Introduction
The accurate and standardized assessment of the severity of injury is as an essential prerequisite, both to effective trauma care and timing of clinical intervention. Reference Champion, Sacco, Copes, Gann, Gennarelli and Flanagan1–Reference Baker, O’Neill, Haddon and Long4
Trauma patients are triaged out-of-hospital and at emergency department (ED) admission by evaluating physiological parameters. Several trauma scoring systems have been developed for trauma severity stratification and mortality prediction. Reference Wutzler, Maegele, Wafaisade, Wyen, Marzi and Lefering3 Revised Trauma Score (RTS) and its Triage version (T-RTS) proved to be easy to obtain and effective, and they are commonly used in clinical and research settings on trauma. Reference Manoochehry, Vafabin, Bitaraf and Amiri5–Reference Nakhjavan-Shahraki, Yousefifard and Hajighanbari8
Although T-RTS is reliable and widely validated, several proposals have been made to improve its accuracy. The New Trauma Score (NTS) adopted Glasgow Coma Scale (GCS) score instead of code, a revision of systolic blood pressure (BP) interval and the use of peripheral oxygen saturation (SpO2) instead of respiratory rate (RR). Reference Jeong, Park and Kim9 The NTS proved to be slightly superior to RTS in trauma mortality prediction, however, the calculation formula is very complex to be used in triage or prehospital settings. A simplified version of NTS proposed for triage was not compared to T-RTS, and neither has been independently validated. Reference Jeong, Park and Kim9 Similarly, the triage-directed trauma score Mechanism, GCS, Age, and Arterial Pressure (MGAP) demonstrated an overall Receiver Operating Characteristic (ROC) area under curve (AUC) not significantly different from T-RTS. The MGAP proved to be slightly more accurate than T-RTS, only setting a higher cut-off point, allowing an estimated under-triage of approximately 0.5%. Reference Sartorius, Le Manach and David10 The Kampala Trauma Score (KTS) is widely used in low-income countries for trauma stratification and triage, Reference Kobusingye and Lett11 but it did not prove to be superior to RTS in a recent meta-analysis. Reference Manoochehry, Vafabin, Bitaraf and Amiri5 Finally, some authors proposed to add Albumin determination to RTS score (RTS-A) to improve its accuracy. Reference Kim, Kim and Kim12 The so obtained RTS-A score proved to be more accurate than standard RTS, however, the study did not propose a triage version of the score and the albumin determination is hardly achievable in prehospital and triage settings.
Increased blood glucose level (BGL) is often observed in trauma Reference Kreutziger, Lederer and Schmid13 due to a stress-induced adrenergic mediated metabolic reaction Reference Bar-Or, Rael and Madayag14,Reference Dungan, Braithwaite and Preiser15 and is associated to high trauma severity, to higher morbidity and mortality, Reference Yendamuri, Fulda and Tinkoff16–Reference Rau, Wu and Chen21 and to susceptibility to infectious complications. Reference Bochicchio, Bochicchio, Joshi, Ilahi and Scalea22
Determination of BGL has been proposed as a tool for rapid assessment of the severity of trauma, Reference Paladino, Subramanian, Nabors, Bhardwaj and Sinert17,Reference Savić, Cernak, Jevtić and Todorić23 and a BGL higher than 200mg/dL (11.1mmol/L) was reported to be a reliable predictor of mortality, independent of injury characteristics, Reference Laird, Miller, Kilgo, Meredith and Chang18,Reference Sung, Bochicchio, Joshi, Bochicchio, Tracy and Scalea19
This study was aimed to assess if in trauma patients, a combined evaluation of both BGL and T-RTS at ED admission may help to provide a more accurate and effective prediction of the actual clinical outcome, both in the general population and in the elderly, compared to T-RTS alone.
Methods
This is a single-center, retrospective cohort study conducted in the ED of an urban teaching hospital, which is a referral trauma center. The average ED admission rate is 75,000 patients per year, approximately 30% of which are trauma-related access.
The clinical records of all the patients consecutively admitted to the ED for trauma over a three-year period (2016-2018) were reviewed.
Exclusion criteria were: known diagnosis of diabetes, age <18 years old, pregnancy, mild trauma (classified as isolate trauma of upper or lower limb, in absence of exposed fractures), and those in which BGL at ED admission were not available.
