Introduction
Pulse rate is a key vital sign that can help a 911 dispatcher determine a patient's status, what type of help that patient will need, and how quickly help is needed. 1 Previous studies have looked at a pulse check only as a validator of cardiac arrest and a precursor to the initiation of cardiopulmonary resuscitation (CPR).Reference Bahr, Klingler, Panzer, Rode and Kettler 2 - Reference Walcott, Melnick and Walker 4 Cummins et al evaluated the ability of the untrained layperson to check a pulse in unconscious and/or non-breathing/unresponsive patients, and recommended elimination of pulse checking by laypersons as a criterion for determining the need for CPR, due to the fear of false-positive errors.Reference Cummins and Hazinski 5 Eberle et al demonstrated that recognition of pulselessness in potential cardiac arrest patients by first responders with basic CPR training was time-consuming and, 40% of the time, inaccurate.Reference Eberle, Dick, Schneider, Wisser, Doetsch and Tzanova 3 In addition, Bahr et al assessed the ability of layperson-callers with first aid (including CPR) training to check carotid pulse on young, healthy, non-obese, and conscious persons by counting aloud the detected pulse rate.Reference Bahr, Klingler, Panzer, Rode and Kettler 2 They reported that a longer time interval is needed to detect correct carotid pulse than the five seconds 6 or five to 10 seconds 7 reported by the American Heart Association (AHA) and the European Resuscitation Council (ERC) guidelines, respectively.
In a multi-center study involving medical students, paramedics, and emergency medical technicians (EMTs), less than 10% of the medical students and ambulance personnel were able to detect a simulated carotid pulse in a manikin.Reference Flesche, Breuer, Mandel, Breivik and Tarnow 8 On average, the medical students took four seconds to detect a pulse in a conscious, apparently healthy, volunteer. Approximately eight percent of the medical students could not detect the pulse within 120 seconds.
The hypothesis of this study was that, when instructed by a trained emergency medical dispatcher (EMD), using the scripted Medical Priority Dispatch System (MPDS) protocol Pulse Check Diagnostic Tool (PCDxT), a layperson-caller can detect a carotid pulse and accurately determine the pulse rate in a conscious person. Therefore, the objective of this study was to establish whether a layperson-caller can (a) successfully detect a pulse, and (b) accurately determine a patient's pulse rate.
Methods
Design and Setting
This non-randomized and non-controlled prospective cohort study was conducted in three large public locations (i.e., library, university, and high school) in Salt Lake City, Utah (USA). A booth was set up outside the library to enlist volunteers. At the university, the study was conducted within the student service center, and opened to any volunteering student. The high school subjects comprised students from a health class and an English as Second Language class. Study data was collected from September 2010 through March 2011 (library: September 7, 2010; university: November 29, 2010; and high school: March 17-18, 2011). The study was approved by the International Academies of Emergency Dispatch Institutional Review Board.
Pulse Checking Process
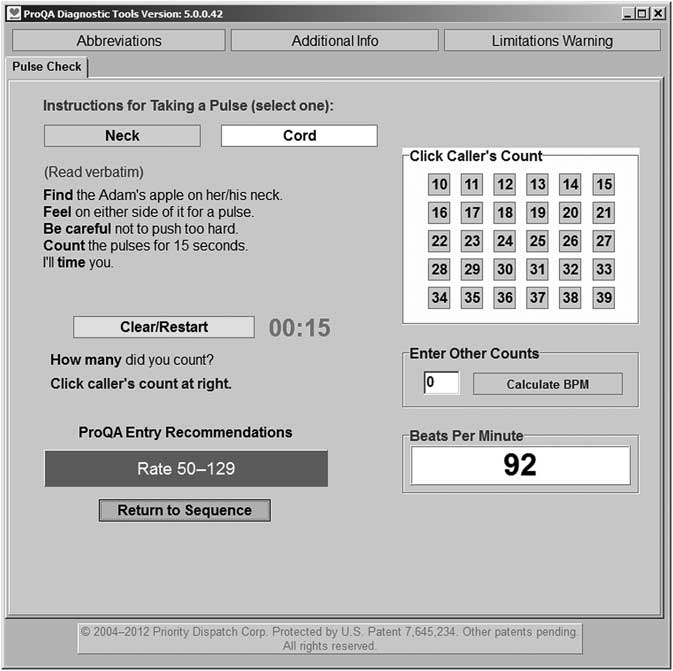
Before each study participant was invited into the study room, the Investigator used an electrocardiogram (ECG) monitor (handheld ECG Monitor MS-7420, Medsource International, LLC, Mound, Minnesota USA) to obtain a mock patient's pulse rate. The pulse rate obtained using the ECG monitor was a standard measure to compare with the values obtained by the layperson-caller for accuracy. Volunteers, enlisted as layperson-callers, were invited into the study room, one by one. Each layperson-caller then initiated a phone call to a certified EMD call-taker. The EMD used the scripted information in the MPDS's PCDxT (Figure 1) to instruct the layperson-caller how to perform a carotid pulse check on the patient and obtain a pulse rate. Using a stopwatch, the investigator determined the time taken by the layperson-caller to detect a pulse.

