Introduction
Despite injury’s rank as the leading prehospital condition in Sub-Saharan Africa, over 90% of the African population does not have access to Emergency Medical Services (EMS).Reference Mould-Millman, Dixon and Sefa1 In low-income countries and in rural areas where formal EMS penetrance is low, commercial drivers, volunteers, and other bystanders currently provide a large proportion of prehospital transport and occasionally also provide first aid.Reference Nielsen, Mock, Joshipura, Rubiano, Zakariah and Rivara2 In low- and middle-income countries (LMICs) without formal EMS, 80% of injury deaths occur in the prehospital setting compared with just 59% in developed settings.Reference Mock, Jurkovich, nii-Amon-Kotei, Arreola-Risa and Maier3 If expanded, EMS in LMICs could address 45% of all deaths and 36% of the total disease burden.Reference Jamison4 The World Health Organization (WHO; Geneva, Switzerland) recommends lay first responder (LFR) programs as the first step toward developing formal EMS in settings without formal, developed prehospital systems.Reference Jamison4-Reference Mock6
Given the WHO consensus on LFRs, a number of authors have since investigated establishing LFR programs in LMICs, primarily in urban environments.Reference LaGrone, Riggle and Joshipura7-Reference Orkin, Curran and Fortune13 With the exception of an investigation in rural Iraq,Reference Murad and Husum14,Reference Husum, Gilbert, Wisborg, Van Heng and Murad15 there is a scarcity of research investigating LFR program development in predominantly rural, low-resource settings of low-income countries.16
An LFR curriculum was implemented in the Salamat Region of Chad (a rural, low-resource setting) to evaluate the efficacy of a WHO-informed prehospital emergency care curriculum by measuring the knowledge improvement of participants, evaluating longitudinal program impact on the care trauma victims in the community receive, and tracking program cost. Twelve-month, qualitative follow-up interviews were conducted with initial participants and community members to understand the factors motivating continued voluntary participation as first responders in their community, aiming to inform future program continuity and investigate the feasibility of scaling up prehospital emergency care by leveraging pre-existing transportation providers in low-resource settings.
Methods
Study Design
A pre-/post-course test measured knowledge improvement (assessed with a Wilcoxon signed-ranks test) while a one-way sensitivity analysis investigated program cost. Trainees submitted incident report forms after each patient encounter to assess longitudinal impact. To evaluate the longer-term effect of the program, qualitative follow-ups were conducted with participants via structured interviews 12 months after the initial training. Data were compiled in Microsoft Excel (Microsoft Corporation; Redwood, Washington USA) and analyzed in R (R Foundation for Statistical Computing; Vienna, Austria). Ethical approval was obtained for the study from the Washington University in St. Louis (St. Louis, Missouri USA) Institutional Review Board and the local Chadian government prior to study commencement.
Course Development
Two American National Registry of Emergency Medical Technicians (NREMT; Columbus, Ohio USA) developed the LFR course, adapting a WHO-informed curriculum previously implemented in Uganda, consisting of five components: principles and definitions of first aid, scene safety, airway management/hemorrhage control (ABCs), fracture splinting, and victim transport (Table 1).Reference Delaney, Bamuleke and Lee17
Table 1. Components of the Prehospital Trauma Course

Abbreviations: ABC, airway management/hemorrhage control; BSI, body substance isolation; CPR, cardiopulmonary resuscitation; EMS, Emergency Medical Services.
