer, Levine, Behrens, Geller, Ritter and Homel20 They found that Glasgow Coma Scale (GCS) score, transfusion requirements, and fluid requirements were associated independently with mortality. Therefore, the task force chose to evaluate the current cut-off values for GCS scores and systolic blood pressure (SBP) for the geriatric patient in their sample. Zautcke et al also emphasized the importance of falls in geriatric trauma.Reference Zautchke, Coker, Morris and Stein-Spencer24
Sugimoto et al compared patients >65 years of age to patients ≤65 years of age in a Level-I Trauma Center in Japan.Reference Sugimoto, Aruga, Hirata and Shindo21 More than half of the geriatric patients admitted were pedestrians who were struck by vehicles. They noted a higher mortality and higher rate of unexpected death in older than in younger patients. Helling et al examined all patients admitted to their Level-I Trauma Center with falls <20 feet.Reference Helling, Watkins, Evans, Nelson, Shook and Van Way22 They found that although only 25% of patients were >60 years of age, half of the total mortality occurred in this group. As a result, the Task Force decided to examine the impact of falls from any height in the current study.
Richmond et al performed a retrospective survey of a large statewide database of trauma admissions in Pennsylvania focusing on adults >65 years old.Reference Richmond, Kauder, Strumpf and Meredith25 In additionl to emphasizing the importance of falls in this age group, the authors noted the importance of injuries involving multiple body regions. Falls increased the risk of discharge to a specialized nursing facility. Interestingly, while co-morbidities did not increase the risk of death, they did increase the risk of complications during the initial hospital stay.
The analysis of these studies led the Task Force to examine the criteria listed in Table 2. The objective of the current study was to determine if there were criteria for geriatric patients that would identify an increased mortality risk when compared to the existing adult triage criteria. This analysis of these criteria either could result in additions to the current Ohio criteria or alterations to existing criteria (e.g., change in the blood pressure threshold for transfer).
Table 2 Potential geriatric field-destination criteria identified by literature review6.16,19-26

Criterion Validation Using the Ohio Trauma Registry
The Task Force considered each of the potential geriatric-specific criteria (Table 2) independently through a statistical analysis using the Ohio Trauma Registry. It was decided that any individual criterion that carried a mortality rate equal to or greater than that for patients between 16 to 70 years of age would be included in the final recommendations. In a pilot investigation performed prior to the complete data analysis, it was concluded that other factors such as length of stay (LOS), complications, and intensive care unit (ICU) admission rates showed similar patterns in their differences between elders and other adults as did mortality. Therefore, to simplify the analysis, these factors were not utilized in this analyses, only mortality differences were considered (Table 3). This is consistent with other studies of elderly trauma patients that have focused on mortality as a primary outcome.Reference Finelli, Jonsson, Champion, Morelli and Fouty28–Reference Victorino, Chong and Pal30
Table 3 Comparison of gross mortality, length of stay (LOC), intensive care unit (ICU) length of stay (LOS) and complications between adult trauma patients and geriatric trauma patients

Data in the Ohio Trauma Registry were obtained for each of the potential criteria. The Ohio Trauma Registry is a legislatively mandated registry of trauma patients under ORC 4765.06 and defined by the International Classification of Diseases, Clinical Modification (ICD-9-CM) codes related to trauma, ranging from 800-959.9. Designated trauma centers and non-trauma hospitals are required to provide data with almost 90% of all Ohio hospitals participating. Excluded ICD-9-CM codes include those for isolated hip fractures, late effects of injury, foreign bodies, and superficial abrasions.31 In addition to having an appropriate ICD-9-CM code, patients eligible for inclusion were required to meet the following criteria: (1) a first or initial admission for ≥ 48 hours; (2) transfer into or out of a hospital or emergency department setting regardless of length of stay; (3) patient declared dead on arrival; or (4) patient death after receipt of any evaluation or treatment. Mortality was considered to be present if there was a record of death in the emergency department or the inpatient disposition fields. Trauma patients who are declared dead on scene or those who are admitted for <48 hours are not required to be reported to the Registry. To avoid double counting of patients, registry entries from the transferring institution in cases where the patient was transferred to another acute care facility were excluded. These patients were captured from the records of the facility where final disposition occurred.
