Background
The newly launched World Report on Disability (WRD) provides global guidance on implementation of the UN Convention on the Rights of Persons with Disabilities (CRPD) and has recently indicated that trauma care and rehabilitation services are essential services to be provided in humanitarian crises.1 The important implications of this report are highlighted when providing care to a patient undergoing amputation. The recent Haitian earthquake and the significant volume of patients requiring amputation in its aftermath highlighted the need for coordinated and standardizedsurgical and peri-operative care in the humanitarian setting. Recommendations in best practices, standards, accountability and accreditation must be addressed in a timely and accurate manner.2–4
Amputations Following Disasters or Conflict Surgical Working Group Summary:
Statement on Team Response:Expanded planning for a multidisciplinary surgical care team.
Statement on Medical Records:Clear, interpretable, culturally-sensitive obtaining of consent and thorough post-operative record keeping.
Statement on Anesthesia and Pain Management:Access to anesthesia and analgesia is a human right. TIVA and USRA are ideal considerations in austere settings. Multimodal management of somatic and phantom limb is a priority.
Statement on Surgical Services:Early window of opportunity for limb salvage or optimize function by preserving appropriate limb length. Guillotine amputation is rarely indicated.
Statement on Rehabilitation Services:Involvement from prior to surgery through to community referral and follow-up. Task shifting between available providers and family/caregiver(s) educationis necessary.
Statement on Discharge and Follow-Up:Clear plan and optimize function prior to discharge.
Statement on Surgical Outcomes:Operative and post-operative amputation-specific outcome measures to develop consistency in care.
Haiti's earthquake left approximately 1500 amputation survivors relying on a healthcare system whose baseline, pre-earthquake surgical, anesthesia, rehabilitation and prosthetic services were already severely limited.Reference Landry, O'Connell, Tardif and Burns5 These patients were at higher risk for medical complications, and access to rehabilitation services played an important role in terms of functional recovery, with associated implications for health-related quality of life and social reintegration.Reference Gosney6 In the setting of the ongoing crisis, resources for persons with amputations were strained even further and ethical considerations regarding distribution of services arose.Reference Merin, Nachman, Levy, Schwaber and Kreiss7 The disparities in quality of care received by Haitians with amputations highlights the necessity of multidisciplinary field guidelines to address the comprehensive medical needs of persons undergoing amputation in humanitarian emergency settings.
Where there is lack of evidence to define the delivery of medical care in field settings, the international humanitarian community generally relies on expert recommendations in the form of consensus statements or guidelines to direct such care. Given the unique challenges of each humanitarian crisis, such consensus statements or guidelines establish baseline standards of care in the face of disrupted health systems. They also facilitate the coordination between team members, and with other foreign teams and local responders. Development of consensus guidelines for international aid agencies, including surgical response teams, reflects the movement towards increasing professionalism standards in humanitarian response.Reference Keane, Pack, Greenough and Buckle8,Reference Bradt and Drummond9
During the 2009 Humanitarian Action Summit (2009 HAS), the Burden of Surgical Disease Working Group (BOSDWG)published the following recommendations on the provision of surgery in humanitarian settingsReference McQueen, Parmar, Keane and Broaddus10:
i. Understand the local context by conducting pre-program needs assessment
ii. Incorporate best practices in humanitarian delivery of surgery
iii. Incorporate data collection into humanitarian practice
Delivery of surgical care was specified to include “post-operative care and adequate follow-up including management of disability, (which) ensures the best possible care for the patient and serves as a means of quality assurance to guide changes to the program or procedure provided.”10 Consequently, a 2011 Surgical Issues Within the Humanitarian Space Working Group was formed in order to build on these statements and develop best practices for surgical care in disaster and conflict settings.
Given the surgical experience that followed the recent earthquake in Haiti, a separate 2011 HAS Amputations Following Disasters or Conflict Working Group was developed.
During the Summit, the goals and deliverables of the Amputation Working Group were to:
1. Review the literature and develop consensus on the multidisciplinary approach to limb amputation, rehabilitation and peri-operative support following disasters and conflict.
2. Define the role of international organizations (IO)/non-governmental organizations (NGO) and military medical services providing limb amputations in the field and establish consensus statements to encourage accountability, consistency, and quality of care of limb amputation patients in surgical humanitarian response.
Methods - Working Group Preparation
Published Literature Sources
A detailed literature review was conducted of current approaches to surgical limb amputation, perioperative pain control and rehabilitation of amputation patients in both disaster settings and conflict zones. The goals were to assess variations in surgical technique and analgesia for limb amputation patients and to determine the preoperative consideration given by surgical teams to the prosthetic fitting and rehabilitation of amputees in areas of disaster and conflict.