Figure 1 The Medical Priority Dispatch System Protocol Pulse Check Diagnostic Tool
Once the pulse was found, the EMD timed the layperson-caller for 15 seconds as the layperson-caller counted beats aloud or silently. At the 15-second mark, the EMD instructed the layperson-caller to report the number of beats counted. The EMD then used the PCDxT to calculate the patient's pulse rate in beats per minute (bpm), multiplying the number of beats reported by four. The rate was recorded as the layperson-caller-measured rate. The entire process was repeated for each layperson-caller.
Outcome Measures
The primary endpoints were the time taken to find the patient's pulse, the number of times the layperson-caller was able, or not able, to find the pulse, and the pulse rate accuracy (estimated by comparing the patient's pulse rate obtained by the layperson-caller with that obtained by the investigator using the attached ECG monitor). Other outcome measures were the percentage of pulse rates obtained by the layperson-caller within an eight beat margin of error, and those within the 50-130 bpm normal range (as defined in the MPDS). The eight beat margin of error was based on a mathematical measurement limitation. Since pulse rate was assessed (using the PCDxT) in a 15-second period only, there was a potential eight beat calculation error because of small variations in the precision of the cut-off points.
Data Analysis
STATA for Windows software version 11.2 (STATACorp, College Station, Texas USA) was used for data analysis. Fisher's exact test was used, along with odds ratio (OR) with 95% confidence interval (CI), to assess associations between categorical measures. The Student t test was used to test mean differences between continuous measures. Spearman's correlation coefficients were used to assess the accuracy of the patient's pulse rate determined by layperson-callers when compared to the (standard) rate obtained using the ECG monitor. All differences were tested at a .05 level of significance. Mock patients and layperson-callers were profiled, and stratified by gender, age, and study site. The proportions of layperson-callers who found a pulse as instructed by the EMD were also tabulated, and gender and mean age differences were assessed. The age of layperson-callers who found the patient's pulse was compared with the age of those who did not. Other analyses evaluated gender and age differences among layperson-callers who obtained patient's pulse rate within the 50-130 bpm normal range and within the eight beat margin of error.
The accuracy (differences between pulse rate obtained using the ECG monitor and those obtained by layperson-callers) of pulse rate obtained within the eight beat margin of error, by layperson-callers, was assessed using Spearman's correlation coefficients. Comments and/or recommendations to improve the MPDS protocol were also presented.
Results
Characteristics of Study Patients and Layperson-Callers
The study involved 11 mock patients (54.6% female), mean age 41.4 years of age (SD = 9.9 years), with 123.3 (SD = 12.2) and 70.8 (SD = 10.5) mean systolic and diastolic blood pressures, respectively. A total of 268 layperson-callers (44.0% female) participated in the study (Table 1), of which 248 (92.5%) found the patient's pulse. A majority, 99.2% (246/248) of layperson-callers complied with the EMD-provided pulse check instructions. Out of the 246 layperson-callers, 50.0% obtained a pulse rate within an eight beat margin of error. Layperson-callers were on average 20.1 years of age (SD = 8.7) (library: 36.2 years (SD = 11.3 years); university: 22.0 years (SD = 4.5 years) and high school: 15.9 years (SD = 0.8 years)). Males were significantly older than females at the university, library, and overall.
Table 1 Characteristics of mock patients and layperson-callers

aTwo-sided Fisher's Exact and Student t-test P values comparing site difference in the categorical measurements and mean layperson-caller's age, respectively.
bSome blood pressure data missed.
Abbreviation: SD, standard deviation.
Finding Patient's Pulse
Male layperson-callers who detected a patient's pulse were significantly older than the females (P = .001), but time to detect a pulse did not differ significantly by gender (Table 2). Overall, 87.8% of layperson-caller-obtained pulse rates were within the 50-130 bpm normal range (high school: 84.5%; library: 94.7%; university: 93.5%).
Table 2 Layperson-callers who found pulse as instructed by the EMD