Body regions, determined by using the Barell injury diagnosis matrix, included the following: (1) traumatic brain injuries;
(2) head/face/neck; (3) chest; (4) abdomen/pelvis; (5) spine; and (6) extremities.32 The Barell injury diagnosis matrix (complete name: Barell Injury Diagnosis Matrix, Classification by Body Region and Nature of the Injury) standardizes data selection and reports, using a two dimensional array (matrix) that includes all ICD-9-CM codes describing trauma. It serves as a basic tool in epidemiological and clinical analyses of injury data. The matrix displays the nature of injury in columns and body region in rows placing each ICD-9-CM code in the range from 800 to 995 in a unique cell location in the matrix. Each cell includes the codes associated with a given injury. The matrix rows and columns easily can be collapsed to get broader groupings, or expanded if more specific sites are required.
Statistical Processing
Potential triage criteria were compared in patients ≥70 years of age (geriatric) to all other adult patients (ages 16 through 69 years). Each of the potential triage criteria was analyzed to determine whether it identified a greater risk of mortality for patients ≥70 years of age than for other adults included in the Trauma Registry. Seventy years of age was chosen to define the geriatric population after statistical analysis of the Ohio Trauma Registry demonstrated that it was at this age that mortality rates consistently increased.Reference Caterino, Valasek and Werman29 Those criteria that demonstrated a significantly increased risk of mortality were included in the final triage criteria. Analyses were conducted using Stata version 10 (StataCorp, College Station, TX).
For the GCS score and systolic blood pressure (SBP), cutoffs were identified in the elderly that were associated with significantly greater mortality than the currently used field destination guidelines in adults. The GCS score was measured on an ordinal scale. The SBP was converted into groups of 10 mmHg from its initial continuous scale to ease interpretation and aid applicability in the field. Mortality rates with 95% confidence intervals (CI) for each age group were calculated both at the currently used cutoff as well as other potential cutoff values identified by the review of the literature. These rates were compared using Pearson's chi-square analysis and the relative risk (probability) for death was identified. The final suggested criteria included those cutoff points, which were associated with greater or equivalent mortality in the elderly as compared to the current triage cutoff in the adult group as defined by non-overlapping CIs of the mortality rates, by assessing the relative risk, and/or a p <0.05 on chi-square analysis.
Categorical variables that were analyzed included mechanism of injury, injury to specific organ systems in patients with falls, pedestrians stuck by a motor vehicle, injury to multiple body regions, presence of several co-morbid conditions, and motor vehicle crash (MVC) with long bone fracture(s). For each variable, mortality rates were calculated in both age groups (elderly and other adults) and an odds ratio (OR) with 95% CI was obtained. Additionally, chi-square analysis was used to compare the two groups for each criterion. Mortality was considered to be significantly greater in the elderly if there was a calculated odds ratio with 95% CI >1.0 and/or a p <0.05 on the chi-square test. Multiple logistic regression analysis was not performed as
the suggested criteria were tested on an individual basis to see if alternative cutoffs were more useful, but a comprehensive risk factor model was not sought.
Results
From 01 January 2003 through 31 December 2006, 111,529 records of all patients ≥16 years of age were entered into the Registry. Of these, 90,597 were included in the analysis after eliminating the initial visit record for patients seen at more than one institution. Approximately 90% of Ohio hospitals submitted data to the Registry, as required by law.33 Data are included from verified trauma centers as well as non-trauma centers in the state.
Geriatric Patients and GCS Scores
Current triage criteria state that adults with a GCS score of ≤13 should be transported to a trauma center. Figure 1 demonstrates mortality rates at each GCS for both elderly and adult patients.

