Introduction
Chagas disease is caused by the protozoan Trypanosoma cruzi (Chagas, Reference Chagas1909) and affects about 7 million people worldwide, especially in the 21 endemic countries of Latin America (WHO, 2020). The infection is classified as a neglected tropical disease and related to poor populations in tropical and subtropical regions, although it has been spread to non-endemic areas in Europe, the USA and Japan (Lidani et al., Reference Lidani, Andrade, Bavia, Damasceno, Beltrame, Messias-Reason and Sandri2019). Benznidazole (BZ) and nifurtimox (NFX) are the nitro drugs of choice for the treatment of T. cruzi infection. These drugs are effective in inducing cure in the early stages of infection, but the benefit of their administration in the chronic phase is limited due to variable efficacy (Ribeiro et al., Reference Ribeiro, Dias, Paiva, Hagström-Bex, Nitz, Pratesi and Hecht2020). In addition, treatment is long and may lead to several adverse reactions that compromise its continuation (Pérez-Molina and Molina, Reference Pérez-Molina and Molina2018).
Looking for new alternatives of Chagas disease treatment, a large number of molecules have been evaluated in preclinical studies and few promising compounds have been tested in clinical trials (Villalta and Rachakonda, Reference Villalta and Rachakonda2019), including the azolic inhibitors of sterol C14α demethylase posaconazole and fosravuconazole (Molina et al., Reference Molina, Gómez i Prat, Salvador, Treviño, Sulleiro, Serre, Pou, Roure, Cabezos, Valerio, Blanco-Grau, Sánchez-Montalvá, Vidal and Pahissa2014; Torrico et al., Reference Torrico, Gascon, Ortiz, Alonso-Vega, Pinazo, Schijman, Almeida, Alves, Strub-Wourgaft, Ribeiro, Santina, Blum, Correia, Garcia-Bournisen, Vaillant, Morales, Pinto Rocha, Rojas Delgadillo, Magne Anzoleaga, Mendoza, Quechover, Caballero, Lozano Beltran, Zalabar, Rojas Panozo, Palacios Lopez, Torrico Terceros, Fernandez Galvez, Cardozo, Cuellar, Vasco Arenas, Gonzales, Hoyos Delfin, Garcia, Parrado, de la Barra, Montano, Villarroel, Duffy, Bisio, Ramirez, Duncanson, Everson, Daniels, Asada, Cox, Wesche, Diderichsen, Marques, Izquierdo, Sender, Reverter, Morales and Jimenez2018). Although these clinical studies represented an advance in the field of chemotherapy for Chagas disease, they led to disappointing results, with high levels of therapeutic failure detected (Molina et al., Reference Molina, Gómez i Prat, Salvador, Treviño, Sulleiro, Serre, Pou, Roure, Cabezos, Valerio, Blanco-Grau, Sánchez-Montalvá, Vidal and Pahissa2014; Morillo et al., Reference Morillo, Marin-Neto, Avezum, Sosa-Estani, Rassi, Rosas, Villena, Quiroz, Bonilla, Britto, Guhl, Velazquez, Bonilla, Meeks, Rao-Melacini, Pogue, Mattos, Lazdins, Rassi, Connolly and Yusuf2015; Torrico et al., Reference Torrico, Gascon, Ortiz, Alonso-Vega, Pinazo, Schijman, Almeida, Alves, Strub-Wourgaft, Ribeiro, Santina, Blum, Correia, Garcia-Bournisen, Vaillant, Morales, Pinto Rocha, Rojas Delgadillo, Magne Anzoleaga, Mendoza, Quechover, Caballero, Lozano Beltran, Zalabar, Rojas Panozo, Palacios Lopez, Torrico Terceros, Fernandez Galvez, Cardozo, Cuellar, Vasco Arenas, Gonzales, Hoyos Delfin, Garcia, Parrado, de la Barra, Montano, Villarroel, Duffy, Bisio, Ramirez, Duncanson, Everson, Daniels, Asada, Cox, Wesche, Diderichsen, Marques, Izquierdo, Sender, Reverter, Morales and Jimenez2018). While limitations concerning the appropriate dose and duration of treatments with azoles required to control human T. cruzi infections are being discussed (Martínez-Peinado et al., Reference Martínez-Peinado, Cortes-Serra, Losada-Galvan, Alonso-Vega, Urbina, Rodríguez, VandeBerg, Pinazo, Gascon and Alonso-Padilla2020), the clinical development pipeline for Chagas disease is actually based on nitro compounds, either in proof of concept trials, such as fexinidazole (FEX12-NCT03587766), or evaluating new regimens of compounds already in use (MultiBenz – NCT03191162; BENDITA – NCT03378661; CHICAMOCHA 3 – NCT02369978; NCT03981523) (Martínez-Peinado et al., Reference Martínez-Peinado, Cortes-Serra, Losada-Galvan, Alonso-Vega, Urbina, Rodríguez, VandeBerg, Pinazo, Gascon and Alonso-Padilla2020).