aTwo-sided Fisher's Exact and Student t-test P values comparing site difference in the categorical measurements and mean layperson-caller's age, respectively.
bUndeterminable due to small sample size.
Abbreviations: EMD, emergency medical dispatch; SD, standard deviation of layperson-caller's age from the mean age; OR, Odds Ratio; CI, Confidence Interval.
Some layperson-callers had problems locating the patient's pulse. Some lost the pulse in the middle of counting, while others withdrew fingers or excessively eased pressure from the patient's neck when asked “not to press too hard.” A few layperson-callers could not follow EMD instructions adequately to complete the process, due to a language barrier. One layperson-caller stopped counting after 15 beats, instead of 15 seconds. Others looked for their own pulses or looked elsewhere than the patient's neck, and some had multiple unsuccessful attempts at finding a pulse. Additionally, some layperson-callers did not know what a pulse was or felt like, or believed female patients did not possess an Adam's apple. A few layperson-callers said the EMD's instructions were ambiguous; one suggested that a description should be provided as to what a pulse should feel like.
Pulse Rate Obtained within an Eight Beat Margin of Error
Male layperson-callers who obtained a pulse rate within the eight beat margin of error were significantly older than females, at the library (P = .023) and overall (P = .001) (Table 3). A borderline association (P = .050) existed between study site and a likelihood of a layperson-caller obtaining a pulse rate within the eight beat margin of error (high school: 47.2%; library: 68.4%; university: 45.7%).
Table 3 Characteristics of the layperson-callers who obtained pulse rate within an eight beat margin of error

aTwo-sided Fisher's Exact and Student t-test P values comparing site difference in the categorical measurements and mean layperson-caller's age, respectively.
Abbreviation: CI, Confidence Interval; SD, standard deviation; OR, Odds Ratio.
Time Taken by Layperson-Callers to Find Patient's Pulse
The overall median time to detect a pulse was 15 seconds (high school: 12 seconds; library: 19 seconds; university: 20 seconds), while the highest percentage took 20 seconds or less (Table 4). Layperson-callers who determined pulse rates within the eight beat margin of error took a median 14 seconds (high school: 11 seconds, library: 18 seconds, university: 17 seconds) to detect a pulse.
Table 4 Time (in seconds) taken by layperson-caller to find pulse of the patient

aPercentage of cases in respective study sites.
Abbreviations: HS, high school; Lib, library; Univ, university.
Accuracy of Pulse Rate Obtained by Layperson-Callers
There was an overall 94.6% correlation between pulse rates obtained using the ECG monitor and the rate by the layperson-callers. The correlations were significantly high by site (Figure 2a; high school: 89.6%, library: 85.2%, university: 81.0%; P < .001 each), gender (Figure 2b; female: 93.1%; male: 95.0%; P < .001 each), and age (Figure 2c; 15-16 years: 89.5%; 17-18 years: 92.2%; 19-20 years: 96.3%; >20 years: 86.1%; P < .001 each).

Figure 2a Box plots of pulse rates determined within 8 bpm margin of error using the ECG monitor and by layperson-caller, by site
Abbreviations: bpm, beats per minute; ECG, electrocardiogram.

Figure 2b Box plots of pulse rates determined within 8 bpm margin of error using the ECG monitor and by layperson-caller, by gender
Abbreviations: bpm, beats per minute; ECG, electrocardiogram.