In addition to demographics, for each patient, were evaluated:
-
Type of ED Referral: Self-referred or transported by Emergency Medical System;
-
Context of Trauma: Road, domestic, sport, work, violence, or other;
-
High- or Low-Energy Trauma: Based on the mechanisms of injury – high-energy trauma was defined as fall from height greater than two meters, ejection from a vehicle or difficult extraction, motorbike accident, pedestrian investment, major fracture, first rib fracture, penetrating trauma, or amputation;
-
T-RTS Score: Calculated at admission;
-
BGL: At ED admission;
-
Physiological Parameters: BP, SaO2, heart rate (HR), RR, GCS, and body temperature;
-
Laboratory Values: Hemoglobin, Creatinine, blood urea nitrogen (BUN), Fibrinogen, and Prothrombin time (PT); and
-
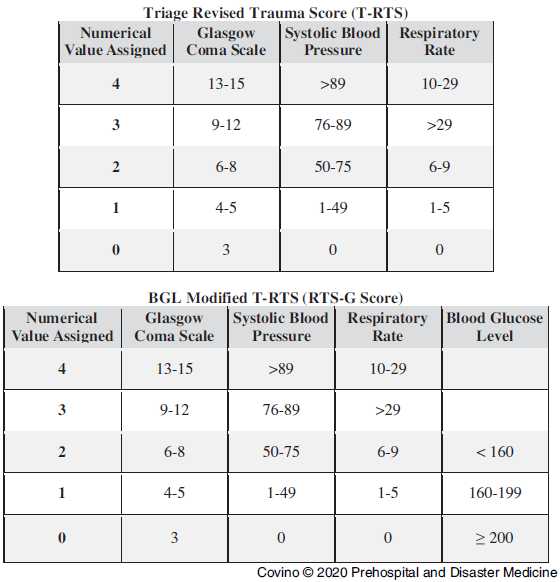
Combined Revised Trauma Score Glucose (RTS-G) Score: Obtained as shown in Figure 1, adding to T-RTS: two for BGL <160mg/dL (8.9mmol/L); one for BGL ≥160mg/dL and <200mg/dL (11.1mmol/L); and zero for BGL ≥200mg/dL.

Figure 1. Calculation Criteria for Triage Revised Trauma Score (T-RTS) and Proposed Blood Glucose Level (BGL) Modified T-RTS (RTS-G).
Outcome Measures
The primary outcome was a composite of patient’s death in ED or admission in intensive care unit (ICU).
The criteria for ICU admission during the study period included circulatory shock requiring vasopressors and the need for positive pressure respiratory support, including non-invasive ventilation. High-flow oxygen treatment is provided in general wards. The ICU admission criteria were consistent throughout the study period.
Statistical Analysis and Sample Size
Continuous, not normally distributed variables are reported as median [interquartile range] and compared at univariate analysis by Mann-Whitney U test or Kruskal-Wallis ANOVA test, as appropriate. Categorical variables are reported as absolute number (percentage) and compared by Chi-square test.
Significant parameters at univariate analysis were entered in a logistic regression model in order to identify the independent predictors of adverse outcome. Since physiological parameters are included in the T-RTS, any of these were entered in the logistic model in order to avoid analysis redundancy. Logistic regression results are expressed as Odds Ratio (95% confidence interval).
Receiver Operating Characteristic curve analysis was used to evaluate the overall performance of T-RTS and of the combined RTS-G score to predict the defined adverse outcome. This ROC curve analysis was performed separately for all the study cohort, only for patients ≥65 years, and was used to estimate sensitivity and specificity at different score threshold values. The comparison between the ROC AUCs was made according to previously described method. Reference DeLong, DeLong and Clarke-Pearson24 A P value ≤.05 was regarded as significant. Data were analyzed by SPSS v25 (IBM Corp; Armonk, New York USA).
Considering the 5.6% rate of adverse outcome in BGL <200mg/dL and the 25.4% rate of adverse outcome in BGL ≥200 mg/dL patients, the study population largely outnumber the 562 patients needed for univariate estimation (setting β error = 0.1 and α error = 0.05). Similarly, considering the 12 degrees of liberty of the multivariate model, at least 120 events (deaths or ICU admissions) would have been needed for the analysis. Thus, the study cohort is adequate for the multivariate parameters estimation.
Statement of Ethics
This study has been approved by the local Ethics Committee and has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Due to its retrospective design on anonymous database, the need of informed consent was waived.
Results
In the three-year study period, a total of 68,933 injured patients were admitted for trauma in the ED. Among these, 59,455 were classified as mild trauma, and in 42 cases, BGL values were not available. Thus, the study population consisted of 9,436 patients (4,407 females) aged from 18 to 103 years old. Of these, 4,288 patients were aged ≥65 years (Table 1).