Nitro compounds, such as the nitrofuran NFX and the nitroimidazoles BZ and fexinidazole, are a group of bioactive compounds with well-established indications to treat a wide variety of conditions, including those caused by parasites (Patterson and Wyllie, Reference Patterson and Wyllie2014). The basis for their biological activity is the biotransformation of the nitro group, releasing intermediates in the redox process, which bind to macromolecules causing damage (Patterson and Fairlamb, Reference Patterson and Fairlamb2019).
Particularly, fexinidazole is very active against trypanosomatides (Winkelmann and Raether, Reference Winkelmann and Raether1978; Jennings and Urquhart, Reference Jennings and Urquhart1983; Raether and Seidenath, Reference Raether and Seidenath1983; Kaiser et al., Reference Kaiser, Bray, Cal, Bourdin Trunz, Torreele and Brun2011; Bahia et al., Reference Bahia, de Andrade, Martins, da Silva do Nascimento, de Diniz, Caldas, Talvani, Trunz, Torreele and Ribeiro2012; Wyllie et al., Reference Wyllie, Patterson, Stojanovski, Simeons, Norval, Kime, Read and Fairlamb2012; Tarral et al., Reference Tarral, Blesson, Mordt, Torreele, Sassella, Bray, Hovsepian, Evène, Gualano, Felices and Strub-Wourgaft2014), and the drug was recently approved as the first oral treatment for African trypanosomiasis (Deeks, Reference Deeks2019). After promising preclinical data on T. cruzi infection, fexinidazole has been evaluated in clinical trials against chronic Chagas disease (DNDi, 2020). The first clinical trial was interrupted due to safety and tolerability issues (NCT02498782). The second clinical trial, using lower fexinidazole doses, has now been completed (FEX12 – NCT03587766), but the results are not available (DNDi, 2020). Fexinidazole is orally available and is rapidly converted by oxidative metabolism to two metabolites, the sulfoxide and the sulfone (Torreele et al., Reference Torreele, Bourdin Trunz, Tweats, Kaiser, Brun, Mazué, Bray and Pécoul2010). Bahia et al. demonstrated that the oral administration of fexinidazole metabolites was well tolerated and effective in treating acute murine T. cruzi infection (Bahia et al., Reference Bahia, Nascimento, Mazzeti, Marques, Gonçalves, Mota, de Diniz, Caldas, Talvani, Shackleford, Koltun, Saunders, White, Scandale, Charman and Chatelain2014). The authors identified that the primary effective species is probably the sulfone metabolite of fexinidazole (fex-SFN) and that high concentrations need to be maintained to ensure efficacy (Bahia et al., Reference Bahia, Nascimento, Mazzeti, Marques, Gonçalves, Mota, de Diniz, Caldas, Talvani, Shackleford, Koltun, Saunders, White, Scandale, Charman and Chatelain2014). However, the effects of lower doses of this metabolite when combined with other drugs have not been evaluated yet.