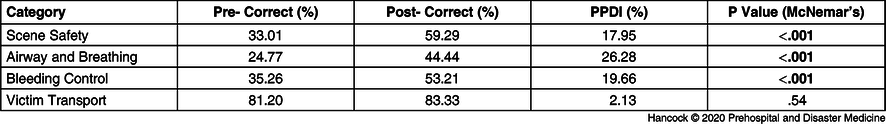
The final curriculum was translated and revised in collaboration with a local physician, given his knowledge of local mechanisms of injury. To ensure local ownership of the course and cultural appropriateness, investigators collaborated with the local Red Crescent chapter and co-taught the course with a local Red Crescent instructor. The five-hour course was taught in Chadian Arabic in a lecture format, interspersed with hands-on, breakout sessions, administered in a 58-slide slideshow using graphics for learning objective reinforcement. Two instructors led each course, with an additional assistant present during hands-on, breakout sessions. To maximize practicality for participants, each course lasted five hours in total and was taught over a single day to accommodate participants, with up to 20 motorcycle taxi drivers participating in each class. Upon course completion, each participant was awarded a certificate of completion and given a first aid kit, stocked with locally sourced materials to promote program sustainability, with a cost per kit of US$12.79 (Table 2).
Table 2. First Aid Kit Materials
a Exchange rate current to study period (May 2018: US$1 = 560 XAF).
Study Setting
Am Timan is located in southeastern Chad along the Sahel, the semi-arid strip of land along the southern border of the Saharan Desert. The town serves as the capital of the Salamat Region, and though locally known as one of the more resource-rich areas in Chad, Salamat has claimed the title of “poorest region” globally by the World Bank (Washington, DC USA) and International Monetary Fund (Washington, DC USA) as measured by a multidimensional poverty index.16 Though Chadian Arabic is the predominant language spoken, French is widely used in school instruction throughout Chad, as it was formerly a French colony. Am Timan has no formal prehospital emergency system and just two ambulances for its estimated 38,000 residents, which are often nonfunctional. Patients in outlying villages are located far from ambulances and are frequently required to pay to fuel the vehicle beforehand, leading to diminished use and prolonged response times in the event of an emergency. Traditional box ambulances are generally not well-suited for the muddy, impassable roads that predominate during the height of the rainy season, which lasts from July through October.
Study Participants
Based on a local needs assessment and findings from a previous study conducted in Uganda, motorcycle taxi drivers (locally known as “clandos”) were chosen for trainings because of their strategic self-dispersion, profession-driven proximity to road trauma, and the potential scalability of the program post-implementation by leveraging the pre-existing network infrastructure of transportation providers.Reference Delaney, Bamuleke and Lee17 These inherent advantages promoted a wider geographic coverage, as LFRs had no formal notification system sending alerts of accidents. All six clando association chairmen were consulted to gather volunteers for the first responder course, who selected 20 volunteer trainees who expressed interest in participating from each of the six clando associations in Am Timan to ensure even dispersion of first responders. Participants were required to be at least 18 years of age, have reading literacy, and hold membership in a Chadian clando association to meet the criteria for study inclusion. All other individuals were excluded.
Data Collection/Analysis
Pre-/Post-Test—Participants provided verbal consent at the beginning of the course for study inclusion. Upon signing in, participants completed a 15-question, criterion-referenced pre-/post-test, based on a study instrument previously used and validated in Uganda and since improved in a study in Guatemala,Reference Delaney, Bamuleke and Lee17,Reference Delaney, Figueroa and Eisner18 lightly edited by CJH and PGD to reflect course content adapted for the Chadian setting. The test was initially written in English and translated to Arabic and French by bilingual authors (EK, PGD). Translations were confirmed by local stakeholders and piloted with multiple native speakers to ensure question integrity. Participants chose to test in whichever language they preferred. Participants who did not consent, who took either the pre-test or post-test exclusively, or who completed fewer than 50% of test questions were excluded from pre-/post-test analysis. Upon test completion, responses were recorded and stored in a secure box for later analysis.
Correct answers on the pre- and post-test were assigned a score of one point while incorrect, blank, or multiple answers were assigned a score of zero points. A pre-test/post-test difference index (PPDI) was assigned to each question to quantify participant improvement. The primary outcome of interest was measured as the difference between pre- and post-test scores, with score improvement indicating participant knowledge acquisition.