Table 1. Demographic Characteristics of Enrolled Patients

Note: Data are shown for all populations and according to age group. Categorical variables are presented as number (%); continuous variables are presented as median [interquartile range].
Abbreviations: BGL, blood glucose level; BP, blood pressure; BUN, Blood Urea Nitrogen; ED, emergency department; GCS, Glasgow Coma Scale; ICU, intensive care unit; PT, Prothrombin time; RTS, Revised Trauma Score; SaO2, peripheral oxygen saturation.
The admission BGL of the overall studied population was 108 [96 - 129] mg/dL (6.0 [5.3 - 7.2] mmol/L). Admission BGL was significantly higher in elderly patients at P level <.001 (Table 1).
Approximately one-third of traumas occurred as road accidents and one-third in the domestic setting (Table 1). As expected, the distribution of trauma settings was different in young and elderly patients, being the young were more often involved in road accidents and the elderly were more often involved in domestic trauma (Table 1).
The physiological, clinical, and laboratory characteristics of the study cohort and the distribution in each age group is reported in Table 1.
Overall, 38 patients died in ED (0.4%) and 539 patients were admitted to ICU; consequently, a total of 577 (6.1%) patients met the primary combined endpoint of the study (Table 2).
Table 2. Study Variables and their Association with Primary Composite Outcome (Death or ICU Admission)

Note: Categorical variables are presented as number (%); continuous variables are presented as median [interquartile range].
Abbreviations: BGL, blood glucose level; BP, blood pressure; BUN, Blood Urea Nitrogen; GCS, Glasgow Coma Scale; ICU, intensive care unit; PT, Prothrombin time; SaO2, peripheral oxygen saturation.
Several parameters were associated with death or ICU admission at univariate analysis (Table 2). Among trauma characteristics, younger age, male sex, road accident, and high-energy trauma were associated to a worse outcome. Conversely, the self-referred patients had almost invariably good outcomes. Among the physiological parameters, BP, HR, and GCS had a significant association with death or ICU admission; on the other hand, neither body temperature nor SpO2 were associated with worse outcome. A T-RTS score <12 was a very good predictor of the cumulative adverse outcome.
Among the laboratory parameters evaluated, elevated BGL showed a significant association with worse prognosis. Similarly, so did hemoglobin values, serum creatinine, fibrinogen, and PT (Table 2).
To enter BGL values in the multivariate models, cut-off values were used to dichotomize this continuous variable. The cut-off values were chosen according to previously published papers Reference Sung, Bochicchio, Joshi, Bochicchio, Tracy and Scalea19 and by a further evaluation made by the ROC analysis of BGL values in the study population. Specifically, values were selected that had a specificity >90% and >95%, respectively, for poor outcome. The chosen values were BGL ≥160mg/dL and BGL ≥200mg/dL.
When entered in the multivariate model, most of the evaluated parameters were independently associated with adverse outcome (Table 3). Of note, high-energy trauma and T-RTS showed the highest OR (respectively, 27.40 and 9.65), followed by elevated BLG with OR of 3.85 for BGL >160mg/dL and 4.51 for BGL >200mg/dL.
Table 3. Multivariate Analysis for Parameters Associated to Adverse Outcome at Univariate Analysis
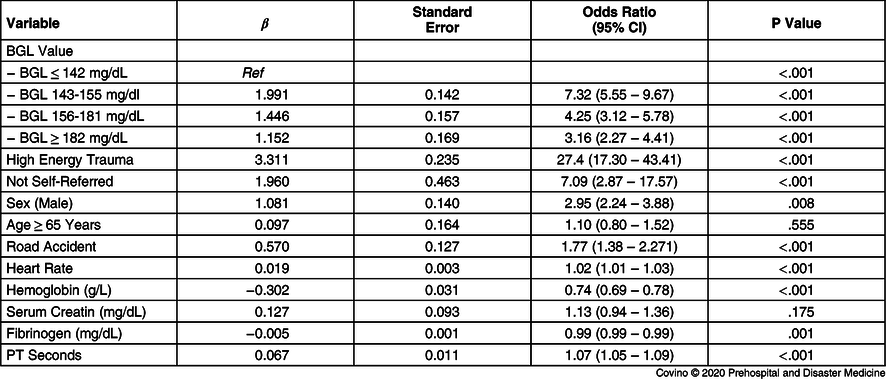
Note: Logistic regression model had an overall predictive value of 94.3%; Model β2 was 1051.8 (P <.001); –2 log likelihood was 2223.9; goodness of fit (Hosmer-Lemeshow) β2 was 9.9 (P = .271). Constant was included into the model.