Drug combinations have been evaluated for experimental (Araujo et al., Reference Araujo, Martins-Filho, Pereira and Brener2000; Benaim et al., Reference Benaim, Sanders, Garcia-Marchán, Colina, Lira, Caldera, Payares, Sanoja, Burgos, Leon-Rossell, Concepcion, Schijman, Levin, Oldfield and Urbina2006; Cencig et al., Reference Cencig, Coltel, Truyens and Carlier2012; de Diniz et al., Reference Diniz, Urbina, Andrade, Mazzeti, Martins, Caldas, Talvani, Ribeiro and Bahia2013, Reference Diniz, Mazzeti, Caldas, Ribeiro and Bahia2018; Grosso et al., Reference Grosso, Alarcon, Bua, Laucella, Riarte and Fichera2013; Strauss et al., Reference Strauss, Lo Presti, Bazán, Baez, Fauro, Esteves, Sanchez Negrete, Cremonezzi, Paglini-Oliva and Rivarola2013; Assíria Fontes Martins et al., Reference Assíria Fontes Martins, de Figueiredo Diniz, Mazzeti, da Silva do Nascimento, Caldas, Caldas, de Andrade, Ribeiro and Bahia2015; Providello et al., Reference Providello, Carneiro, Portapilla, do Vale, Camargo, Tirapelli and de Albuquerque2018; Guedes-da-Silva et al., Reference Guedes-da-Silva, da Batista, Da Silva, Pavão, Batista, Moreira, Souza, Britto, Rachakonda, Villalta, Lepesheva and de Soeiro2019; Mazzeti et al., Reference Mazzeti, de Diniz, Gonçalves, WonDollinger, Assíria, Ribeiro and Bahia2019; Rocha Simões-Silva et al., Reference Rocha Simões-Silva, Brandão Peres, Britto, Machado Cascabulho, de Melo Oliveira, Nefertiti da Gama, França da Silva, Lima da Costa, Finamore Araújo, Diego de Souza Campos, Meuser Batista, Cristina Demarque, da Cruz Moreira and de Nazaré Correia Soeiro2019; Machado et al., Reference Machado, Bahia, Caldas, Mazzeti, Novaes, Vilas Boas, de Santos, Martins-Filho, Marques and de Diniz2020; Ribeiro et al., Reference Ribeiro, Dias, Paiva, Hagström-Bex, Nitz, Pratesi and Hecht2020) and in the clinical context for Chagas disease (BENDITA – NCT03378661, STOP CHAGAS – NCT01377480). Interestingly, the association between nitro compounds has not been extensively evaluated. Thus, the objective of this work is to assess the effects of treatment with BZ, NFX, fex-SFN, and their combinations in vitro and in vivo on experimental T. cruzi infection.
Materials and methods
Parasite
In the study, the T. cruzi Y strain classified as DTU II (Zingales et al., Reference Zingales, Andrade, Briones, Campbell, Chiari, Fernandes, Guhl, Lages-Silva, Macedo, Machado, Miles, Romanha, Sturm, Tibayrenc and Schijman2009) and previously characterized as partially resistant to BZ (Filardi and Brener, Reference Filardi and Brener1987) was used.
Study drugs
BZ, which is also known as N-benzyl-2-(2-nitroimidazol-1-yl) acetamide, was purchased from Laboratório Farmacêutico de Pernambuco (LAFEPE, Recife, Brazil). Fex-SFN, which is also known as 1-methyl-2-(4-methylsulfonyl phenoxymethyl)-5-nitroimidazole (Axyntis/Centipharm, France), was provided by the Drugs for Neglected Diseases initiative (DNDi). NFX, which is also known as (E)-N-(3-methyl-1,1-dioxo-1,4-thiazinan-4-yl)-1-(5-nitrofuran-2-yl) methanimine, was donated by the DNDi.
For in vitro assays, stock solutions of BZ, fex-SFN and NFX were prepared in dimethyl sulfoxide (DMSO) and stored at −20°C. Stock solutions were further diluted to appropriate working concentrations using a culture medium. Importantly, the final DMSO concentration never exceeded 0.5% (v/v) in order to avoid toxicity to host cells. For in vivo assays, BZ and NFX were suspended in 0.5% methylcellulose solution in distilled water and fex-SFN was formulated in an aqueous suspension containing 0.5% methylcellulose and 5.0% polysorbate.
