Introduction
Trypanosoma vivax is a hemoprotozoan that survives in the blood plasma of its hosts and has been causing damage to beef and dairy cattle producers in various regions of the world (Oliveira et al., Reference Oliveira, Hernández-Gamboa, Jiménez-Alfaro, Zeledón, Blandón and Urbina2009; Bastos et al., Reference Bastos, Faria, de Cavalcante, de Madrid, Zapa, Nicaretta, Cruvinel, Heller, Couto, de Rodrigues, Ferreira, Soares, Cadioli and Lopes2020a; Chávez-Larrea et al., Reference Chávez-Larrea, Medina-Pozo, Cholota-Iza, Jumbo-Moreira, Saegerman, Proaño-Pérez, Ron-Román and Reyna-Bello2020). Regarding the mode of transmission of this parasite to cattle, in Africa it occurs with the participation of biological vectors such as the tsetse fly (Glossina spp.), while in Central and South America, it occurs by mechanical vectors such as horseflies (Tabanidae) (Otte and Abuabara, Reference Otte and Abuabara1991), and iatrogenic (Dagnachew and Bezie, Reference Dagnachew and Bezie2015; Bastos et al., Reference Bastos, Faria, de Madrid, De Bessa, Linhares, Fidelis Junior, Sampaio, Cruz, Cruvinel, Nicaretta, Machado, Da Costa and Lopes2017).
Among these types of transmission of T. vivax to cattle, the iatrogenic route stands out, through the reuse of syringes and needles among animals. From the trypanosomosis outbreaks described in the literature, they occurred in Girolando dairy cattle, after the introduction of new animals to the herd, associated to the use of medication sharing the same syringe and needle between animals as the predisposing factor for the occurrence of the disease (Guerra et al., Reference Guerra, Feitosa, Santos, Abreu-Silva and Dos Santos2008; Silva et al., Reference Silva, Costa, Polenz, Polenz, Teixeira, Lopes and Monteiro2009; Cadioli et al., Reference Cadioli, de Athayde Barnabé, Machado, Teixeira, André, Sampaio, Fidélis, Teixeira and Marques2012; Pimentel et al., Reference Pimentel, do Nascimento Ramos, do Ramos, de Araújo, Borba, da Gloria Faustino and Alves2012; Andrade Neto et al., Reference Andrade Neto, Afonso, Mendonça, Souto, André and Machado2015; Costa et al., Reference Costa, Abreu, Machado, Thomé, Massard, Santos and Brito2016; Bastos et al., Reference Bastos, Faria, de Madrid, De Bessa, Linhares, Fidelis Junior, Sampaio, Cruz, Cruvinel, Nicaretta, Machado, Da Costa and Lopes2017; Vieira et al., Reference Vieira, de Macedo, Santos, Silva, de Mendonça, da Gloria Faustino, do Nascimento Ramos, Alves, Ramos and de Carvalho2017; Lopes et al., Reference Lopes, da Prado, Martins, Beserra, de Sousa Filho, de Evangelista, de Cardoso, Mineiro and de Souza2018). Although not recommended, the reuse of the same syringe and needle is common. A manual issued by the US Department of Agriculture (2011) reports that approximately 85% of producers reuse the needle on different animals, with 32% using the same needle on 11–30 bovines.
Although the iatrogenic pathway is important in the epidemiology of T. vivax transmission to cattle, especially where there are no vectors, there are still doubts related to this issue that need to be clarified. The first would be how many cattle could be infected by different routes (subcutaneous, intramuscular and intravenous) reusing the same syringe and needle from an animal with the acute phase of T. vivax. The other would be whether T. vivax is able to survive on different injectable veterinary drugs, and for how long. These gaps need to be answered, so it will be possible to better understand the importance of the iatrogenic pathway to propagate T. vivax in cattle herds.
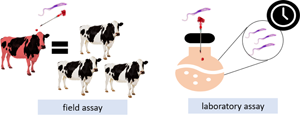
The present study verified how many cattle could become infected with T. vivax, by subcutaneous, intramuscular and intravenous routes, using the same syringe and needle, from an animal with an acute infection of this protozoan. In addition, the viability of T. vivax in injectable veterinary drugs, belonging to different classes of drugs (antibiotics, antiparasitics, reproductive hormones, vitamin complex and their derivatives, vaccines, anaesthetics, anti-inflammatory/antipyretics, antitoxics).