Figure 1 Analysis of Glasgow Coma Scale (GCS) score for both geriatric and other adult patients
Mortality in adults 16–69 with a GCS score = 13 was 3.9% (95% = 2.8–5.0). By comparison, mortality of the patients ≥70 with GCS = 15 was 2.9% (2.6–3.2), with GCS score = 14 was 6.3% (5.1–7.5), and with GCS = 13 was 14.4% (11.1–18.5). Patients ≥70 years of age with a GCS score = 14 were more likely to die than were adults with GCS = 13 (RR = 1.65, 95% = 1.14–2.40) (p = 0.01). Therefore, the Task Force recommended that a GCS of 14 or less for an elderly patient be used as a criterion for transport to a trauma center. However, since some elderly patients have underlying disorientation and thus, have a “Best Verbal Response” of 4 out of 5, an additional qualifier was added to suggest that there must be some evidence of recent head trauma for triage to a trauma center.
Geriatric Patients and Systolic Blood Pressure
The current triage rule for adults stipulates that patients with a SBP <90 mmHg should be evaluated in a trauma center. The mortality rates at each SBP for both elderly and adult patients are in Figure 2.

Figure 2 Analysis of first recorded systolic blood pressure (SBP) for both geriatric and other adult patients
Mortality in adults ages 16–69 with SBP 81–90 mmHg was 12.0% (95%CI = 10.1–14.0). By comparison, mortality in the elderly with SBP 81–90 mmHg was 19.2% (15.1–23.2%). The mortality for geriatric patients at SBP 91–100 was 11.8% (9.5-14.0) and with SBP 101–110 mmHg was 8.6% (7.2–10.0%). The older adult with SBP 91–100 were equally likely to die as adults with SBP of 81–90 mmHg (RR = 0.98, 95% CI = 0.73–1.32) (p = 0.89). The geriatric patient with SBP101–110 were less likely to die than adults at the current cutoff of 81–90 mmHg (RR = 0.69, 95%CI = 0.53–0.90) (p = 0.005). This analysis suggests that an older adult patient with a SBP <100 mmHg is equivalent to the current triage criteria for other adult patients. As a result, the Task Force proposed that elderly trauma patients with a SBP of <100 mmHg be evaluated in a trauma center.
Falls Associated with Head, Chest, Abdominal, or Spinal Injury
The data pertaining to falls associated with injury to the head, spine, chest, or abdomen/pelvis were studied to identify their association with increased mortality in the older adult as compared to younger adults (Table 4). Only falls associated with signs of head injury were associated with a significantly increased mortality in the elderly population (OR = 2.12, 95%CI = 1.88–2.39) (p <0.001). It should be noted that all patients with evidence of spinal cord injury already are triaged to a trauma center according to the current triage guidelines. Thus, the Task Force proposed the additional caveat that geriatric trauma patients with falls and evidence of traumatic brain injury (regardless of GCS score) should be triaged to a trauma center.
Table 4 Comparison of mortality for elderly and adult patients examining the various field-destination criteria

Mechanism of Injury and Injury Modifiers including Prolonged Extrication, Significant Vehicle Damage, Patient Ejected, and Pedestrian Struck
The the use of data contained in the Ohio Trauma Registry currently is limited in its ability to capture the modifiers of mechanism of injury for trauma patients, such as prolonged extrication, significant vehicle damage, and patient ejection. However, pedestrians who have been struck by vehicles are readily identified using the ICD-9-CM external cause of injury codes (E-code). The data included in Table 4 indicate that there occurs a near doubling of the mortality rate for older adult pedestrians struck when compared to all other adults (OR = 2.39 (1.77–3.21; p <0.01). The Task Force proposed that geriatric pedestrians who are struck by a moving vehicle be triaged to a trauma center.
Geriatric Patients and Multiple System Injuries
Older adult patients with multiple body regions injured had greater mortality rate than did those with an injury to a single body region (8.0% vs. 3.7%) (Table 4). Geriatric patients with multiple body region injuries (8.0%, 95%CI = 6.8–9.2%) had statistically significant higher probability of death as compared to that for other adults with injuries to multiple body regions whose mortality rate was 6.3% (95% CI = 5.7–6.9%; p <0.001). Therefore, it was recommended that geriatric patients with injuries to more than one body system be included in the revised field destination guidelines and ultimately would be assessed in a trauma center.
