Introduction
When natural disasters occur, many people lose their homes and are forced to live in evacuation centers. These evacuees face dramatic changes in their living conditions and are exposed to various health risks due to environmental factors. Living under these circumstances can make it difficult for evacuees to maintain hygiene, it can force them to miss out on routine health care including medication, and it may cause psychological stress. Further, certain infrastructure factors, such as contaminated water, loss of electricity, and interrupted gas supply, can also negatively affect evacuees. Consequently, infectious disease is a prevalent health condition in these circumstances. Reference Izumikawa1 Overpopulated and confined living spaces that lack sufficient ventilation can easily lead to outbreaks of influenza, norovirus, and tuberculosis and can invite the transmission of other pathogens. Reference Izumikawa1 All types of disasters frequently cause deaths in the acute phase. Disasters can also cause a variety of long-term disabilities during the chronic phase, including spinal cord injuries, traumatic brain injuries, fractures, limb amputations, peripheral nerve injuries, and crush injuries, especially if the disaster was caused by an earthquake, volcano, storm, or flood. Reference Khan, Amatya and Gosney2
Japan experiences frequent and various natural disasters, including typhoons, heavy rain, heavy snow, floods, and sediment-related disasters such as earthquakes, tsunamis, and volcanic eruptions. In fact, 20.5% of all past earthquakes with a magnitude of 6.0 or higher have occurred in Japan, and 7.0% of the world’s active volcanoes are located in Japan. Reference Izumikawa1 This report describes the assessment system used during a recent natural disaster in Japan that generated heavy rains in the western part of the country from July 3 through July 8, 2018. The heavy rain caused river inundations, flood damage, and associated sediment disasters in the western part of Hiroshima Prefecture. The disaster also caused substantial damage to human life and infrastructure. As of March 11, 2020, there were 224 people dead, eight missing, and 459 who had sustained either severe or mild injuries. In addition, 52,033 homes were damaged during this disaster. 3 The authors were dispatched as members of the Infection Control Team, Japan Medical Association Team, and Disaster Psychiatric Assistance Team to the affected area and evacuation centers. The disaster relief effort included tasks to control and prevent infectious diseases, improve the evacuation center environments, support the rehabilitation of evacuees who were displaced at evacuation centers, improve evacuees’ mental status, and prevent deterioration of oral health. The authors noticed that certain evacuee health problems, such as poor oral health, depleted mental health, or poor motor function, did not receive adequate attention at the evacuation centers, yet these issues would have long-term impacts on health and well-being. However, there was no sufficient tool available to staff for communicating these health issues with other health professionals and relevant government departments. This study reports the development of a health assessment sheet that was recently adapted to suit evacuees’ needs after the Hiroshima natural disaster in 2018.
Objective
This study aims to develop two types of information sheets:
-
1. To assess the evacuation center environment, and to report the outcome to local health departments of prefectures and cities; and
-
2. To assess the health and well-being of evacuees, and to report the outcome to managers of the evacuation centers.
Methods
The first form was designed to be completed by an evacuation center manager to report and share information about the center’s environmental health and overall evacuees’ health conditions. The sheet is shared with the infection control team and teams supporting oral health, mental health, and rehabilitation of motor function. The second form was developed for use as an evacuee registration sheet. This is a self-administered document that evacuees complete with their medical and health information upon arrival at the center. The modified Delphi method Reference Dalkey and Helmer4,Reference Dalkey5 was used to develop these sheets, and the researchers consulted medical doctors who specialize in infectious disease, psychiatry, rehabilitation, and dentistry. Prior to developing the new information sheets, the researchers (HK, HO, KT, HN, YM, HY, and MM) reviewed sheets developed by the Department of Public Health Promotion, Hiroshima Prefecture. The initial consultation with the medical doctors was conducted face-to-face to discuss the symptoms commonly experienced by evacuees in a disaster situation, and those symptoms were listed as part of the sheet in November 2018. The second consultation was conducted in December 2018 to summarize previously collected information, and the outcomes were reported to the medical doctors to justify the items included in the report. The consultation from the previous month was summarized with references in January 2019. The process of developing and revising the sheets, including determining what should be included to assess the status of the evacuation center environment, took approximately three months.