Materials and methods
Trypanosoma vivax inoculum
For the field and laboratory assays, samples of T. vivax were thawed and inoculated into two bovines for each study to be kept as a donor (Girolando breed, 5 months of age) at the location where the study was conducted. The inoculum of T. vivax used was the Ipameri strain (Bastos et al., Reference Bastos, Faria, de Madrid, De Bessa, Linhares, Fidelis Junior, Sampaio, Cruz, Cruvinel, Nicaretta, Machado, Da Costa and Lopes2017 – Genbank accession code MK392089), which is kept cryopreserved (8% glycerol) in liquid nitrogen at the Center for Veterinary Parasitology of the Veterinary and Husbandry School of the Federal University of Goiás, Goiânia, Brazil. For the inoculum acquisition, a portion of a frozen blood sample with high T. vivax parasitaemia was thawed in a water bath for 5 min. After determining its viability under an optical microscope, 4 mL of blood containing about 3 × 106 trypomastigotes per mL was inoculated in a bovine for inoculum expansion. Daily, the parasitaemia of the infected bovine was accompanied by blood collection to visualize the protozoan using Brener (Reference Brener1961) methodology. On D0, at least one bovine had about 1 × 106 trypomastigotes per mL in the blood sample.
Experiment 1 (field assay): iatrogenic transmission of Trypanosoma vivax by different routes
Two repetitions (R1 and R2) of the animal stage were performed, conducted from February to April 2020 (R1), and from January to March 2021 (R2). In each of these repetitions, 35 male calves (Bos taurus indicus, Girolando) were used as recommended by Reinbold et al. (Reference Reinbold, Coetzee, Hollis, Nickell, Riegel, Christopher and Ganta2010). These animals had approximately 10 months of age at the start of the study and were purchased from a commercial farm free of T. vivax located in the municipality of Inhumas, state of Goiás, Brazil, 45 km from the state capital of Goiania.
The cattle arrived at the University's cattle sector, on day −30, where they were kept in the period of acclimatization until the beginning of the study. During the entire experimental period, the cattle were kept on Brachiaria brizanta pasture and water ad libitum. The acclimatization period was 30 days (from D −30 to D −1). Before day 0 of the study, blood samples were then collected from the calves for T. vivax parasitological diagnosis using Woo, Brener, blood smear and conventional PCR (Brener, Reference Brener1961; Woo, Reference Woo1970; Cortez et al., Reference Cortez, Rodrigues, Garcia, Neves, Batista, Bengaly, Paiva and Teixeira2009), on days −30, −10, −3, −2 and −1. On arrival day at the experimental site on D −21, all calves received a specific medication for helminths (albendazole 5 mg kg−1, Valbazen®, Zoetis), a spray with a combination of alpha cypermethrin + chlorpyrifos + ethion (Potenty®, MSD Saúde Animal) for tick control and, orally, toltrazuril 15 mg kg−1 (Baycox®, Elanco Saúde Animal) against Eimeria spp.
On D0 of the study, for each repetition (R1 and R2), animals were distributed into four groups: T01 = animals that received, subcutaneously, saline solution with the same syringe and needle contaminated by T. vivax from the donor animal (n = 10); T02 = animals that received, intramuscularly, saline solution with the same syringe and needle contaminated by T. vivax from the donor animal (n = 10); T03 = animals that received, intravenously, saline solution with the same syringe and needle contaminated with T. vivax from the donor animal (n = 10); T04 = control animals that received intravenously, only saline solution with the same syringe and needle (n = 5).
The randomization and distribution of the bovines was based on the weight of each animal on D −1. For animals of T01 to T03, they were divided into ten blocks of three animals each. The animals were listed in descending order of the weight. The first three animals (with the highest weight) were assigned to the first block, the following three animals were assigned to the second block, and so on until all ten blocks were filled. Next, the three animals in each block were randomly assigned to each of the treatment groups (T01, T02 or T03). Five animals with similar body weight were kept as a control (T04 = 5). These procedures were repeated in each repetition (R1 and R2).