To quantitatively assess participant knowledge acquisition, the mean value, median value, and standard deviation were determined for both the pre- and post-test. Distributions of total scores for the pre- and post-test were compiled and compared using a Wilcoxon Signed-Rank test for nonparametric analysis. Each individual question from the pre-test was mapped to its corresponding post-test analog and compared using McNemar’s Chi-Squared Test in order to examine knowledge acquisition on a by-question basis. In order to assess participant knowledge acquisition in terms of discrete topics in first aid, questions were then grouped according to the four course categories: scene safety, airway and breathing, bleeding control, and victim transport. The proportion of correct answers on both the pre- and post-assessments were recorded, and each category was assessed for significance using McNemar’s Test. Pearson’s correlation coefficient was used to assess the relationship between participant demographics and test improvement.
Cost Analysis—A one-way sensitivity analysis was used to investigate program costs in accordance with a cost projection method previously developed for use with LFR programs by investigators in Uganda.Reference Jayaraman, Mabweijano and Lipnick19 Standard practices were repeated to assess financial feasibility of the expansion of future initiatives in light of costs for similar public health initiatives. First aid materials and training costs were tracked by investigators and collaborating agencies throughout the duration of the study for later analysis.
Longitudinal Incident Report Forms—First aid kits distributed to participants contained incident report forms, which trainees were instructed to complete after patient encounters. Forms in Chadian Arabic and in French were made available to participants. Participants delivered incident report forms to clando association offices in Am Timan, which were stored securely until final aggregation and transcription for data analysis. Clando association secretaries and chairmen were trained to assist motorcycle taxi drivers in completing incident reports if a lack of writing ability was prohibitive. The forms were collected monthly by research assistants and physical copies were destroyed once data were aggregated and stored electronically in a secure database before frequency assessment.
Qualitative 12-Month Follow-Up Interviews and Surveys—Using a sample of motorcycle taxi LFR course participants 12-months post-training, investigators aimed to understand the longitudinal social and financial effects of the program on participants and what motivates long-term continued volunteer participation. For comparison, motorcycle taxis from the same municipality who had not participated in the first aid trainings in 2018 were also randomly sampled.
Motorcycle taxis that had participated in the first aid trainings conducted in 2018 were included in the first sample. A Chadian data collector who was trained by a local investigator (EK) followed up in-person with past participants. The data collector made up to four attempts to contact trainees, who established rapport with participants via shared life experiences. A total of 49 of 108 (45%) of the first-aid-trained motorcycle taxis were successfully contacted and all consented to a follow-up structured interview and survey.
Untrained, randomly sampled motorcycle taxis from the same Chadian municipality who had not participated in the 2018 training comprised the other sample. Participants were required to be at least 18 years of age and members of a local clando association to meet inclusion criteria. Anyone younger than 18 years of age or who were not members of a local clando association were excluded. In accordance with a standard random sampling method previously developed for use with motorcycle taxis in Uganda, standard practices were used to generate a sample size of at least 50 people to be sufficiently representative of motorcycle taxis in the municipality.Reference Kisaalita and Sentongo-Kibalama20 Data collectors approached 51 randomly sampled motorcycle taxi drivers via convenience sampling face-to-face at taxi-stands where taxis regularly wait for customers, all of whom consented and were included and interviewed alone nearby the participant’s taxi-stand. Un-trained respondents were also asked to report what they would be willing to pay to cover both training and first aid kit costs. This reported amount was then compared to their respective weekly income and Pearson’s correlation coefficient was determined to assess the relationship between weekly income and willingness to pay for future first responder courses.
Semi-structured interviews that employed a constructivist grounded theory approach were used. Thematic analysis is used to determine the response-type frequency for the ultimate generation of theoretical constructs and thereby elucidate themes in a grounded theory-based approach. Data were reviewed iteratively and coded for dominant themes, which continued until thematic saturation was achieved. A six-question survey for trained participants and a three-question survey for untrained, randomly sampled participants were generated.