Results
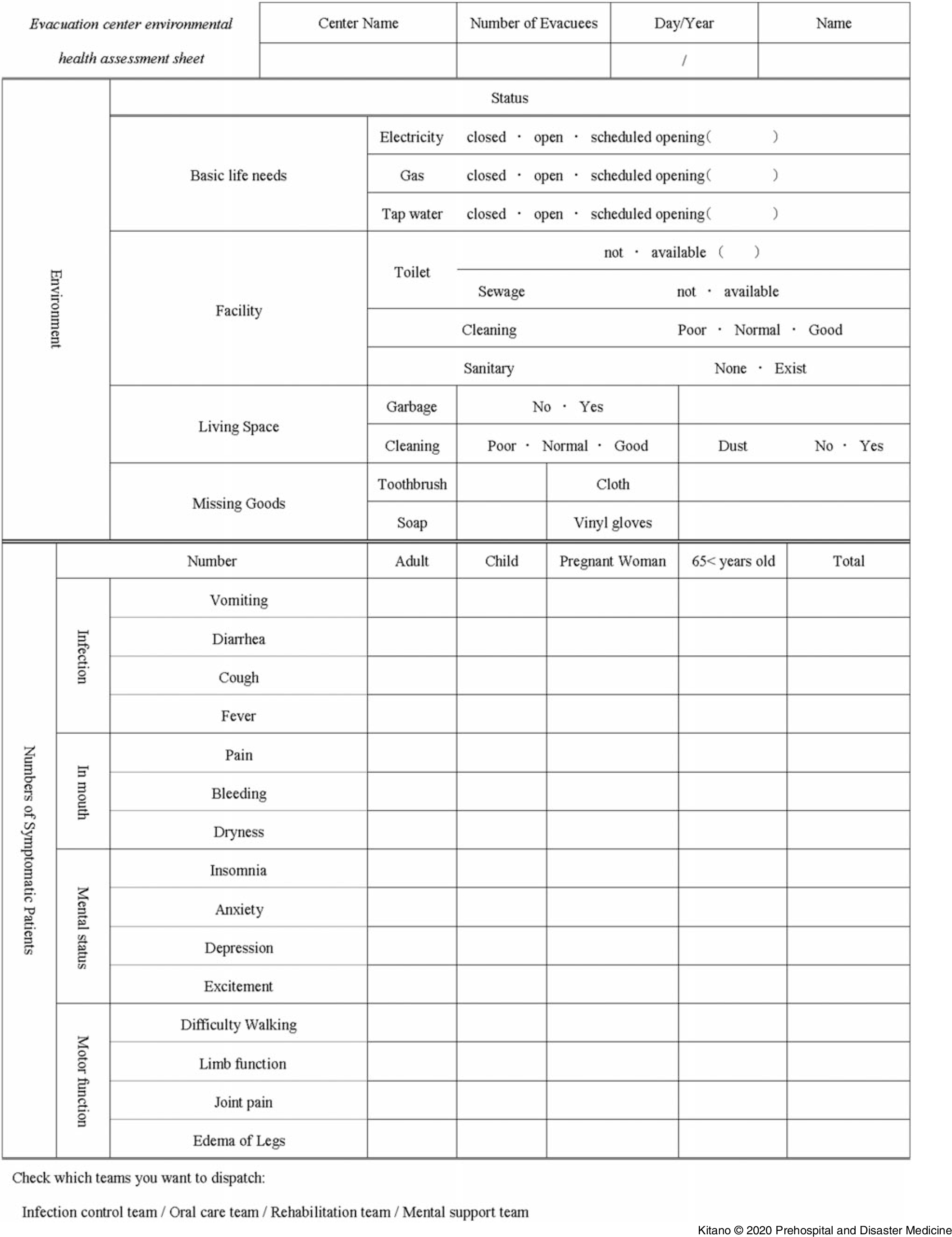
After consulting with the stakeholders of evacuee health conditions and evacuation center environments, the following category was extracted and included in each sheet (Figure 1).

Figure 1. Evacuation Center Environmental Health Assessment Sheet.
Evacuation Center Environment Status
This sheet concerns both the evacuation center environment and evacuee health and is structured to reflect two core categories: environment (of evacuation center as a living space) and the overall evacuees’ health presentation. The first category concerning the evacuation center environment covers basic life needs (ie, electricity, gas, and water) and includes facility status, such as maintenance of toilets, sewage system, and handwashing areas. The sheet allows managers to assess whether sanitation is maintained and the availability of garbage removal and supplies of sanitation and personal protective equipment.
Evacuees’ Health Presentation at the Center
The sheet allows managers to indicate patient symptoms that potentially signal infectious disease (ie, nausea, vomiting, diarrhea, cough, and fever) as they are responsible to maintain the center. These are the main symptoms of infectious diseases that are easily transmitted in evacuation centers because of difficulty in providing proper hand hygiene. In addition, as these symptoms are the most common indicators of respiratory and gastrointestinal infections, infection control team members need this information when treating patients with infections. Symptoms such as oral pain, oral bleeding, and mouth dryness, which may be caused by limited access to water, are also included on the sheet. These symptoms require urgent treatment by a dentist, as mouth dryness poses a risk for infection or bleeding. Psychiatric symptoms, such as insomnia, anxiety, depression, and stress, are also included. These symptoms can be caused by a disaster or the change of living conditions at an evacuation center, and can have long-term impacts on the evacuees’ health and well-being. Further, the sheet includes items to evaluate motor function such as difficulty walking, limb function deterioration, and back or joint pain. Identifying a deterioration in motor function is important because some elderly people entering evacuation centers display these symptoms. The manager can separately indicate the demographic information of evacuees who present with these symptoms. Finally, the sheet includes a section that allows the evacuation center manager to request assistance from the relief team depending on their health needs (Figure 2).