Experimental design for iatrogenic routes and Trypanosoma vivax diagnoses in animals
After randomization, the animals were separated into their respective groups and later directed to the containment trunk. With the donor bovine showing approximately 1.0 × 106 trypomastigotes per mL, a puncture of 2 mL of blood from the jugular vein of this animal was performed, using a 5 mL syringe and a 25 × 0.8 mm needle. Then, this volume of blood was discarded in a vial and, using the same syringe and needle, 4 mL of saline solution containing 0.9% sodium chloride were immediately aspirated and applied to the first bovine, of the respective group, which entered the containment trunk. Next, another 4 mL of saline solution was aspirated, which was injected into the second animal that entered the containment trunk; so successively until the 10th animal in each group (T01 = subcutaneous; T02 = intramuscular/T03 = intravenous), when entering the containment trunk, received saline solution always using the same syringe, needle and saline bottle (Fig. 1). This procedure was performed separately for each group (T01, T02 and T03). In addition, a syringe, a needle and a saline vial were used for each of these three groups separately.

Fig. 1. Experimental design for iatrogenic routes and Trypanosoma vivax diagnoses in animals of T01, T02 and T03. 1 = 2 mL of blood was collected intravenously from the reservoir animal infected with ±1 × 106 T. vivax trypomastigotes. 2 = Elimination of 2 mL of blood collected from the reservoir animal. 3 = Withdrawal of 4 mL of saline solution from a 50 mL bottle. 4 = Saline application (subcutaneous T01; or intramuscular T02; or intravenous T03) in the first bovine that entered in the containment trunk. 5 = Withdrawal of 4 mL of saline solution from a 50 mL bottle. 6 = Saline application (subcutaneous T01; or intramuscular T02; or intravenous T03) in the second bovine that entered in the containment trunk. 7 = Withdrawal of 4 mL of saline solution from a 50 mL bottle. 8 = Saline application (subcutaneous T01; or intramuscular T02; or intravenous T03) in the third bovine that entered in the containment trunk. 9 = Withdrawal of 4 mL of saline solution from a 50 mL bottle. 10 = Saline application (subcutaneous T01; or intramuscular T02; or intravenous T03) in the fourth bovine that entered in the containment trunk. 11 = Withdrawal of 4 mL of saline solution from a 50 mL bottle. 12 = Saline application (subcutaneous T01; or intramuscular T02; or intravenous T03) in the fourth bovine that entered in the containment trunk, and so on until the 10th animal of each group.
Day zero (D0) of the study was considered as the day on which the animals were inoculated with 4 mL of saline solution plus the remaining blood in the syringe and needle after disposal. The time between the removal of blood from the donor animal, until the 10th animal in each group received the saline solution, was measured. The order of application in each animal, within each group, happened randomly, according to the order of entry of the animal of each group in the containment trunk. On days 3, 7, 14, 21 and 28, the presence of T. vivax was examined using Brener (Reference Brener1961) and conventional PCR (Cortez et al., Reference Cortez, Rodrigues, Garcia, Neves, Batista, Bengaly, Paiva and Teixeira2009).
Experiment 2 (laboratory assay): viability of Trypanosoma vivax in products for veterinary use in cattle
Experimental design to evaluate the viability of Trypanosoma vivax in the products
The in vitro viability test of T. vivax in veterinary medicines was carried out at the Veterinary Parasitology Center (CPV) of the Federal University of Goiás (UFG), Goiânia, Goiás, Brazil. A total of 109 injectable drugs of different drug classes were evaluated, belonging to: antibiotics, analgesics, anti-inflammatory drugs, antipyretics, antiparasitic, vitamin complexes, reproductive hormones, vaccines, among others manufactured by several laboratories. Total blood and blood with 0.9% saline solution were the negative controls. The pH of all 109 products was checked using a Gehaka PG1800 model device. Before the measurement, the device was calibrated with a buffer solution pH 4.00 and pH 10.0 (Table 1). The evaluation of each solution containing 1.0 × 106 trypomastigotes + product (each of the 109 solutions + controls) at different exposure times was performed in quintuplicate.
Table 1. Injectable veterinary products (n = 109) evaluated, drug classification, pH values and presence of viable Trypanosoma vivax

NA, not applied: it was not possible to perform the reading with the equipment used.