Interview guides and surveys were translated from English into French and Chadian Arabic, and multiple native speakers were consulted during pilot testing to ensure question integrity. Data collectors were fluent in both languages. Audio data and field notes were recorded during interviews and translated into English and securely stored electronically. Notes collected during interviews were reviewed iteratively for dominant themes with multiple investigators independently responsible for qualitative data analysis (CJH, PGD, ZJE) to ensure reasonable concordance of categorized themes and to enhance reliability. The coding scheme followed was based on the framework outlined in Figure 1. Any coding discrepancies were resolved through consensus. Interviews lasted 10 minutes on average, no repeat interviews were conducted, and interview transcripts were returned to participants if comment or correction were sought. The consolidated criteria for reporting qualitative research (COREQ) checklist was used to guide design, analysis, and reporting the qualitative results.

Figure 1. Coding Tree Used for Thematic Analysis.
Results
Six classes of the LFR course were taught. Of the 120 motorcycle taxi drivers that had agreed to participate, 108 attended (90%). In total, 136 LFRs were trained: 108 motorcycle taxi drivers, 15 non-governmental organization employees from Am Timan, and 13 Red Cross affiliate members. Although 96% of trained motorcycle taxi drivers were staged within 10 kilometers of Am Timan, many were found to take passengers to and from villages up to 60 kilometers away, suggesting the breadth of coverage attainable when leveraging transportation providers. Of the 80 motorcycle taxi drivers who responded, 8.8% (7/80) had no education, 18.8% (15/80) had some primary education, 62.5% (50/80) had some secondary education, and 10.0% (8/80) had a university education. The median number of road traffic injuries witnessed by trainees in the past six months was six (n = 103), while the median number of deaths witnessed from injury was four (n = 103).
Participant Knowledge Acquisition
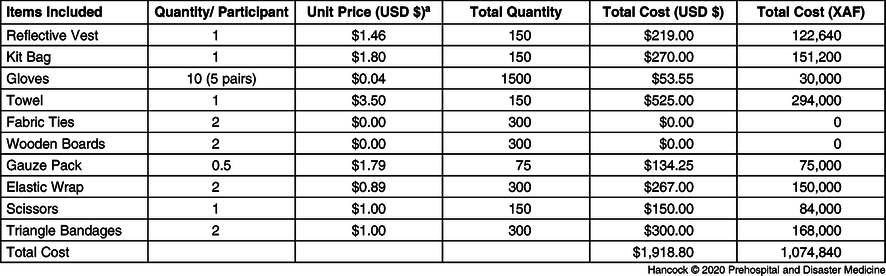
Of the 108 motorcycle taxi drivers participating, 106 completed the survey component of the LFR course. Sixty-seven percent of respondents completed the survey in French version, while 33% completed the version in Arabic. The pre-/post-test assessed knowledge improvement over four groupings of question categories: bleeding control, scene management, airway and breathing, and victim transport. From the baseline measured from the pre-test, investigators found significant knowledge improvement across three of four categories (Table 3).
Table 3. Participant Performance by Topic Category
Abbreviation: PPDI, pre-test/post-test difference index.
Pearson’s correlation coefficient revealed no significance (P >.05) between education (r = 0.09), age (r = −0.11), language (r = −0.22), or years of experience (r = −0.22) with knowledge improvement.
Cost Analysis
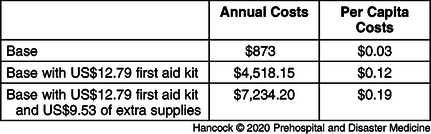
In this pilot program, the 136 total LFRs trained represented 71.6% of the minimum 190 LFRs Disease Control Priorities (DCP) recommended be trained to provide basic prehospital trauma services coverage for a town of 38,000 residents, which is between 0.5% and 1.0% of the total population (suggested range: 190 to 380 LFRs).Reference Jamison4 Calculations for cost projection were completed with a hypothetical amount of 285 LFRs, as the value falls in the middle of the range in DCP-suggested values. The resulting projected annual cost to train 285 LFRs over one year using the aforementioned curriculum and first aid kit components had its training costs informed by a previous cost analysis of a similar LFR program.Reference Jayaraman, Mabweijano and Lipnick19 The projected annual cost for a program was US$873.00, and when divided among Am Timan’s residents, becomes a per capita cost of US$0.03 (Table 4).