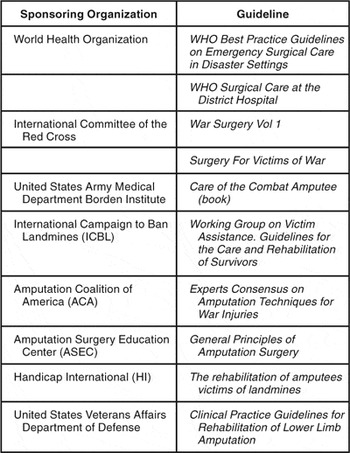
Current limb amputation guidelines published from the following organizations were also reviewed: the World Health Organization (WHO),11,12 the International Committee for the Red Cross (ICRC),Reference Gianou and Balden13,Reference Betrancourt, Dufour and Jensen14 the United States Army Medical Department Borden Institute,15 the International Campaign to Ban Landmines (ICBL) working group,16 the Amputation Coalition of America (ACA),17 the Amputation Surgery Education Center (ASEC),18 Handicap International (HI),19 and the Veterans Affairs Department of Defense Clinical Practice Guideline for Rehabilitation (VA/DoD) of Lower Limb Amputation20 (Table 1). The VA/DOD and the American Academy of Orthopedic Surgery (AAOS) recommendations on clinical practice guideline development were consulted as background reference material.21
Table 1 Summary of Guidelines Reviewed
Non-Literature Sources
The International Society of Physical and Rehabilitation Medicine's (ISPRM) WHO-Subcommittee on Rehabilitation Disaster Response (CRDR) provided substantive commentary to the working group introduced by the primary rehabilitation medicine representative (J Gosney). Since the earthquake in Haiti, core working group members engaged in online discussions in the months leading up to the 2011 HAS.
Methods - Working Group Sessions
During 2011 HAS, aworking group of invited experts convened in the fields of surgery, anesthesia, rehabilitation medicine, emergency medicine, mental health and family medicine to discuss the role of international organizations in providing multidisciplinary care to amputation patients.
Consensus building was centered on the role of international humanitarian organizations in providing management of amputations during disaster and conflict. To that end, related humanitarian recommendations and guidelines were also referenced, with the Haiti earthquake servicing as the focal crisis. The amputation working group developed statements during the consensus discussion based on an evaluation of the literature, current amputation guidelines, outside commentary, and the expert opinion of working group members as previously described. A summary of these statements is provided at the beginning of this article.
Discussion - Working Group Findings
Provision ofhumanitarian surgical care forlimb amputation extends beyond the technical considerations of when and how to operate. Working group members unanimously agreed that the medical care of limb amputation patients involves a comprehensive, multidisciplinary approach as the patient progresses from initial triage, pre-operative assessment and resuscitation to amputation, prosthetic fitting, rehabilitation and eventual community reintegration (Figure 1). Working group members also affirmed that humanitarian surgical responders should provide appropriate post-operative and follow-up care for amputation patients. Such care involves management considerations consistent with the care environment and available medical resources.

Figure 1 (Color online) Multidisciplinary approach to amputation patient
Within the broader surgical working group (see Surgical Issues Within the Humanitarian Space Working Group consensus), areas with particular significance for amputation care were identified:
- Team member composition
- Medical record keeping including consents and post-operative care
- Anesthesia and pain management
- Surgical technique and operative considerations
- Spectrum of rehabilitation services
- Patient follow-up and community reintegration
- Data tracking/ surgical outcomes reporting
Consensus Statements
1. Statement on Team Member Composition: The Multidisciplinary Surgical Response
Providing appropriate care to the patient undergoing amputation in the humanitarian setting means expanded planning for a multidisciplinary surgical care team. Along with surgical and anesthesia providers, this team should include access to, and early ongoing coordination with, personnel trained in rehabilitation and mental health services.
The decision to treat based on the potential for successful rehabilitation can be made as early as the moment of triage, as was evidenced at the Israeli Field Hospital in post-earthquake Haiti.Reference Merin, Nachman, Levy, Schwaber and Kreiss7 If appropriate resources are in place, such difficult ethical considerations are minimized. Therefore, access to and availability of rehabilitation services should be considered at all levels of the continuum of care of the amputation patient; ranging from the preoperative assessment, obtaining consent, post-operative prosthetic fitting and training, and extending to community reintegration. The 2011 Sphere Humanitarian Charter and Minimum Standards in Humanitarian Response Handbook reinforced that surgery provided without any immediate rehabilitation capabilities can result in a complete failure in restoring functional capacity of patients.22
The loss of limb is not the only impairment an amputation patient faces. Accompanying loss of loved ones and property, diminished earning capacity, ostracism, and psychological disturbance are common.23 Psychosocial support of amputated survivors in humanitarian emergencies should be facilitated by training and employing competent, locally based service providers who will provide culturally appropriate support and involve families in the recovery process.16 Particularly in areas of conflict and war, early mental health intervention and preventative psychiatric consultation are important in diminishing feelings of stigmatization experienced by military personnel.15
Recognizing limitations of personnel and resources, rehabilitation and psychosocial services should still be integrated as early as possible in the pre-deployment planning of international aid organizations and individuals providing amputations in austere settings. Local collaborating partners and referral relationships should be identified and established early, to ensure an uninterrupted transition from short to long-term convalescence.