After reactivation and replication of the number of T. vivax trypomastigotes in the two reservoir animals, as described above, approximately 30 mL of blood was collected from the jugular vein in a tube containing EDTA. Immediately after collection, the sample was transported to the laboratory for use in the in vitro viability test using the 109 solutions. Each millilitre of blood contained approximately 3.3 × 106 viable trypomastigotes quantified using the Brener (Reference Brener1961) method.
Three hundred μL of blood containing approximately 1 × 106 viable T. vivax trypomastigotes were placed in plastic Eppendorf microtubes. A product was added to each tube at the respective concentration until completing 1 mL. For oxytocin products, more times were evaluated, and oxytocin testes was homogenized and a 5 μL aliquot was prepared for the study of viable (motile) parasites after exposure times of 30 s, 1, 2, 3, 5, 10, 30 1 h20, 2, 2 h40, 3 h20, 4 and 5 h, following the method recommended by Wang et al. (Reference Wang, Jobe, Tyler and Steverding2008) and Couto et al. (Reference Couto, Bastos, Heller, Zapa, de Assis Cavalcante, Nicaretta, Cruvinel, de Melo Júnior, Ferreira, Soares, Cadioli, de Mendonça and Lopes2021a).
The other products were evaluated separately from the oxytocins, in a ‘second battery’ of tests. In this case, each tested solution was homogenized and at 5 μL aliquot was prepared for the study of viable (motile) parasites after exposure times of 30 s, 1, 5, 10, and 40 min, 1 h20, 2, 2 h40, 3 h20, 4, 5, 6, 7, 8, 10, 12, 14, 16, 18, 20, 22 and 24 h, following the method recommended by Wang et al. (Reference Wang, Jobe, Tyler and Steverding2008) and Couto et al. (Reference Couto, Bastos, Heller, Zapa, de Assis Cavalcante, Nicaretta, Cruvinel, de Melo Júnior, Ferreira, Soares, Cadioli, de Mendonça and Lopes2021a). The evaluation of the viability of T. vivax at different times was completed when the last product failed to demonstrate viable trypomastigotes for at least two consecutive observation periods.
Statistical analysis
Experiment 1 (field assay)
The results regarding cattle infected (T01: subcutaneous route; T02: intramuscular; and T03: intravenous) or not (T04 = control animals) by T. vivax from different treatments were analysed by SAS (2006), using Fisher's exact non-parametric test, with a significance level of 5%.
Experiment 2 (laboratory assay)
The data from the crude trypomastigote counts in the different products at each evaluation time were transformed into log n (x + 1). The transformed data were analysed using a mixed repeated-measures linear model, which included fixed effects for treatment, exposure time and treatment–exposure time interaction. Differences among the treatments were determined using the Kruskal–Wallis test with the level of significance set at 5% (SAS, 2006).
Results
Experiment 1 (field assay)
In R1 of this experiment, after using the same syringe/needle/bottle of saline solution by subcutaneous, intramuscular and intravenous routes, one, four and seven cattle were infected with T. vivax, respectively. In R2, three, five and eight cattle were infected with T. vivax via the subcutaneous, intramuscular and intravenous routes, respectively, using the same syringe/needle/saline bottle. No cattle kept as a negative control became infected with T. vivax during the study. Considering the two repetitions together (R1 and R2), the total number of cattle infected with T. vivax via the subcutaneous route (3/20) was lower (P ≤ 0.05) compared to the total number of cattle infected via the intramuscular route (9/20), which was lower (P ≤ 0.05) compared to the intravenous route (15/20) (Table 2).
Table 2. Summary of the result of animals infected or not, after day 0 of the study, according to the order in which these animals' entrance in the containment and saline solution administered by different routes (subcutaneous, intramuscular and intravenous)

Positive = animals positive for T. vivax by Woo and cPCR during the period post saline solution application using the same syringe and needle. NA = not applied total animals infected with T. vivax, followed by the same letter on the line does not differ (P > 0.05).