Abbreviations: BGL, blood glucose level; PT, Prothrombin time.
The T-RTS showed a good ROC AUC for association to adverse outcome, both in general population and in patients ≥65 years (Figure 2). The cumulative RTS-G score was significantly more accurate than T-RTS and reached the best accuracy in elderly patients. In general population, ROC AUC for T-RTS was 0.671 (95% CI, 0.661 - 0.680) compared to RTS-G ROC AUC 0.743 (95% CI, 0.734 - 0.752); P <.001. In patients ≥65 years, T-RTS ROC AUC was 0.671 (95% CI, 0.657 - 0.685) compared to RTS-G ROC AUC 0.780 (95% CI, 0.768 - 0.793); P <.001 (Figure 2).

Figure 2. ROC Curve Analysis of T-RTS and RTS Combined with BGL (RTS-G), with Respect to Adverse Outcome Defined as Death in ED or ICU Admission.
Note: In general population, ROC AUC for T-RTS was 0.671 (95% CI, 0.661 - 0.680) compared to RTS-G ROC AUC 0.743 (95% CI, 0.734 - 0.752); P <.001. In patients ≥65 years, T-RTS ROC AUC was 0.671 (95% CI, 0.657 - 0.685) compared to RTS-G ROC AUC 0.780 (95% CI, 0.768 - 0.793); P <.001.
Abbreviations: AUC, area under curve; BGL, blood glucose level; ED, emergency department; ICU, intensive care unit; ROC, Receiver Operating Characteristic; RTS, Revised Trauma Score; RTS-G, Revised Trauma Score Glucose; T-RTS, Triage Revised Trauma Score.
In the study population, a RTS-G ≤13 had sensitivity 58.2% [54.1 - 62.3] and specificity 88.3% [87.6 - 88.9] for death or ICU admission. Table 4 shows sensitivity and specificity for RTS-G and T-RTS at different threshold values, both for the general and the elderly populations.
Table 4. Sensitivity and Specificity for Death or ICU Admission at Different Score Threshold Values

Note: Data are shown for T-RTS and RTS-G score obtained combining T-RTS and BGL values, as shown in Figure 1. A high sensitivity consents the identification of more patients at risk (reducing under-triage), whereas a high specificity reduces the risk of over-triage. Both T-RTS and RTS-G have high specificity; RTS-G performs significantly better in terms of specificity. Sensitivity and specificity values are presented as value [95% confidence interval].
Abbreviations: BGL, blood glucose level; ICU, intensive care unit; RTS-G, Revised Trauma Score Glucose; T-RTS, Triage Revised Trauma Score.
Discussion
The main finding of this study is that the proposed RTS-G score, obtained combining BGL and T-RTS (Figure 1), is superior to T-RTS in general population, and it is particularly accurate in elderly population.
The T-RTS takes into consideration three clinical items (GCS, systolic BP, and RR), scoring each parameter from one to four points/from high to low severity (Figure 1). Using the so obtained 12 points T-RTS score in the triage procedures, a trauma patient with a T-RTS = 12 may be labeled as “delayed,” whereas for T-RTS ≤12 should be considered urgent or for immediate care. Reference Champion, Sacco, Copes, Gann, Gennarelli and Flanagan1,Reference Manoochehry, Vafabin, Bitaraf and Amiri5 The standard version of RTS combine GCS, systolic BP, and RR into a weighted sum (RTS = 0.937 GCS + 0.733 BP + 0.291 RR, with a possible range from 0.0 to 7.84). However, the RTS is not as simple to calculate as T-RTS in triage and prehospital settings. Reference Champion, Sacco, Copes, Gann, Gennarelli and Flanagan1 Moreover, based on the analysis made on a large trauma cohort, it has been suggested that T-RTS could replace the RTS as the standard physiologic severity score for trauma outcome prediction. Reference Moore, Lavoie and Abdous7
Glucose level has long been routinely determined by prehospital rescue teams and ED triage operators by finger stick rapid tests, mainly in unconscious and in diabetic patients. Reference Degroote and Pieper25 The physiological bases of BGL determination in trauma patients is that in critical illness, the metabolic stress leads to the synthesis of adrenocorticotrophic hormone, glucagon, catecholamine, to active glycogenolysis, and to increased insulin resistance. All these conditions could lead patients to hyperglycemia. Reference Bar-Or, Rael and Madayag14,Reference Dungan, Braithwaite and Preiser15
Several studies reported that elevated BGL in patients with traumatic injuries were associated with worse outcomes. Reference Yendamuri, Fulda and Tinkoff16–Reference Bochicchio, Bochicchio, Joshi, Ilahi and Scalea22,Reference Bochicchio and Scalea26–Reference Sperry, Frankel and Vanek28 Furthermore, non-diabetic patients with major injuries showed significantly higher BGL on admission to ED, and the study suggested that high glucose levels could be as good as base deficit and lactate levels in the identification of major injury. Reference Paladino, Subramanian, Nabors, Bhardwaj and Sinert17 Moreover, it has been reported that BGL at admission could predict the development of hemorrhagic shock more precisely than other laboratory parameters such as admission hemoglobin, lactate, standard base excess, pH, bicarbonate, or vital parameters. Reference Sung, Bochicchio, Joshi, Bochicchio, Tracy and Scalea19 In prehospital settings, high BGL was correlated to the need of ICU admission and life-saving interventions Reference Glassberg, Lipsky and Lending29 and was found to be a predictor of cardiac rhythm instability. Reference Kreutziger, Schmid and Umlauf30