In vitro assays
Toxicity of combinations of nitro compounds to host cells
In vitro assays were performed using the H9c2 (American Type Culture Collection, ATCC: CRL 1446) cardiomyoblast lineage. Cells were maintained in 25 cm2 bottles in Dulbecco's modified Eagle's medium (DMEM) supplemented with 10% fetal bovine serum, 1% l-glutamine 2 μ m, 100 IU mL−1 penicillin and 0.1 mg mL−1 streptomycin at 37°C in an atmosphere of 5% CO2. To exclude toxic effects of drug combinations on mammalian cells, cytotoxicity was measured by the Resazurin colorimetric assay for cell viability and proliferation inhibition according to the previously described method (Diniz et al., Reference Diniz, Mazzeti, Caldas, Ribeiro and Bahia2018). Briefly, 1 × 103 H9c2 cells were plated per well in 96-well plates and incubated at 37°C, 5% CO2 for 24 h. Thus, cells were incubated for 72 h with increasing concentrations of each drug in twofold dilutions, covering a range of 1.56–200 μ m for BZ, 0.78–100 μ m for NFX and 1.56–200 μ m for fex-SFN. The top concentration of combined treatment was 100 μ m plus 100 μ m for BZ/fex-SFN and 50 μ m plus 100 μ m for NFX/fex-SFN, followed by eight 1:2 dilutions. The plates were subjected to microplate spectrophotometer reading (Biochrom Anthos 2010 Microplate Reader, Cambridge, United Kingdom) at 570 and 600 nm wavelengths. The percentage of cell viability induced by the treatments was calculated considering the percentage of reduction of incubated cells in the absence of drug. All tests were performed at least twice in triplicate, and the reduction of cell viability by more than 30% was considered cytotoxic, as recommended by the International Organization for Standardization (ISO, 2009).
Determination of nature of interaction among nitro compounds
The evaluation of in vitro anti-amastigote activity was performed using H9c2 cells infected with the Y strain, according to Diniz et al. (Reference Diniz, Mazzeti, Caldas, Ribeiro and Bahia2018). For this, 1 × 104 cells were seeded on coverslips in 24-well plates; after 24 h, cells were infected with T. cruzi Y strain trypomastigotes (20:1 ratio of parasites to host cells). Non-adherent parasites were removed by washing with DMEM after 24 h of interaction, and the cultures were exposed to compounds alone or in combination at concentrations ranging from 0.15 to 20 μ m for BZ, 0.08 to 10 μ m for NFX and 0.15 to 20 μ m for fex-SFN. After 72 h of incubation, the cultures were fixed with methanol, stained with Giemsa, and examined microscopically to determine the percentage of cells infected in treated and untreated controls. IC50 and IC90 values were calculated using Calcusyn software (Biosoft, UK). All tests were performed at least twice in duplicate, and the results were given as mean ± standard deviation.
In vivo assays
Mice, infection and treatment
Female Swiss mice (18–22 g) from the animal facility at UFOP were maintained in a temperature-controlled room with access to water and food ad libitum under 12 h day/night cycles and temperature 22 ± 2°C. Animals were inoculated intraperitoneally with 5 × 103 blood trypomastigotes of T. cruzi Y strain and randomly divided into groups of 6–10 animals. As control groups, infected and untreated and uninfected and untreated animals were used. Each treated group received the compounds daily at different doses alone or in combination by oral gavage for 20 days: BZ 100 mg kg−1 (reference treatment), BZ 50 mg kg−1, fex-SFN 50 mg kg−1, NFX 25 mg kg−1, and combination therapy consisting of BZ 50 mg kg−1 + fex-SFN 50 mg kg−1 or NFX 25 mg kg−1 + fex-SFN 50 mg kg−1. All treatments began on the fourth day after infection at the onset of parasitemia. Mortality was checked daily until 30 days after treatment.