Considering the evaluation days when the investigation of T. vivax in animals by PCR was performed, the incubation period was different for the injections routes and for the order in which the animals received saline solution + viable forms of T. vivax. In R1, by the subcutaneous route, the incubation period was 14 days for the 1st animal. In R2 for this same route, the incubation period for the 1st animal was 7 days, and for the 2nd and 3rd animals it was 14 days. Via intramuscular, in R1 the incubation periods for the 1st animal were 7 days, while the 2nd, 4th and 5th were 14 days. In R2 of the intramuscular route, the incubation periods for the 1st, 2nd and 3rd, 4th and 5th animals were 3, 7 and 14 days, respectively. Through the intravenous route, in R1 the incubation periods for the 1st and 2nd animal were 3 days, for the 3rd, 5th and 6th it was 7 days and for the 7th and 8th it was 14 days. In R2 by intravenous route, the following incubation periods were observed: 1st, 2nd and 3rd, 4th to the 8th animals were 3, 7 and 14 days, respectively.
The average time from the blood withdrawal from the donor animal until the 10th animal of each group received it in both repetitions was 4.42, 4.31 and 5.46 min, for the animals of the groups that received the saline solution by the subcutaneous, intramuscular and intravenous routes, respectively.
Experiment 2 (laboratory assay)
Table 1 shows that the pH value of the 109 products ranged from 2.33 (Corta Curso®) to 9.83 (Fortigal Plus®). Among the 48 products in which viable trypomastigote forms of T. vivax were visualized, the pH of the products ranged from 3.92 (Catosal®) to 9.83 (Fortigal Plus®). Still within these 48 products, in 16 the device used was unable to measure the pH value. For the 63 products in which no viable T. vivax was found, the pH values ranged from 2.33 (Corta Curso®) to 9.55 (Maxican® 2%).
Of the 109 products evaluated, in 44% (48/109) trypomastigote forms of T. vivax remained viable regardless of time. Among the different drug classes evaluated, this protozoan was found viable in 100% (7/7) of oxytocin-based hormones, in 60% (6/10) of non-oxytocin-based reproductive hormones, in 64.3% (9/14) of the vaccines, in 63.3% (8/15) of the vitamin/derivative complexes, 30% (6/20) of the antibiotics and in 29.6% (8/27) of the antiparasitic products tested (Table 3). In the group of oxytocin-based products (Ocitocin Forte®, Lactocin®, Placentex®, Ocitocin Biofarma®, Ocitovet® and Placentina®), in six, T. vivax survived for up to 2 min. In only one (Ocitopec®), viable trypomastigote forms of this protozoan were found for up to 2 h (Table 4).
Table 3. Injectable drug classification, total analysed, total and percentage of positives products for the presence of viable T. vivax regardless the time evaluation positives

Table 4. Mean counts of viable T. vivax trypomastigotes in six oxytocin products and controls (blood + saline solution and total blood)

1 = Means followed by the same letter in the column, do not differ (P > 0.05).
In vaccines, foot-and-mouth disease (Aftovacin® and Ourovac®) and brucellosis (Brucelina B-19® and Brucelin B-51®) stand out. Vaccines against foot-and-mouth disease were those that kept T. vivax viable for a longer period, up to 20 h. Furthermore, it was possible to observe the presence of inverted blood micelles containing T. vivax trypomastigotes in the samples of these vaccines. In vaccines against brucellosis, this protozoan remained viable from 7 to 12 h. Among the other vaccines, T. vivax survived for up to 30 s on ScourGuard® 4KC, 10 min on IBR/BVD Hertape® Vaccine, 40 min on Rotavec Corona®, 3 h20 min in Raivacel Multi® and 4 h in CattleMaster® Gold FP 5/L5. In the antiparasitic group, in two doramectin-based products (Dectomax® and Dorax®), T. vivax was viable for up to 7 h. In the other products in this group, viable forms of trypomastigotes were found for up to 30 s (Ivomec® Gold, Long Range®, Longamectin® Premium and Treo® ACE), 1 min (Master LP®) and 5 min (Vivedium®). At some evaluation times, the mean of T. vivax trypomastigotes quantified in the vaccines Aftovacin®, Ourovac®, Brucelin B-51®, Brucelin-B19®, and in the doramectin-based products (Dectomax® and Dorax®), was higher (P ≤ 0.05) than the mean of trypomastigotes of this protozoan found in the blood + saline solution (Table 5).