Geriatric Patients and Co-Morbidities
Among the co-morbidities that can be identified in the Ohio Trauma Registry are cardiac disease, pulmonary disease, diabetes (Types I and II), dialysis, immunosuppressive disease, and clotting disorders (including the anticoagulant use of warfarin). The impact of these co-morbidities on mortality is in Table 5. Data synthesis demonstrates that in the presence of each of the disease processes described, geriatric patients have a statistically significant increase in mortality rate compared to all other adult patients. While geriatric trauma patients with any of the above co-morbid conditions had a statistically significant higher risk for death than did their adult counterparts, the list of conditions collected by the Ohio Trauma Registry contains approximately 30 specific disorders. It was felt that such an exhaustive list could not be translated accurately into practice. As such, the Task Force supported the recommendation that a geriatric trauma patient with any co-morbidity be given special consideration for transfer to a trauma center. This language already existed in the current statewide adult field destination criteria; thus, no changes were made.
Table 5 Impact of various co-morbidities on mortality rates among elderly trauma patients as compared to all other adult trauma patients (OR = odd ratio)

Geriatric Patients and Proximal Long-Bone Fractures
Older adult patients with a single proximal long-bone fracture (femur or humerus) following a motor vehicle crash have much higher mortality and morbidity rates than adults in general (OR = 2.41 (1.81–3.21; p <0.001) (Table 4). Therefore, the presence of any proximal long-bone fracture following motor vehicle trauma would require an evaluation in a trauma center in the proposed triage scheme.
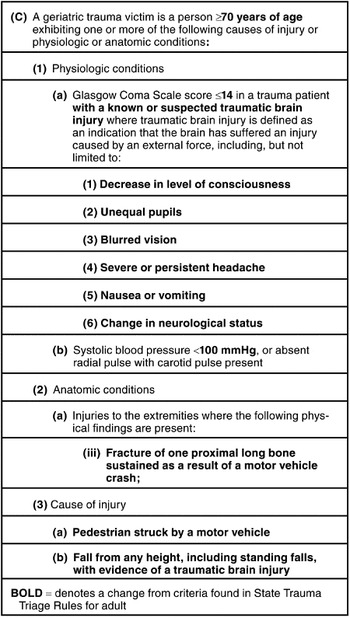
The final recommendations of the Task Force made to the Trauma Committee for geriatric-specific field destination criteria are included in Table 6. The current state-defined field destination criteria in Table 1 would remain applicable for adults age 16 through 69 years.
Table 6 Geriatric-Specific Trauma Triage Criteria (proposed) — text in bold denotes change from current adult criteria (Table 1)

well as compliance issues.Reference Chang, Bass, Cornwell and MacKenzie17,Reference Huei-Ming, Mackenzie, Alcorta and Kelen37,Reference Baez, Lane and Sorondo38 To date, there is no truly ideal triage tool.
As a result of this analysis, the Task Force recommended additional geriatric-specific criteria that are listed in Table 6. These include an increase in both the GCS score and SBP used to determine field destination for geriatric patients, as well as the addition of single long-bone fracture in motor vehicle collision and pedestrian struck as definitive destination criteria. These criteria represent changes or additions to the existing criteria for other adult trauma patients. These recommendations were reviewed and approved by the Trauma Committee, which then sent its recommendations to the State of Ohio Board of Emergency Medical Services (EMS) Board. The EMS Board, of which 15 of 20 members represent field EMS providers, voted unanimously to adopt the new criteria and recommended incorporation in to the Ohio Administrative Code. Prior to implementation, the EMS Board was required by law to distribute the proposed rules throughout the EMS community and to hold a public hearing on the proposed rules. Another public comment opportunity on proposed rules was required by the General Assembly. Upon completion of the legally proscribed process, the new criteria took effect on 29 December 2008.
These criteria represent a starting point for Ohio. Further study will be needed to identify whether these criteria improve triage for elderly patients. By statute, the EMS Board is required to re-evaluate the field destination rules every three years with the intent of minimizing over- and under-triage. Thus, the impact of changes in the triage criteria such as the preferential transport of elderly trauma victims with more than a single body system injury, will have to be determined by subsequent analyses.