Determination of treatment efficacy
Treatment efficacy was determined following the methodology of Caldas et al. (Reference Caldas, Santos, Lana, de Diniz, Machado-Coelho, Veloso and Bahia2008) based on parasitemia detection by fresh blood examination (Brener, Reference Brener1962) before and after cyclophosphamide (Baxter Oncology, Germany) immunosuppression and blood qPCR. Animals with negative results in the fresh blood examination up to 30 days after treatment were immunosuppressed with cyclophosphamide at the dose of 50 mg kg−1 in three cycles of four consecutive with an interval of 3 days between each cycle. Parasitemia was checked daily during and up to 10 days after immunosuppression cycles.
For qPCR, blood samples were collected 30 and 180 days after treatment from mice with negative fresh blood examinations. Also, heart samples were collected during euthanasia 180 days after treatment to quantify parasite DNA in tissue. The genomic DNA of samples was isolated and purified using the Wizard Genomic DNA Purification Kit (Promega Corp., Madison, WI, USA), according to the manufacturer's instructions. The presence of T. cruzi in samples was evaluated by amplifying a 195-bp sequence, repeated in tandem in genomic DNA, using TCZ-F (5-GCTCTTGCCCACAMGGGTGC-3, where M indicates A or C) and TCZ-R (5-CCAAGCAGCGGATAGTTCAGG-3) primers as described by Cummings and Tarleton (Reference Cummings and Tarleton2003). The murine TNF-α gene sequence was amplified separately using the primers TNF-5241 (5-TCCCTCTCATCAGTTCTATGGCCCA-3) and TNF-5411 (5-CAGCAAGCATCTATGCACTTAGACCCC-3) (Cummings and Tarleton, Reference Cummings and Tarleton2003). Reactions consisted of 2 μL of template DNA at 25 μg mL−1, specific primers at a final concentration of 10 μ m and Sybr-Green PCR Master Mix in a total volume of 10 μL. Standard curves for DNA parasite quantification in the cardiac tissue were produced from 10-fold DNA dilution of epimastigotes of T. cruzi Y strain in DNA from the heart tissue of non-infected mice, ranging from 1 × 106 to 1 parasite equivalent/25 μg of tissue DNA. The DNA amplifications were carried out in the 7500 Fast Real-Time PCR System (Applied Biosystems, Life Technologies, California, USA). After the initial denaturation step of 10 min at 95°C, amplification was carried out for 40 cycles (94°C for 15 s). Fluorescence data collection was performed at 62°C for 1 min at the end of each cycle. Amplification was immediately followed by a melting programme with initial denaturation for 15 s at 95°C, cooling to 60°C for 1 min, and then stepwise temperature increases from 60 to 95°C at 0.3°C s−1. All samples were analysed in duplicate, and negative samples and reagent controls were processed in parallel in each assay. The efficiencies of amplification were determined automatically by 7500 Fast Real-Time PCR software. Animals showing negative results in all tests were considered cured.
Determination of treatment toxicity
Weight determination was performed every 7 days up to 30 days after treatment. In addition, treatment toxicity was evaluated by hepatic enzyme dosages in mouse serum collected on the last day of treatment. For infected and untreated mice, the samples were obtained at day 15 post-infection. In this group, subsequent sampling could not be performed as T. cruzi Y strain infection induced 100% of mortality until day 18 of infection. Aspartate aminotransferase (AST) and alanine aminotransferase (ALT) were determined by colorimetric assay using the commercial Bioclin® kit, according to the manufacturer's instructions, in an autoanalyser (Wiener Lab model CM200 – kinetic analysis).
Statistical analysis
Statistical analysis of the data was performed using GraphPad Prism 5.01 software (GraphPad Software Inc., San Diego, CA, USA). The results were expressed as mean ± standard deviation. Parametric data were analysed with Student's t-test, and non-parametric data were analysed with the Mann–Whitney test. Statistical significance was established with 95% confidence intervals and P < 0.05.