Table 5. Mean counts of viable T. vivax trypomastigotes in 48 injectable veterinary products and controls (blood + saline solution and total blood)

1 = Means followed by the same letter in the column, do not differ (P > 0.05).
As for reproductive hormones, in some of them, viable T. vivax was visualized for up to 1 min (Fertagyl®, FertiCare Ovulation®, Folligon® Gonadiol®) and up to 3 h20 min (E.C.P® – Zoetis). In vitamin complexes and derivatives, T. vivax trypomastigotes remained viable in some products for up to 30 s (Roborante®), 5 min (Fosfosal®), 10 min (Phenodral®, Roboforte®), 40 min (Hertavita®) and 1 h20 min (ADE injectable emulsifiable®, Monovin A®). In the antibiotic group, this protozoan remained viable in some products for up to 30 s (Ceftiomax®, Cobactan® and Fortgal Plus®), 10 min (Borgal®) and 40 min (Clamoxyl®). In other products, viable forms of T. vivax were identified in some products for up to 30 s (Aliv V®, Cursotrat®), 1 min (Sedacol®) and 40 min (Camphora oil UCB®) (Table 5). In blood diluted with saline solution and in whole blood, viable trypomastigotes of T. vivax were found for up to 6 and 18 h, respectively (Table 4).
Discussion
This study describes unprecedented results directly applied in the field. It was possible to demonstrate how many cattle can become infected with T. vivax by subcutaneous, intramuscular, and intravenous routes, from an animal with an acute infection of this protozoan, reusing the same syringe and needle, simulating the administration of drugs in the field. In addition, the viability time of T. vivax in 109 injectable products for veterinary use was evaluated.
Studies with experimental infection of T. vivax in cattle have already demonstrated the infection of this protozoan when animals are infected subcutaneously, intravenously (Fidelis Junior et al., Reference Fidelis Junior, Sampaio, Machado, André, Marques and Cadioli2016; Bassi et al., Reference Bassi, de Araújo, Garcia, Vinícius da Silva, Oliveira, Bittar, de Souza Gomes, Rodrigues do Amaral, Costa e Silva, Nascentes, Rodrigues Junior, Martins-Filho, Araújo and Bittar2018; Bastos et al., Reference Bastos, Faria, Couto, Nicaretta, Cavalcante, Zapa, Ferreira, Heller, Madrid, Cruvinel, Rossi, Soares, Cadioli and Lopes2020b), intradermally and intramuscularly (Bastos et al., Reference Bastos, Faria, Couto, Nicaretta, Cavalcante, Zapa, Ferreira, Heller, Madrid, Cruvinel, Rossi, Soares, Cadioli and Lopes2020b). The reuse of hypodermic needles, although not recommended, is a quite common practice in several countries (USDA, 2011). In a survey that assessed biosafety in farm animals in the United States, Canada, Germany, Sweden and Ecuador, it is revealed that in some cases, veterinarians reuse the same needle in up to 30 cattle (Anderson, Reference Anderson2010). The present work showed that not only the reuse of the same needle is a factor to spread a disease, the route of administration in which these fomites are used is also important to determine how many cattle can become infected. In the case of T. vivax, when the same syringe and needle is reused from an animal with the acute disease, up to 8, 5 and 3 cattle can become infected intravenously, intramuscularly and subcutaneously, respectively.
Regarding the intravenous route and T. vivax, in the field the use of intravenous oxytocin in lactating cows performed with the same needle and syringe on several animals contributes to spreading the protozoan in the herd (Costa et al., Reference Costa, Abreu, Thomé, Massard, Santos, Ubiali and Brito2020). In the present study, in 100% of the oxytocins evaluated, T. vivax remained viable for up to 2 min, except for one brand in which trypomastigote forms of this protozoan were found for up to 2 h. In practice, the time of 2 min is enough for a rapid spread of T. vivax in Girolando dairy herds that carry out this management practice during milking, since during this time 5–10 cows receive this hormone intravenously. It is evident that the administration of oxytocin is responsible for the spread of this protozoan among dairy Girolando cattle (Bastos et al., Reference Bastos, Faria, Couto, Nicaretta, Cavalcante, Zapa, Ferreira, Heller, Madrid, Cruvinel, Rossi, Soares, Cadioli and Lopes2020b). However, despite the evidence mentioned above for the intravenous route and oxytocin, it is worth highlighting that not only the use of oxytocin may also help to disseminate this protozoan in the routine of farms, regardless of whether the animals are suitable for milk or beef, but the use of other injectable veterinary products such as vaccines, antibiotics and hormones for reproductive protocols.