Table 4. Training Costs

a Two classes of 20 trainees per day.
b US$9.00/day per trainer.
c US$66/day.
A one-way sensitivity analysis was utilized to determine the addition of components for the US$12.79 locally-sourced first aid kit and with an additional US$9.53 in restocking supply cost (without reflective vest and first aid kit bag); overall costs ranged between US$4,518.15 (US$0.12 per capita for kit without restock) and US$7,234.20 (US$0.19 per capita for kit with restock; Table 5).
Table 5. Per Capita and Total Costs of Training 285 Lay First Responders for Am Timan, Chad
Longitudinal Incident Report Forms
Over the first six months of observation, incident report forms indicated motorcycle taxi drivers treated 71 victims in 38 incident encounters. Seventy-one percent of encounters were road traffic incident-related, with 66 injuries treated in total and five deaths encountered (seven percent of victims). Motorcycle taxi drivers performed airway management in 32% of encounters, bleeding control and bandaging in 61% of encounters, and fracture splinting in 45% of encounters. In 49% of incidents, more than one motorcycle taxi driver LFR was present to assist. After providing necessary prehospital treatment, LFRs provided transport in 82% of incident encounters. Patients requested transport to Am Timan Regional Hospital in 19% of encounters, a smaller health center in 27% of encounters, a private home in 35% of encounters, and no transport in 19% of encounters.
On a scale from one to ten (one = lowest confidence; ten = highest confidence), motorcycle taxi drivers reported an average confidence score of 8.53 (SD = 3.01; n = 38) in the care they had provided following incidents. The spread of incidents treated had been wide, with the furthest incident encounter 30 kilometers from Am Timan’s center. At least nine incidents had occurred outside of Am Timan’s town, while 26 (68%) had been reported to have occurred inside Am Timan (three incident reports did not provide a location).
12-Month Follow-Up Interviews
Survey Responses—A total of 100 motorcycle taxi drivers participated in the semi-structured interview and survey (Table 6).
Table 6. Survey Responses

a Included in longer-form follow-up responses in the Structured Interview.
Of the 51 untrained, randomly sampled motorcycle taxi driver respondents, 96% stated they would be willing to pay for the training. Participants reported the median amount they were willing to pay for the training would be 3,500 Central African Franc (XAF) [IQR: 1,500-8,000] (US$5.98), while the mean amount for the first aid kit was 2,000 XAF [IQR: 2,000-5,000] (US$3.41). The median weekly income of the untrained motorcycle taxi drivers was 22,500 XAF [IQR: 20,000-29,000] (US$38.41). Randomly sampled participants were willing to pay a median of 5,500 XAF [IQR: 3,000-8,000] (US$9.39) for the combined training and kit cost, equating to 24.4% of their weekly income. There was a strong correlation between total weekly income and participant willingness to pay (r = 0.5039026).
Semi-Structured Interview—First-Aid-Trained Motorcycle Taxi Driver Participants: Themes and representative quotations for each structured interview question topic are found in Table 7. Participants reported new knowledge and skills, the ability to help others, and the resultant gain in social status and customer acquisition motivated continued involvement as LFRs. The main challenges faced were first aid kit supply limitations and consistently resupplying.
Table 7. First Aid-Trained Motorcycle Taxi Driver Participant Responses

Untrained, Randomly Sampled Motorcycle Taxi Drivers: Themes and representative quotations for each structured interview question topic are found in Table 8. Respondents desired participating in future LFR courses for the new knowledge and skills they expected to gain, as well as the new ability to help others in their community. They believed training would attract more customers because assisting their community would increase their popularity and provide social distinction.