2. Statement on Medical Record Keeping: Consent and Post-operative Care
It is essential that a medical record be established for all limb amputation patients undergoing care in a disaster setting or conflict zone. Due to the long-term and multidisciplinary nature of their recovery and follow-up, patient registration, clinical record keeping includingthe post-operative discharge plan arecriticalfor patients undergoing limb amputation. The lifelong implications of amputation must be effectively communicated when obtaining consent. The presence of rehabilitation professionals should be emphasized, as they are well qualified to properly describe the expectations in terms of functional recovery through prosthesis fitting.
Building on the minimum proposed standards of individualized, interpretable medical records, the importance of complete record keeping must be underscored in amputation patients who will have prolonged involvement in the local health system at multiple care sites. In particular, the post-operative plan should take into account that several providers with differing skill sets will be referring to this plan for managing the care of the patient and therefore needs to be clear and precise.
Before proceeding with any amputation, it is essential that patient and caregiver understand the rationale for performing amputation, and the possibility of additional intervention. Consent documents should be clear and easily interpreted, made available in Braille for the sightless, and supplemented with simple illustrations for the illiterate and in order to facilitate communication across language barriers. Additionally, consent for amputation in humanitarian settings is often fraught with significant cultural, personal, and psychological considerations. There is significant stigmatization surrounding amputation patients and certain populations are particularly vulnerable, including women, children, adolescents, and the elderly. They are likely to be reliant on outside decision makers regarding their care and may face increased challenges during recovery and community reintegration.Reference Gianou and Balden13
3. Statements on Providing Anesthesia and Appropriate Pain Management
Provision of effective anesthesia and analgesia for surgical care of limbamputation patients in a disaster setting or conflict zone is a fundamental human right. Pre-deployment planning for anesthesiologists must give rigorous attention to the equipment, pharmacy and support limitations that will be present in austere clinical settings. As such, total intravenous anesthesia (TIVA) and ultrasound based regional anesthesia techniques (USRA) may be ideally suited to the clinical care of limb amputation patients in disaster settings or conflict zones. Multimodal prevention and management of peri-operative somatic pain and phantom limb pain (PLP) remain priorities for these patients who will need to be successfully reintegrated into their communities with future, self-supporting livelihoods.
When possible, an anesthesiologist should be actively involved in the peri-operative care of patients presenting for limb amputation in disaster settings or conflict zones. This includes resuscitation, pre-operative assessment and optimization, intra-operative anesthesia care, post-operative critical care and peri-operative pain management. Disasteraffected patients presenting for evaluation of limb amputation are often trauma patients with other injuries. Maintaining a patent airway, effective ventilations and hemodynamic stabilization are first prioritiesfor any trauma patient presenting for amputation evaluation. Careful pre-operative evaluation is essential. Secondary trauma evaluation and management and attention to pre-existing medical co-morbidities, including “crush syndrome” must be considered when preparing a patient for limb amputation anesthesia and surgery.Reference Poçan24,Reference Oda25
Bestpractices for delivery of humane and competent anesthesia and analgesia must be provided even in difficult settings. Lessons learned from prior disasters, including Haiti, have revealed that delaying definitive surgery may sometimes be the wisest decision, especially when the patient can be stabilized and provided with antibiotics (for prevention of infection and gas gangrene) and pain management.Reference Missair, Gebhard, Pierre, Cooper, Lubarsky, Frohock and Pretto26 In the event that surgery must proceed, resuscitationis a priority, and appropriate anesthesia and pain management must be available. Limb amputation surgery in field hospital settings must never proceed in the absence of effective anesthesia (general or regional) and analgesia.
In the first days and weeks post crisis, anesthesiaagents and monitoring equipment may be scarce.Anesthesiology teams planning deployment to settings of humanitarian crises must proactively match equipment, pharmacy supplies and staff to the austere setting in which they will be providing clinical care. Complex pneumatic or electronic anesthesia machines for delivery of mixed oxygen and nitrous oxide gases and volatile anesthetic agents for general anesthesia require backup gas cylinder supplies, scavenging methods and biomedical support that may not be available in the disaster setting. Anesthesia and analgesia for limb amputation in disaster settings and conflict zones may be accomplished by a number of methods including volatile general anesthesia, TIVA, central neuraxial anesthesia (epidural or spinal) and regional anesthesia techniques facilitated by peripheral nerve stimulation (PNS) or those that are ultrasound guided.Reference Buckenmaier27 TIVA via portable, battery-operated infusion pumps may be a cost-effective, safe and practical anesthesia delivery system for amnesia and hypnosis in austere settings. Regional anesthesia techniques, including central neuraxial and peripheral upper and lower extremity blocks, have benefits for intra-operative amputation surgery and post-operative pain management in resource-limited settings. They minimize hemodynamic changes as compared to central neuraxial or general anesthesia approaches but require provider clinical skill and competence. The anesthesia provider performing regional anesthesia must be appropriately trained, should have an understanding of the plexus anatomy and be competent in the diagnosis and management of potential complications that may result from injection of large volumes of local anesthesia drugs into perineural spaces including local anesthesia toxicity (LAT) particularly in pregnant and pediatric patients.Reference Neal28