In the current study, T. vivax remained viable for a certain period in 64.3 and 29.6% of injectable vaccines and antiparasitic products, respectively. In products based on doramectin (Dectomax® and Dorax®), T. vivax survived for 7 h, while in vaccines against brucellosis (Brucellin B-51® and Brucelin B-19®) and against foot-and-mouth disease (Aftovacin® and Ourovac®), this same protozoan remained viable for up to 8–12 and 20 h, respectively. The majority of antiparasitic products are administered subcutaneously, and vaccines can be used subcutaneously, or in some cases, intramuscularly. This fact could reduce the chance of new cattle being infected by T. vivax, from an animal infected by the subcutaneous route, when compared to the other iatrogenic routes, as observed in this study. However, in vaccines and injectable antiparasitic drugs, T. vivax remained viable for longer, which in practice certainly increases the chances of other cattle becoming infected when this type of product is used, via the subcutaneous route. In addition, these veterinary products, as well as the use of oxytocin, are generally used as a massive treatment for the herd (Bastos et al., Reference Bastos, Faria, Couto, Nicaretta, Cavalcante, Zapa, Ferreira, Heller, Madrid, Cruvinel, Rossi, Soares, Cadioli and Lopes2020b; Couto et al., Reference Couto, Bastos, Heller, Zapa, de Assis Cavalcante, Nicaretta, Cruvinel, de Melo Júnior, Ferreira, Soares, Cadioli, de Mendonça and Lopes2021a), unlike the use of antibiotics, or some vitamin supplements that can be applied in a more selective and specific way to animals.
The reproductive management of dairy and beef cows on the properties is management approach that possibly facilitates the spread of the protozoan in question in the herd. In this case, the cows are simultaneously submitted to reproductive protocols, with the administration of drugs, mostly, through the intramuscular route (Claypool et al., Reference Claypool, Spencer, Zoca, Shafii, Price, Ahmadzadeh, Rimbey and Dalton2019; Couto et al., Reference Couto, Zapa, Heller, de Cavalcante, Nicaretta, Cruvinel, Colli, Ferreira, Alencar, de Melo-Junior, Soares, de Borges and Lopes2021b). In this sense, if there is a carrier animal during the acute phase of T. vivax, the pathogenic agent can spread quickly in the herd, since, in the present study, this protozoan remained viable in 60% of the tested reproductive hormones, and even five cattle were infected via the intramuscular route. In one of these products, T. vivax survived for up to 3 h20 min. In addition, some vaccines such as brucellosis are mandatory for females in some countries, which may further increase the chances of damage caused by T. vivax to producers. Even that, there is still the possibility of future reproductive damage in these females, triggered by this protozoan, if any animal becomes infected (Ogwu et al., Reference Ogwu, Njoku and Osori1986; Okech et al., Reference Okech, Watson, Luckins and Makawiti1996).
In the present study, the pH of the formulations and the actives seem to not influence the viability of T. vivax in the different products. From the results found, possibly the constituents of the vehicles present in the formulations have a direct relationship with the survival of this protozoan in the products. The viability of T. vivax was longer especially in products with oily vehicles, such as foot-and-mouth disease and brucellosis vaccines, and in doramectin-based antiparasitic drugs. Notoriously, the blood plasma, where T. vivax is found, is a predominantly aqueous fraction (Psychogios et al., Reference Psychogios, Hau, Peng, Guo, Mandal, Bouatra, Sinelnikov, Krishnamurthy, Eisner, Gautam, Young, Xia, Knox, Dong, Huang, Hollander, Pedersen, Smith, Bamforth, Greiner, McManus, Newman, Goodfriend and Wishart2011), and when it came into contact with oily products, there was the formation of inverted micelles (Nielloud and Marti-Mestres, Reference Nielloud and Marti-Mestres2000 – when a liquid, in this case blood, is completely surrounded by the constituents of the product) containing the trypomastigotes forms, which separated from the product, showing no emulsion between the blood containing T. vivax with the products. Of the 48 products in which this protozoan remained viable at some point, in 16 products it was not possible to read the pH, due to the presence of oily vehicles in these formulations.