Figure 2. Evacuee Registration Sheet.
This is a self-administered information sheet provided to each evacuee to record information about medical history and any illnesses. For example, the evacuees can describe the medications they are currently taking, and any health conditions, such as pregnancy or chronic illness. This sheet also includes information regarding oral health, such as the need for dentures. Further, the sheet contains a section for evacuees with disabilities to report whether they have a disability certificate, and to indicate whether they require any assistive devices.
Discussion
Japan has experienced three major natural disasters in recent years—the 2011 Great East Japan Earthquake, the 2016 Kumamoto Earthquake, and the 2018 West Japan Torrential Rainfall. These disasters caused substantial damage to the communities in which they occurred.
Once a natural disaster strikes a community, the risk emerges that various infectious disease epidemics could occur. Reference Connolly, Gayer and Ryan6-Reference Hatta and Kaku8 The population density of evacuees within the evacuation centers only increases this risk. Symptoms of illness, such as respiratory, gastrointestinal, and dermatological issues, can occur because of close contact of humans in non-hygienic and poorly ventilated environments. Reference Suzuki, Uwano and Ohrui9 Therefore, the information sheets must contain information regarding the evacuation center environment and evacuee screenings to detect any signs of infection.
Further, some categories represent essential items to be included in the sheet. For example, oral health is one of the most important issues for survivors of disaster. One study found that disaster evacuees who had received dental treatment for lost or fractured dentures or clinical oral health problems before the disaster were likely to show low levels of oral-health-related quality of life (OHRQol). In addition, perceived systemic health and serious psychological distress were also associated with low levels of OHRQol. Reference Kishi, Aizawa and Matsui10 Survivors who lose their dentures are at risk of eating difficulties, speech problems, emotional distress, and feelings of embarrassment upon smiling, laughing, or showing teeth. Reference Sato, Aida and Takeuchi11 Therefore, the new evacuation center and evacuee registration sheets include these items on abnormal symptoms in the mouth and dentures. This will support the evacuees in maintaining their health status and quality of life.
Numerous manuscripts have discussed how disasters can lead to various mental health outcomes. Reference Hussain, Weisaeth and Heir12-Reference Thienkrua, Cardozo and Chakkraband14 After disasters occur, many mental health issues, such as specific phobias, agoraphobia, social anxiety disorders, posttraumatic stress disorder (PTSD), major depressive disorders, and dysthymic disorders, are reported. Reference Hussain, Weisaeth and Heir12 Moreover, the number of survivors burdened with PTSD is substantial, Reference Neria, Nandi and Galea13 and a loss of livelihood is independently and significantly associated with symptoms of PTSD, anxiety, and depression. Reference Thienkrua, Cardozo and Chakkraband14 The researchers included certain psychiatric symptoms (eg, insomnia and stress) on the information sheet, as such symptoms could adversely affect evacuees living in evacuation centers.
Natural disasters often cause long-term disabilities, the most common of which are spinal cord injuries, traumatic brain injuries, fractures, limb amputations, peripheral nerve injuries, and injuries from crushing. Reference Khan, Amatya and Gosney2 Liu, et al Reference Liu, Kohzuki and Hamamura15 reported that attempts by multiple rehabilitation organizations to share the same information about patients were successful in revealing poor preparedness, satisfactory initial response, and supportive activities. Zhang, et al Reference Zhang, He and Lin16 mentioned that fractures were the main issue among the seismically wounded in the Wenchuan Earthquake (2008), and that survivors with fractures experienced reduced range of motion, muscle force, and capacity for activities of daily living. Therefore, the physicians involved in rehabilitation should pay greater attention to muscle force exercises, joint mobilization, and occupational therapy during the early phases after the disaster. Likewise, a study found that rehabilitation interventions were effective for the survivors who had spinal cord injuries. Reference Rauch, Baumberger and Moise17 Reinhardt, et al Reference Reinhardt, Li and Gosney18 presented the effectiveness of medical rehabilitation intervention for natural disaster survivors in helping them overcome the health impacts of disasters. These findings highlight the need to incorporate medical rehabilitation into response planning and disaster management for future natural catastrophes. The information from the perspective of rehabilitation is essential because it has not been seen as necessary for evacuees or as required information about evacuation center environments. Providing this information supports the holistic recovery of evacuees, not only in the acute phase, but also in the chronic phase of a disaster.
Limitations
The study has some potential limitations. The information sheets have not yet been implemented in a disaster; therefore, their usefulness needs to be confirmed. In addition, it is necessary to verify that the information sheets are useful for multiple types of disasters.
Conclusion
The present study created two new information sheets based on the researchers’ experiences during the 2018 West Japan Torrential Rainfall. These newly developed report templates concern not only evacuee health during the acute phase of a disaster, but also include information that impacts their well-being and long-term health recovery, and aim to improve both evacuee conditions and evacuation center environments.
Conflicts of interest
none