Likewise, ultrasound-based regional anesthesia techniques (USRA) can now be provided with small, portable, battery-operated ultrasound machines appropriately suited for use in austere clinical settings. Such compact ultrasound machines are being increasingly utilized for clinical diagnostic purposes in the field. USRA allows for regional blockperformance where limb loss precludes the ability to observe a motor response to PNS.Reference Betrancourt, Dufour and Jensen14
Effective analgesia is a fundamental human right and is possible even in low-resource settings if considered early as a component of surgical mission planning.Reference Size, Soyannwo and DM29–Reference Brennen, Carr and Cousins31 Pain control is a ratelimiting step in the recovery of amputation patients. In areas where sophisticated anesthetic practices are limited, parenteral ketamine can be an effective medication for both anesthesia and analgesia in amputation surgery.Reference Craven32,Reference Bonanno33 Ketamine can provide several hours of post-operative pain relief, but thereafter supplementation with opioids, local anesthesia or other adjuncts will be required.Reference Schnittger34,Reference Hayes35 Ketamine has been shown to reduce severity of chronic phantom limb pain (PLP), though it does not reduce occurrence.15
Chronic post-operative pain such as PLP and residual somatic or persistent stump pain can limit prosthesis fitting, impair mobility and functional recovery and contribute to isolation and suffering.23 In low-resource settings, PLP management is often based on transient supplies of medications from the international organization providing care. Suitable treatment options should be part of the WHO's List of Essential Medications.36 At present, available agents targeting such neuropathic pain include ketamine, lidocaine, acetaminophen, nonsteroidalantiinflammatories, opioids [provider administered and, where appropriate, via patient-controlled analgesia (PCA)], tramadol, antidepressants, and anticonvulsants. There is convincing evidence that an around-the-clock regimen of NSAIDs, selective COX-2 inhibitory blockers, and/or acetominophen is helpful in the post-operative period.37,Reference Bone38
PLP prevention is an important consideration in planning care for limb amputation patients. In the US, 70% of patients undergoing limb amputation, for various indications, experience PLP and 50% still experience PLP 5 years after surgery.Reference Bloomquist39
Regional anesthetic blockade in the form of continuous peripheral nerve blocks and epidural catheter placement may also interrupt transmission in the nocioceptive pain pathway of phantom limb pain. For lower limb revascularization procedures, a Cochrane database review found that there was insufficient evidence to show important differences in outcome for neuraxial anesthesia compared to general anesthesia.Reference Barbosa40 Of note, there are rare reports of recurrence of PLP in patients with previous amputation subsequently provided epidural anesthesia for non-amputation surgery.Reference Martin41 Ultimately, epidurals are likely inappropriate in settings of disaster and conflict. They may cause hypotension, apnea (if narcotics are used or the epidural migrates into the intrathecal space) and paraspinal infections (since strict sterile technique is unlikely in these settings). Unintended flashbacks and nightmares after orthopedic and vascular surgery under neuraxial anesthesia have also been reported.Reference Scheman42
Peripheral nerve blocks can also be used in crisis situations as they can serve as the sole anesthetic intraoperatively, postoperatively to control pain with minimal hemodynamic change, and for repeat procedures such as debridement or amputation revisions and wound care. The United States military has strongly advocated for the importance of peripheral nerve blocks in war trauma care.Reference Buckenmaier43
Multimodal therapy, even in disaster and conflict settings, is the standard of care for phantom limb pain.15,23 In addition to medications, non-pharmacological options are feasible in the humanitarian setting and include heat application, stump massage, transcutaneous electrical nerve stimulation (TENS), or mirror therapy. Mirror visual feedback is a technique whereby vision of the reflection of the intact limb can help in movement of the phantom limb.Reference Ramachandran, Rogers-Ramachandran and Cobb44–Reference Ramachandran and Altschuler46
Statements on Surgical Technique and Operative Considerations for Amputations
The surgical care provider must recognize that there is an early window of opportunity for limb salvage. Surgical decision-making regarding amputations must account for limitations in supplies, availability of blood for transfusion, technical expertise, availability of rehabilitation services and prostheses, as well as cultural implications for the patient. If and when the decision of amputation is made, the goal is to optimize function by preserving appropriate limb length. War injuries present differently from those incurred by civilians during disaster and may require more staged intervention. Guillotine amputation is rarely indicated except as a last resort for emergency extrication and should not be used as a stand-alone solution.
One of the lessons from Haiti, more so than any previous earthquake or natural disaster, is that many patients received amputations as a primary intervention for complex severe wounds and fractures which could potentially have been salvaged.Reference O'Connell, Shivji and Calvot47 Amputations as secondary treatment for infected wounds and compartment syndromes were also reported in high numbers even though this is not the standard of care.Reference O'Connell, Shivji and Calvot47 Significant volumes of guillotine amputations were performed as a “life saving intervention” or when technical expertise was limited, subsequently requiring revision at higher levels.Reference O'Connell, Shivji and Calvot47 These patients’ rehabilitation potential was typically negatively affected by poor surgical indication, timing and technique.