The current work does not aim to fix the number of animals that are infected by different routes from a syringe and needle contaminated by T. vivax and reused. In practice, there will be factors that will determine whether this occurs or not, such as the number of T. vivax trypomastigotes presented by an infected animal, combined with the customs of each property regarding medicines administration management. Although the injection mostly involves pushing rather than pulling, a very common practice in the properties is when the subcutaneous or intramuscular routes are used, the employee, before administering the drug, pulls the syringe plunger to check if the bloodstream has not been reached, since many products should not be administered intravenously. In the same way, when an employee uses the intravenous route, he/she also pulls the syringe plunger back to confirm that the medication will be administered in the bloodstream. During this act, pulling the syringe plunger back to check the administration route of the product becomes a risk for T. vivax transmission between animals.
In addition to the iatrogenic transmission evaluated in this study, there is also the possibility of mechanical transmission of T. vivax by hematophagous insects. This fact should be better investigated once isolating an agent in a fly indicates that this insect demonstrates vector capacity for that pathogenic agent; however, this fly does not necessarily have the vector competence to transmit this agent to a host (Scoles and Ueti, Reference Scoles and Ueti2015; De la Fuent et al., Reference de la Fuente, Antunes, Bonnet, Cabezas-Cruz, Domingos, Estrada-Peña, Johnson, Kocan, Mansfield, Nijhof, Papa, Rudenko, Villar, Alberdi, Torina, Ayllón, Vancova, Golovchenko, Grubhoffer, Caracappa, Fooks, Gortazar and Rego2017). It is noteworthy that the movement of animals is free between properties, and T. vivax is not a priority disease for mandatory diagnostic tests to be carried out to trade and transport cattle (OIE, 2021); this measure is associated with bad biosafety behaviours on farms, using the same syringe, needle and medicine bottles, constitutes an important way of transmission of this protozoan between properties, and between animals in the same herd. Educational measures must be carried out with cattle owners, as using one needle and syringe per animal, or to perform the sanitization of the material with 0% alcohol and 0.5% iodine solutions between the samples (Couto et al., Reference Couto, Bastos, Heller, Zapa, de Assis Cavalcante, Nicaretta, Cruvinel, de Melo Júnior, Ferreira, Soares, Cadioli, de Mendonça and Lopes2021a), with the objective of interrupting the cycle of dissemination of T. vivax in herds.
Conclusion
By reusing the same syringe and needle, from an animal with an acute infection for T. vivax, up to 30% (3/10), 50% (5/10) and 80% (8/10) bovines become infected by this protozoan by subcutaneous, intramuscular and intravenous routes, respectively. Of the 109 products evaluated, viable trypomastigote forms of T. vivax were diagnosed in 48. The largest proportion of products that this protozoan remained viable were hormones based on oxytocin, reproductive hormones, vaccines, vitamin complexes, antibiotics and antiparasitic drugs. In some antiparasiticides and vaccines, T. vivax survived for up to 7 and 20 h, respectively. Apparently, formulations with oily vehicles increased the survival time of this protozoan in the products.
Author contribution
RDMJ: investigation; data curation. TSAB: conceptualization; methodology. LMH: investigation. LFMC: investigation. DMBZ: investigation. ASAC: investigation. LBC: investigation. JEN: investigation. LLF: writing – review & editing. VES: formal analysis. GRLS: methodology; investigation. FAC: conceptualization; methodology. WDZL: supervision; data curation; writing – original draft.
Financial support
This work was supported by Fundação de Amparo à Pesquisa do Estado de Goiás – financial code 201810267001189; Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) – Brazil – Finance Code 001; Conselho Nacional de Desenvolvimento Científico e Tecnológico, Brazil CNPq – #5882670080665232.
Conflict of interest
None.
Ethical standards
This study received approval from the Animal Use Ethics Committee of the Federal University of Goiás, Brazil (certificate number: 009/20) and was conducted in compliance with the ethical principles governing animal experimentation of the Brazilian National Animal Experimentation Control Council (CONCEA).