This study suggests that severe trauma is able to exert a significant stress-induced, adrenergic-mediated, hyperglycemic effect, and patients with high BGL values need more often ICU admission or were deceased in ED (Table 2). The multivariate analysis confirmed that BGL ≥160mg/dL and BGL ≥200mg/dL were independent predictors of poor outcome, respectively, with odds ratios of 3.85 and 4.51 (Table 3).
An optimal triage tool should have good sensitivity to detect as many cases at risk as possible, avoiding a dangerous under-triage. At the same time, it is advisable to reach a high specificity in order to reduce the over-triage, which unnecessarily increases the use of ED resources.
Besides T-RTS and BGL, several variables were independently associated with worse outcome in the study cohort. As expected, lower hemoglobin and fibrinogen values, higher PT values, and HR were all independent predictors of death or ICU admission (Table 3). These hemorrhage and coagulopathy-related parameters, together with male sex and high-energy trauma, are well-known and recognized factors of poor outcome. Reference Abu-Zidan31,Reference Winearls, Campbell and Hurn32 However, among these factors, the only suitable for triage use could be the report of a high-energy trauma. This latter variable, however, is difficult to standardize and often led to a consistent over-triage. Reference Tominaga, Dandan, Schaffer, Nasrallah, Gawlik and Kraus33 For instance, if applied as triage factor in the study cohort, it could produce a five-fold over-estimate of urgent patients. For this reason, it was excluded as a possible adding to the score and a case-by-case evaluation should be made for reported “high-energy-trauma” patients.
The adding of BGL to RTS resulted in the cumulative RTS-G which performed significantly better than T-RTS in general population, and reached the best ROC AUC in patients ≥65 years old. In particular, the analysis demonstrated that RTS-G had an overall specificity similar to T-RTS at different threshold values and compared to T-RTS resulted in an estimate over-triage of approximately five percent of cases (Table 4). Interestingly, although specificity was similar, RTS-G outperformed T-RTS in terms of sensitivity and the score was able to reduce under-triage of approximately 20% in general population and up to 23% in elderly (Table 4). As a result, the RTS-G could address the response of ED staff and trauma team identifying 20% more patients at-risk compared to standard T-RTS with a minimal increase in over-triage.
Study Limitations
Although conducted in a very large cohort of trauma patients, this study presents some limitations. First, its retrospective design cannot provide conclusive data about the efficacy of RTS-G to improve the outcome of trauma patients. Moreover, information about the time from last meal of investigated patients was not collected, and similarly the time from trauma to ED presentation was unknown. These latter biases, however, are randomly distributed among all the study population, far limiting the confounding effect.
Finally, the primary outcome measure (death in ED or ICU admission) is different from overall intra-hospital death or death at 30 days that are often used as primary end-points in most of the previous study on trauma predictors. However, while this choice can limit the evaluation of the data, it does not affect the comparison between T-RTS and RTS-G in the same study cohort. Moreover, this triage score was evaluated with respect to an early endpoint, since the late mortality in trauma could indeed be influenced by several factors, most of which could not be ascertained at the initial trauma evaluation.
Conclusions
Data from this study suggest that at ED admission, RTS-G could be used effectively for the risk stratification of traumatized patients in the place of T-RTS. The analysis reveals that the combined RTS-G score performs significantly better than T-RTS and gives best results in patients ≥65 years.
However, the retrospective design of the study cannot respond to the key question in this setting, that is if the RTS-G could improve the clinical management and ultimately the prognosis of trauma patients. Prospective studies and external validation are needed to define this point.
Conflicts of interest
none