Every effort should be made to optimize resuscitation and wound management in the early stages of limb injury. Limb conservation may sometimes simply require appropriately timed administration of antibiotics, regular dressing changes and wound debridement, or a straightforward arterial suturing technique.Reference Betrancourt, Dufour and Jensen14 In humanitarian disaster and conflict, amputation is often hastily performed as way of removing significant amounts of damaged tissue and saving a life, without consideration for more conservative techniques. Humanitarian surgical providers are encouraged to adhere to, as much as possible, conventional indications for amputation while in the field. These include severe mangling of extremities, overwhelming infection, established gangrene and secondary hemorrhage uncontrollable by other measures.Reference Betrancourt, Dufour and Jensen14 As a last resort, amputations may be necessary in crisis zones for rescue of entrapped casualties.15
Regardless of setting, there are overarching principles of amputation surgery that help to plan for appropriate surgical technique. They are to (1) optimize wound healing, (2) optimize prosthetic fit and (3) to optimize functional ability.Reference Betrancourt, Dufour and Jensen14 Therefore, amputations should be at the most distal level still compatible with wound healing and subsequent satisfactory prosthetic fitting.18 The guiding principles of operative technique are open amputation through healthy tissue, preserving as much length and as many joint levels as possible, and delayed fashioning of flaps and primary closure to obtain a clean, well padded and well balanced stump, in the least amount of procedures.Reference Betrancourt, Dufour and Jensen14,15,17,18,20 The initial amputation should control infection and be followed by a definitive amputation; conservation of bone length and leaving muscle bellies intact minimizes post-operative swelling.18
The group debated the definition of appropriate limb length in terms of prosthetic fitting and functional recovery. For an above knee amputation, this was felt to be between the middle and distal third of the thigh. For a below knee amputation, it was believed to be better between the distal third and proximal third of the leg. Below knee amputation is generally better than above knee (i.e., preservation of joint levels). Through knee amputation is better than above knee amputation because of better weight-bearing potential. Through knee amputation may be preferable to below knee if appropriate below knee length cannot be ensured. In general, short stumps make it difficult to control prosthesis, increases energy requirements and consequent muscle fatigue, which impacts on muscle shortening, weight bearing, alignment and cosmesis.15,18,20 Other factors to be considered when choosing the level of amputation include the availability of technology (through knee prosthesis might not be available while temporary above knees are), as well as maintaining a balance between expected functional recovery, cosmesis and the patient's expectations.
It is also important to recognize that the pathophysiology of limb injuries is significantly different in war and conflict than in natural disaster. During war, bullets, blasts or mine injuries frequently involve extensive soft tissue damage due to the high-energy impact of the initial trauma. In evacuating the area of immediate danger or conflict, open wounds often become infected. Injury may involve extended compartmental injury, frequently necessitating higher levels of amputation to control infection and allow for bone coverage.Reference Gianou and Balden13 The aim is to avoid amputation revision, so definitive reconstructive procedures are often done later once the soft tissue envelope has stabilized.17
With improvements in military medicine, Forward Surgical Teams are often prepared to transport victims efficiently to Deployable Rapid Assembly Shelters, even in the most high acuity war zones. Orthopedic surgeons on site are equipped to provide appropriate primary amputations with staged reconstruction.Reference O'Connell, Shivji and Calvot47
Historically, wartime amputations were performed in a guillotine fashion, which involved cutting skin, soft tissue and bone at the same anatomical level using a circumferential skin cut.11,12,Reference Gawande48,Reference Clasper49 This technique is no longer advocated in military medicine, as it is not significantly quicker than amputations excising non-viable tissue, and often leads to complications such as infection due to exposed bone, compromised bone length, wound infection and poor prosthetic fitting.Reference Gianou and Balden13–21,Reference Clasper49
Similarly, we believe that guillotine surgery should be avoided in the setting of disaster. Amputations as a consequence of natural disasters are most frequently seen post-earthquake, whereby victims are injured or even trapped under debris leading to “crush syndrome.” This syndrome is caused by a combination of direct muscle injury, muscle ischemia and muscle cell death as a result of prolonged pressure on the limbs or torso. Acute renal failure is often precipitated by the release of myoglobin. Despite the haste to save lives and potentially extricate the injured from rubble, most victims can be spared guillotine amputation and afforded a function-preserving approach with delayed primary closure.
Statement on the Spectrum of Rehabilitation Services
Optimal rehabilitation of the traumatic amputee requires a comprehensive approach that considers medical/surgical, physical rehabilitation, psychosocial and community integration interventions. Appropriate, effective surgical care requires interdisciplinary team assessment and management involving rehabilitation providers from prior to surgery through community referral and follow-up. Due to the relative lack of rehabilitation providers and the acuity of crisis settings with the resulting need for taskshifting, surgical providers should understand general, key principles of amputation patient rehabilitation. The patient's family, other caregivers and the community also must be actively involved in providing multi-layered rehabilitation across the continuum of care.