Figure 2c Box plots of pulse rates determined within 8 bpm margin of error using the ECG monitor and by layperson-caller, by age
Abbreviations: bpm, beats per minute; ECG, electrocardiogram.
Discussion
This study demonstrates that layperson-callers, when given specific instructions over the telephone, can find a carotid pulse and accurately determine a pulse rate of a conscious person (as observed by the very high correlation coefficients). While at least one other studyReference Cummins and Hazinski 5 has examined this possibility, that study did not include the expert-scripted, MPDS instructions provided by a trained EMD. These EMD-provided instructions proved to be reliable in directing the layperson-caller on where and how to find a pulse (next to the Adam's apple, feel with two fingers, etc). Somewhat less reliable was the ability of the layperson-caller to count each of the pulses for the entire fifteen-second interval. This number was reported accurately—by the measure of the eight beat margin of error (i.e., two beats in a fifteen second count)—approximately 50% of the time. A layperson-caller result of eight beats above or below the ECG reading was considered to be a fully accurate result, since the pulse count went for only 15 seconds, and the caller-reported count was multiplied by four to get the pulse rate. A caller may subjectively count, or not count, a single pulse beat at the start and/or end of the 15 seconds because the command from the EMD to start or stop counting may come right at the moment a beat is felt. Several participants reported to the investigators that they had this experience when measuring pulse counts.
The primary goal of the PCDxT in the MPDS is to classify a patient into one of two clinical categories: patients with a pulse rate of 50–129 bpm, and those that fall outside of this range (i.e., <50 bpm or ≥130 bpm). The MPDS Heart Problems/Automatic Implanted Cardiac Defibrillator (AICD) chief complaint comprises three priority levels: ALPHA (low acuity cases), CHARLIE (moderate acuity cases) and DELTA (high acuity cases). 1 The MPDS assigns an ALPHA-level priority to asymptomatic patients who have a pulse rate within the ≥50 and <130 bpm range. A CHARLIE-level priority is assigned to patients outside of this range. In most Emergency Medical Services (EMS) systems, a CHARLIE-level case will receive an urgent or emergency response from an Advanced Life Support (ALS) crew. An ALPHA-level case will generally receive a lesser response, often from a Basic Life Support (BLS) crew only. Since the clinical categorization of ALPHA contains a relatively wide range between high-and low-end pulse rates, a small error in determining an actual pulse rate from the layperson-caller would not change the priority level in the vast majority of cases.
Several observations made during the study suggest where the EMD instructions could be improved to increase layperson accuracy. At times, the research team observed layperson-callers repositioning or removing their pulse-checking fingers from the patient's neck as soon as the EMD stated the instruction “Be careful not to push too hard.” Subsequently, those layperson-callers had difficulty in finding a pulse and, in some cases, counting the beats. The authors suggest this particular instruction be removed from the MPDS script or merged with the first instruction of “Find the Adam's apple on her/his neck” to read “Without pushing too hard, find the Adam's apple on her/his neck.” None of the test patients reported that the layperson-callers were pressing too hard. In some instances, the layperson-caller asked the patient if s/he was pressing too hard, and the patients universally responded “No.” This study also validated the findings of a previous studyReference Bahr, Klingler, Panzer, Rode and Kettler 2 that a layperson-caller may actually require a longer time interval to detect correct carotid pulse than the five seconds 6 or five to 10 seconds 7 reported by the AHA and the ERC guidelines, respectively.
Layperson-callers did not always inform the EMD when they had found the pulse—a necessary signal to the EMD to start the 15-second timer. The pulse script could potentially be improved by adding the following statements: “Tell me when you have found her/his pulse,” and “Count the beats out loud so I can time you, starting now.” The investigators also observed several instances where the layperson-caller checked his or her own pulse, and not the patient's pulse. However, this does not appear to be a weakness in the MPDS script (the instruction to take the pulse of the patient is clearly stipulated), but rather a case of mock patient/role-playing confusion on the part of a few layperson-callers not understanding the part that the mock patient played in the simulated emergency call. It is doubtful that, during a true emergency call, there would be any confusion as to whom the patient is, and the intent to have the layperson-caller find the patient's pulse rate.
Some layperson-callers placed their thumbs right on the Adam's apple, a few placed their hands horizontally across the Adam's apple, and some located the Adam's apple with both hands. An instruction should be included for layperson-callers to use two fingers in finding the Adam's apple.
Limitations
Because pulse rate can change quickly over a short period of time, one limitation of this study was that the patient's pulse was not measured concurrently (using the ECG monitor) as the layperson-caller counted the pulse and reported the count to the EMD. The authors decided that a concurrent measurement with the monitor on the patient would encourage cheating, and would be too intrusive, taking away from the intended effect of simulating a true emergency call. Another limitation was the simulation environment itself, which was not a completely convincing depiction of a medical emergency. Additionally, because the patients were healthy, not sick, their actual pulse rates were mostly within a normal pulse rate range, making it impossible to measure how accurate a layperson-caller would be when checking for the pulse and determining the pulse rate of patients with bradycardia, tachycardia, or other actual dysrythmias. True emergency callers may also be under more duress, making it harder for them to adequately follow instructions from the EMD or report findings.
Conclusion
This study demonstrated that layperson-callers, when instructed over the phone by a trained 911 Emergency Medical Dispatcher using the MPDS PCDxT, can find a pulse and accurately determine a pulse rate of a conscious, healthy subject. Improvements to the specific MPDS PCDxT instructions may increase the accuracy of layperson-caller pulse rate determination. Future research is recommended involving true emergency calls.
Abbreviations
- AHA:
-
American Heart Association
- BPM:
-
beats per minute
- CPR:
-
cardiopulmonary resuscitation
- ECG:
-
electrocardiogram
- EMD:
-
emergency medical dispatcher
- ERC:
-
European Resuscitation Council
- MPDS:
-
Medical Priority Dispatch System
- PCDxT:
-
Pulse Check Diagnostic Tool
Acknowledgments
The authors thank Bailee Newbold for her services as a trained EMD. We are grateful to Mike Veenendaal at Valley Emergency Communications Center, for allowing Bailee to participate. We thank JoDee Hilton for logistics management and subjects’ recruitment, and the study-site administrators for their permission and cooperation. Thanks to Matt Bishop, Bruce Tenney, Holly Clark, Chris Knight, Cindy Grigg, Bob Henderson, Alyssa Whitney, and Dawn McBride for being mock patients. The same goes to all Priority Dispatch Corp. staff who participated in study pretesting. Finally, we thank Salt Lake City Fire Department, through Chief Brian Dale, for providing ECG monitors.