Table 8. Untrained, Randomly Sampled Motorcycle Taxi Drivers

Discussion
Participants in the LFR course demonstrated significant improvement across three of four curricular categories, except for patient transport, as pre-test scores were already greater than 80% leaving participants little room for improvement. In practice, participants demonstrated competence in important skills, most often using bleeding control skills to treat patients and reporting confidence in the care they had provided. Motorcycle taxi driver participants provided patient transport in 82% of encounters, raising important questions for those seeking to find a sustainable alternative to formal ambulance-reliant EMS that are cost-prohibitive in rural, low-resource settings of low-income countries across Sub-Saharan Africa.
At 12-months post-training, participant outlook is unanimously positive, as participants report LFR training provides new knowledge and skills, an ability to help others, improved social status, and increased customer acquisition as the primary factors motivating continued voluntary participation as first responders in their community. Participants reporting a change in the public’s perception of them as motorcycle taxis, which is normally characterized by stigmatization of reckless driving habits, was unexpected.Reference Galukande, Jombwe, Fualal and Gakwaya21 An unintended consequence of the resultant social status change, derived from increased respect from the public, is the belief that motorcycle taxi drivers trained as LFRs are more responsible than their untrained counterparts. Qualitative data from untrained, randomly sampled motorcycle taxi driver respondents suggest this to be true, as they reported that providing prehospital care attributed social distinction to course participants, increasing their popularity, and subsequent ability to attract customers. Sixty-six percent of participants reported an increase in income. The social and reported financial benefits to having participated appear to drive continued voluntary participation of responders, presenting a model for basic emergency care that could be expanded across other low-resource settings and scaled using pre-existing transportation providers.
All untrained, randomly sampled motorcycle taxi drivers were interested in participating in future LFR courses, expressing a desire to help their community and increase their social status. Ninety-six percent reported they would be willing to pay, with the median amount equating to almost 25% of one week’s income. Future programs subsidized by participants expecting resultant socioeconomic benefits to participation may present an increasingly affordable method for governments to scale basic EMS across rural, low-resource settings, as EMS development has traditionally been limited because of insufficient funding.
Participant feedback focused on first aid kit supply limitations and a desire for consistent skills refresher trainings. Course participants treated a significant number of people in the first six months following the training, especially for such a small municipality when compared with previous studies conducted in urban locations.Reference Delaney, Bamuleke and Lee17,Reference Arreola-Risa, Mock and Lojero-Wheatly22,Reference Mock, Tiska, Adu-Ampofo and Boakye23 To maximize the clinical benefit of LFR programs increasing transport and access to emergency care, local health care systems must also be strengthened to provide competent trauma care upon patient arrival. Further investigation is needed to assess the impacts of LFR programs on local health care systems in resource-limited areas, given these programs may lead to an unintended consequence of over-burdening limited health care facilities.Reference Razzak and Kellermann24
Limitations
Without clinical data, it is not possible to calculate the effect of the LFR program on disability adjusted life years, needed to conduct an extensive cost effectiveness analysis. The one-way sensitivity analysis of program cost revealed that an expanded version of this course meeting DCP-suggested amounts of LFRs (for adequate emergency care coverage) is projected to cost US$0.19 per inhabitant, which is not dissimilar from preventive programs comparatively implemented for the public good, like de-worming programs, which cost between US$0.15 and US$0.25 per child in similar low-income settings.Reference Hall, Horton and de Silva25
Conclusion
Lay first responder programs appear feasible and cost-effective in rural LMIC settings. Local participants demonstrate significant prehospital emergency care knowledge acquisition and effectively care for injured community members. After 12 months, responders report sustained voluntary participation due to social and financial benefits, suggesting sustainability and scalability of such programs in low-resource settings. Injury remains a significant cause of morbidity and mortality globally. With its disproportionate impact upon LMICs and the prevalence of motorcycle taxis across Sub-Saharan Africa, LFR programs are an important first step toward the development of formal EMS.
Conflicts of interest
none