Amputation rehabilitation interventions are indicated during each phase of care - preoperative, acute post-operative, pre-prosthetic, prosthetic training and long-term follow-up to achieve optimal functional outcomes and improved quality of life. Ideally, a comprehensive, interdisciplinary, patient-centered treatment plan is developed early in the rehabilitation course and updated throughout all phases; interdisciplinary team assessment and management is practiced throughout the plan of care accordingly. Key disciplines can include physiatry, surgery, physical therapy, occupational therapy, prosthetics, nursing, mental health, nutrition, recreational management and social work services. Specialty surgery, internal medicine, pain management, vocational therapy and spiritual advisors may be consulted as well. Since most of these specialty providers are not available in a disaster or conflict setting, on-scene responders must provide essential surgical and rehabilitation services under existing conditions.
Given the likely absence of trained rehabilitation providers at the disaster scene, adequate pre-operative assessment could be performed by a qualified team member (such as a broad spectrum nurse or a generalist or surgeon with good understanding of rehabilitation issues related to amputation surgery). Ideally, the operating surgeon performs the appropriate amputation at the selected level and adheres to appropriatesurgical principles. The choice of amputation level should consider the patient's general condition, the risk of additional surgeries, the potential for healing of the limb, the fitting of the prosthesis and the probable functional outcome. Good surgery maximizes patient rehabilitation potential.
Immediate post-operative rehabilitation management includes appropriate pain control, wound care and residual limb management. Interventions include therapeutic positioning and mobilization to prevent contracture; bandaging and massage reduces postoperative edema and protects the amputated limb from external trauma, ensuring patient safety.19 Once the patient is medically stable, rehabilitation efforts aimed at discharge from acute care include improving the amputee's range of motion, strength, balance, mobility and ability to perform activities of daily living (ADLs).19 Therapeutic emphasis is placed on achieving maximum independence as quickly as possible to meet the anticipated demands of the amputation patient's home and local environment.
The amputation patient should be discharged with a comprehensive follow-up plan of carethat includes wound management, residual limb management and referral to prosthetic and orthotic (P&O) services for an evaluation. Device appropriateness depends on patient factors including medical status, functional goals, motivation, cultural acceptance and social support, and availability of P&O resources in the crisis- affected area.Reference Mannion and Chaloner50,Reference Cummings51 If the patient is a suitable candidate for prosthesis, pre- and post-prosthetic care involves appropriate bandaging and physical and functional physical rehabilitation to ensure proper use of the assistive device, maximum functional status, prevention of secondary injury and effective pain management.16 The amputation patient may be provided additional durable medical equipment (DME) such as a wheelchair, walker, or crutches to facilitate mobility and ADLs.19 Ongoing evaluation is required to ensure optimal patient medical status, device fit and function, adequate activity and participation in the community and patient satisfaction. Psychosocial support and family and caregiver involvement is necessary to achieve best outcomes.
One of the most important factors in providing successful rehabilitation services in the humanitarian setting is effective partnering with pre-existing local organizations. On-the-ground presence of prosthetists in disaster and conflict settings is essential, as each prosthesis requires appropriate fitting and cannot simply be brought along as a donation from the organization delivering care.
Prosthetic, orthotic and associated rehabilitative therapy services were limited in Haiti prior to the 2010 earthquake. Operated by Healing Hands for Haiti (HHH), the primary full-production P&O facility (in Port-au-Prince, about 100 limbs per year) was effectively destroyed in the earthquake and the salvageable machinery used in starting a new workshop in partnership with Handicap International (HI). Since Haiti had no accredited training programs for rehabilitation professionals, high level P&O expertise was provided by international non-government organization expatriates who supervised locally trained Haitian P&O technicians, physical therapists and rehabilitation technicians. HHH administered rehabilitation technician training programs, along with Health Volunteers Overseas (HVO) (in partnership with Hospital Albert Schweitzer) and the Center for Eucharistic Heart and Modern Rehabilitation, a Cuban organization. In fact, most of the estimated 30-40 physical therapists in Haiti were trained in Cuba or the Dominican Republic.Reference Lisa, Iezzoni, Laurence and Ronan52
The Inter-Agency Standing Committee (IASC), a unique inter-agency forum for coordination, policy development and decision-making involving key UN and non-UN humanitarian partners, employs the “cluster” approach as a means of enhancing predictability, response capacity and coordination and accountability in delivering humanitarian assistance by strengthening partnerships in key sectors of humanitarian response. Following the earthquake, HI and Christian Blind Mission (CBM) were appointed as co-leads of the UN-WHO/PAHO Health Cluster's Injury Rehabilitation and Disability(IR&D) Workgroup (“disability subcluster”) and officially partnered with the Secretariat for the Inclusion of Persons with Handicaps (SEIPH) of the Government of Haiti's Ministry of Public Health and Population (GoH-MSPP) to coordinate the rehabilitation response for Haiti's newly injured and disabled person. The SEIPH focused on the needs of the pre-existing disabled whereas the IR&D primarily addressed the humanitarian emergency rehabilitation response. Rehabilitation responders were strongly encouraged to register with the IR&D, attend meetings, monitor the group's and health cluster's online presence and actively participate in general. Adherence to relevant P&O humanitarian programming guidance53–57 and a code of conduct for NGO P&O providers58 was emphasized to foster accountability to global standards for the provision of devices and mobility aids in low-resource settings.