Limitations
There are several limitations in this study. The most significant is the limitation of the statewide Trauma Registry, which contains information on a limited population of trauma patients. By definition, the database includes only those patients who are admitted for a total duration of >48 hours in addition to all trauma deaths and those patients transferred between facilities. Therefore, the Registry is not comprehensive for all trauma patients. While most of the trauma patients can be identified in the EMS Incident Reporting System (EMSIRS), it currently is not possible to directly link the prehospital record to the Trauma Registry using a unique patient identifier. Additionally, the current system as it exists, does not enable the Trauma Committee to ever truly know the sensitivity and specificity of the geriatric triage criteria.
It also should be noted that the Ohio Trauma Registry dataset has not been validated externally. All data within the Registry including E-codes, are limited by the thoroughness of individual chart reviews conducted at centers submitting data. However, a review of prevalence of co-morbid diseases in the database population reveals a similar prevalence between the Ohio Trauma Registry and other national estimates. For example, the prevalence of diabetes in the registry in patients >60 years was 21.2%, as compared to NIH figures of 20.9% in this age group.39 Similarly, the prevalence of coronary artery disease in the entire registry population was 6.5% as compared to an expected prevalence of 6.9% in the general population.Reference Rosamond, Flegal, Furie, Go, Greenlund, Haase, Hailpern, Ho, Howard, Kissela, Kittner, Lloyd-Jones, McDermott, Meigs, Moy, Nichol, O'Donnell, Roger, Sorlie, Steinberger, Thom, Wilson and Hong40
Additionally, since the geriatric-specific criteria developed were based on the Ohio Trauma Registry, they may not be valid as destination criteria in other states. At least one abstract has called these specific criteria into question when tested against in
Discussion
Development of field destination guidelines cannot be viewed as an exact science. Most current triage schemes are based to some degree on the current guidelines promulgated by the American College of Surgeons and those recently revised by the [US] Centers for Disease Control and Prevention. These triage guidelines emphasize physiologic and anatomic measures of patient injury. In addition, the patient's mechanism of injury, as well as other conditions such as age and health status, often are considered modifying factors. Studies that have examined the ACS guidelines have demonstrated that they are limited by high over- and under-triage ratesReference Phillips, Rond, Kelly and Swartz16,Reference Ma, MacKenzie, Alcorta and Kelen18,Reference Demetriades, Sava, Alo, Newton, Velmahos, Murray, Belzberg, Asensio and Berne34–Reference Scheetz36 as another setting.Reference Cushman, Patel, Jones, Swor, Lerner and Shah41 However, the methodology can be employed by other state trauma systems in developing their own set of geriatric-specific field destination criteria.
Finally, using a single variable such as mortality, in defining the geriatric field-destination criteria was limiting, especially since it is clear that this population consumes significant total resources, ICU resources, and suffers greater morbidity when ill or injured. This analysis showed conflicting findings for the adult and geriatric populations when total length of stay, ICU length of stay, and number of complications were examined, even after only survivors were examined to discharge. Since a reliable surrogate measure for morbidity or resource consumption could not be found in this analysis, the analysis was simplified to consider only mortality. Even in this parameter, 60-day post-discharge survival may have been a more accurate measure.Reference Mullins, Mann, Hedges, Worrall, Helfand, Zechnich and Jurkovich42
It should be remembered that the charge of the Trauma Committee was limited to defining geriatric-specific criteria that performed at least as reliably as the existing field destination rules. The Committee has been able to accomplish this task. Further studies should examine the impact and performance of these geriatric-specific criteria.
Conclusions
This analysis has enabled the State of Ohio to develop evidence-based geriatric-specific criteria based on the unique attributes of the geriatric population and their responses to traumatic injury. Further efforts will be directed at improving the trauma system to include a more comprehensive view of all trauma victims and a better link to our existing EMS database. Future analysis of these criteria will be conducted to determine their impact on geriatric trauma outcomes.
Abbreviations:
ACS = American College of Surgeons
EMS = emergency medical services
ICU = intensive care unit
GCS = Glasgow Coma Scale
ICD-9-CM = International Classification of Diseases, Clinical Modification
MTOS = Major Trauma Outcome Study
MVC = motor vehicle crash
ODPS = Ohio Department of Public Safety
SBP = systolic blood pressure
Appendix 1 Members of the Trauma Committee of the Ohio Board of Emergency Medical Services