Within days of the earthquake, HI's emergency response team had begun conducting a rapid assessment of the incidence and initial hospital and community management of disabling traumatic injuries (including fractures, amputations, spinal cord injuries, traumatic brain injuries, burns and polytrauma) in the greater Port-au-Prince area. Objectives included identifying and evaluating the postoperative care, acute rehabilitation interventions, discharge and referral procedures and community interventions to determine the most appropriate strategies to address the overwhelming need for rehabilitative care.37
The post-earthquake rehabilitation services response was significant as indicated by self-reported summary data from 27 provider organizations including about 15 P&O service providers (for the period January 12 – November 30, 2011): 1800 artificial limbs, 2000 braces, over 4500 wheelchairs and nearly 10,000 walking aids; nearly 26,000 received physical therapy and almost 37,000 received counseling (unofficial compilation). Coordination of P&O services and associated rehabilitation, however, proved extremely challenging due to the variability of provider experience, practice and capacity. Several organizations expressed interest with good intentions but lacked necessary experience and qualifications. Achieving an effective distribution of services within the earthquake-affected area and beyond proved an ongoing challenge as well. P&O services currently appear to meet identified demand.
Delivery of rehabilitative services was significantly complicated by difficulty locating and following up with patients in the community. Many amputees were initially discharged from acute care facilities having received no rehabilitation or related instruction and with no plan for post-operative care to include referral for rehabilitation services. Some hospitals subsequently established post-operative hospitals, to free higher acuity beds, and outpatient clinics for wound care and fracture management. Rehabilitation INGOs, including HI and CBM, helped locate these patients in the community and arranged for hospital and community follow-up. However, participation in the prescribed course of rehabilitative care was not possible for many patients who relied on family and caregivers that were preoccupied with the daily struggle for survival; others had lost family and homes and did not have reliable access to transportation.36
The prevailingculture of disability in Haiti whereby affected persons are thought contagious and considered worthless also discouraged participation in therapy by those who feared contaminationand being stigmatized.Reference Ingstad and Reynolds White59 Increasing societal acceptance of disability as a natural condition which can be improved by rehabilitation60 has resulted in more persons with pre-existing disabilities, including amputees, seeking treatment. This phenomenon coincides with the clinical shift toward rehabilitation of chronic conditions that reflects the general transition of the humanitarian medical response from acute emergency to long-term recovery.
Increased focus on health sector recovery and development has gradually translated into improved rehabilitation services infrastructure. Recognizing the significant need for more skilled rehabilitation workers, HHH, HVO and Partners in Health (PIH)/ZanmiLasante have expanded or developed their rehabilitation technician training programs. Incorporating elements of community-based rehabilitation61, these programs align with the Sphere Minimum Standards For Humanitarian Care Delivery guidance that “partnership with community-based rehabilitation programs can optimize the post-operative care and rehabilitation for injured survivors.”23 Most P&O providers in Haiti support the Hispaniola Prosthetics and Orthotics Education (HiPOE) training initiative54 which will result in accreditation of local technicians to provide appropriate quality P&O services.Reference Jacobson58 Increased local capacity will reduce dependence on expatriate support, thereby contributing to more sustainable P&O service programming. Upgraded facilities infrastructure is typified by the newly reconstructed HHH rehabilitation center, an American/Norwegian Red Cross funded project which employs ICRC-Special Fund for the Disabled (SFD) material, technical and educational support.61 The proposed Haiti national rehabilitation plan recommends increased facility infrastructure including a national center for treatment of traumatic injuries, including amputation, in addition to departmental P&O facilities and supporting community services.
Delivery of rehabilitation services following the 2010 Haiti Earthquake has clearly demonstrated to the humanitarian community the value of designating “disability” as a focus area under the UN cluster system coordination mechanism. Formal sharing of IR&D leadership responsibilities between disability INGOs and a host government disability agency as well as active coordination of human and material rehabilitation resources by the IR&D greatly facilitated the delivery of rehabilitation services in the field. Moreover, this significant operational effort has enabled the initial development of a national rehabilitation system in Haiti. For the traumatic amputee in post-earthquake Haiti, early post-operative rehabilitation with provision of prostheses and associated therapy has increased survival and reduced long-term disability,23 thereby contributing to better functioning andgreaterindependence with improved quality of life.
Statement on Discharge Planning and Follow-Up
Clear post-operative discharge planning and follow-up course should be delineated for each amputee. Optimizing function prior to release from the hospital will provide the best potential for outpatient recovery. Patient and family education opportunities must be recognized.
Disorganized discharge and referral patterns of amputees in post-earthquake Haiti raised concerns regarding the welfare of these patients, many of who were displaced and left homeless. Despite caseload burden and disrupted infrastructure in hospitals, several facilities showed that it was possible to collect patient registration and discharge data, as well as to provide bookings for return appointments.36 Partnerships with local organizations such as Handicap International facilitated outpatient follow-up within the community.
Discharge plans should include the location of rehabilitation, financial considerations, home environment assessment, transportation capabilities, vocational and educational considerations.20 There are no clinical trials providing evidence for the need for life-long care or specifying frequency of follow-up.23 Patients at higher risk for complications should be identified to minimize risk of amputation revision. Though challenging in humanitarian settings, care providers should arrange for at least one follow-up visit in the year following amputation.20 Long-term follow-up involves assessing the patient's stump and prosthesis over time. Quality of life is dependent on concurrent psychological rehabilitation and community re-integration, which may include vocational and educational training.23 The Veteran's Association has developed detailed programs encouraging return to service for combat amputees.15,Reference Potter and Scoville62
Statement on Surgical Outcomes Specific to Amputation
In order to move toward improved humanitarian surgery data collection, there are surgical outcomes specific to amputation that should be developed. We considered the following:
Operative: wound infection, wound dehiscence, number of operative procedures, number of stump revisions, limb length Post-operative: pain control, time to initiation of rehabilitation, use/satisfaction of prosthesis, use of assistive technologies, completion of activities of daily living
In the context of developing a minimum dataset for surgical epidemiologic reporting in humanitarian settings, we propose a preliminary set of reportable outcome measures relevant to amputation surgery. The Limb Loss Research Statistics Program developed through the United States Army is a preliminary attempt at measuring outcomes following upper extremity amputation in conflict settings.15 Details on wound healing and complications for amputations can be tracked in a similar fashion to the ICRC wound database and registry.Reference Betrancourt, Dufour and Jensen14 It is important to consider whether limb length was appropriate for the prosthetic being fitted. The number of operative procedures performed prior to stump closure and final limb length are decent indicators of whether complications occurred. Similarly, the number of stump revisions performed after the primary stump is healed should be minimized. In combination with time to initiation of rehabilitation, we are provided with an assessment of the patient's post-operative course. A standardized nonverbal pain scale such as the WHO pain ladder can be used to measure pain control.Reference Charlton63
Suggested Strategies and Next Steps
During the 2011 HAS, the Surgical Working Subgroup on Amputations Following Disasters and Conflictdeveloped multidisciplinary consensus statements for amputation, post-operative management and rehabilitation following disasters and conflict. Further discussion between invested international aid organizations and other humanitarian stakeholders including international medical professional societies and the World Health Organization (WHO) is required. The upcoming stakeholder panel during the ISPRM WHO-Subcommittee on Rehabilitation Disaster Response (CRDR) sponsored symposium on disaster rehabilitation relief (held during the 6th ISPRM World Congress in San Juan, Puerto Rico, June 2011) and the WHO Disability and Rehabilitation (DAR) Professional Organizations Initiative meeting in (Geneva, June 2011) are two appropriate venues. Additionally, Handicap International will participate in an upcoming symposium on AmputationDuring Natural Disaster during the upcoming International Society of Orthopedic Surgery and Traumatology World Congress (Prague, September 2011). A dedicated international consensus conference may be indicated.
Such discussions will help formalize our consensus statements into multidisciplinary practice guidelines with the aim of improving the quality of management of amputations in humanitarian settings. Preliminary steps are already being taken by the newly proposed Emergency Surgery Coalition, a consortium of surgical providers aiming to standardize and maximize delivery of humanitarian surgical assistance.Reference Chu64 Development of uniform multidisciplinary guidelines will compel the humanitarian surgeon and surgical team to observe a higher professional standard of care. Most importantly, life-saving amputations during crisis will grant patients more satisfying, productive lives and help establish a healthier post-crisis society.
Conclusion
Ample discussion within the humanitarian community is required in order to identify and promote best practices for multidisciplinary amputation care in disaster and humanitarian emergencies. The 2011 HAS Amputation Working Group has presented recommendations in the areas of team planning, medical record keeping, operative technique, pain management, rehabilitation, follow-up and outcomes tracking. Further dialogue is needed in each of these areas and will move us toward the evidence base required for advancing surgical care delivery during crises.
Increasingly, the responsible humanitarian surgeon will be required to understand not only surgical principles of amputations, but also to be mindful of what lies beyond the operating theatre for each patient: a lifelong battle with pain control, functional recovery and psychosocial reintegration. Multidisciplinary care must be planned and prepared for even in the post-disaster and conflict setting. Without working towards a full spectrum of care in low-income settings, a life may be initially saved byamputation surgery, but lifelong disability is certain. The time is now to continue this discussion, and to plan for the next disaster or conflict that will call us to action.
Abbreviations:
ADL = activity of daily living
CBM = Christian Blind Mission
HAS = Humanitarian Action Summit
HI = Handicap International
ICRC = International Committee of the Red Cross
IO = International Organizations
ISPRM = International Society of Physical and Rehabilitation Medicine
NGO = non-government organizations
P&O = prosthetic and orthotic
PLP = phantom limb pain
TIVA = total intravenous anesthesia
WHO = World Health Organization