The nature of in vitro drug interactions was determined by the fractional inhibitory concentration (FIC) index. FICs at IC50 and the sum of FICs (ΣFICs) were calculated: FIC of drug A = IC50 of drug A in combination/IC50 of drug A alone. The same equation was applied to the partner drug (drug B), and ΣFICs = FIC drug A + FIC drug B was calculated. The ΣFIC50 was used to classify the interaction as synergistic (ΣFIC⩽0.5), additive or no interaction (0.5⩾ΣFIC <4), or antagonistic (ΣFIC>4) (Odds, Reference Odds2003).
Results
Initially, the cytotoxicities of BZ, NFX and fex-SFN were evaluated in our mammalian host cells model, either alone or in combination. Figure 1 shows the cell viability after 72 h of drug incubation. BZ, fex-SFN and their combinations did not interfere with the viability of H9c2 cells at all concentrations tested (Fig. 1A). Only incubation with 100 μ m NFX and the highest concentrations of the NFX/fex-SFN combination (50 + 100 μ m) induced more than a 30% reduction in cell viability and were considered toxic (Fig. 1B) (ISO, 2009).

Fig. 1. H9c2 cell viability after 72 h of treatment with benznidazole (BZ), nifurtimox (NFX), sulfone metabolite of fexinidazole (fex-SFN) and their combinations. (A) Effects of nitro drugs alone or in combination on the viability of H9c2 cells upon 72 h incubation at the total top concentrations of BZ (200 μ m), NFX (100 μ m), fex-SFN (200 μ m) and their combinations, including BZ/fex-SFN (100 + 100 μ m) and NFX/fex-SFN (50 + 100 μ m), and seven twofold serial dilutions. (B) Bar graphic showing cell viability at the top concentrations of nitro drugs and their combinations in the H9c2 cell line. The results are the average of two independent experiments performed in triplicate.
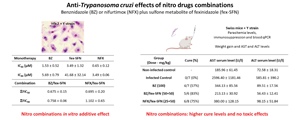
The concentrations considered non-toxic were used to investigate the nature of the in vitro interaction between fex-SFN and BZ or NFX on H9c2 cells infected with the Y strain and the results were analysed at the IC50 level. As expected, the dose-response curves showed potent and concentration-dependent effects of the nitro drugs singly against intracellular parasites (Fig. 2). The IC50 value for BZ and NFX was 1.53 ± 0.52 and 0.65 ± 0.12 μ m, respectively; similarly, the dose-dependent effect of fex-SFN revealed an IC50 value of 3.49 ± 1.32 μ m (Fig. 2C). When used in combination with BZ or NFX, a leftward shift of the combined therapy curve for fex-SFN was identified, suggesting a positive effect resulting from the drug combinations. This effect was confirmed by the analysis of the ΣFICs that revealed ΣFIC50 = 0.675 ± 0.15 for the combination of BZ and fex-SNF and 0.695 ± 0.20 for the combination of NFX and fex-SFN (Fig. 2C), indicating an additive effect.

Fig. 2. Anti-Trypanosoma cruzi activity. In vitro dose-response curves of H9c2 cells infected with Trypanosoma cruzi Y strain treated with nitro compounds in monotherapy or in combination for 72 h. (A) Treatment with fex-SFN, BZ and BZ/fex-SFN. (B) Treatment with fex-SFN, NFX and NFX/fex-SFN. Each point of the dose-response curves corresponds to the mean of two independent experiments. (C) IC50 and ΣFIC50 of nitrocompounds alone and in combination.
Considering the results of the in vitro experiments, we evaluated the effect of the same drug combinations in an acute model of murine T. cruzi infection. In this case, suboptimal doses of each drug (i.e. those that did not induce cure in the experimental murine model infection) (Mazzeti et al., Reference Mazzeti, de Diniz, Gonçalves, Nascimento, Spósito, Mosqueira, Machado-Coelho, Ribeiro and Bahia2018) were used in combination (BZ 50 mg kg−1, fex-SFN 50 mg kg−1 and NFX 25 mg kg−1). Figure 3 shows the parasitemia curves of infected mice until 50 days after infection. Untreated mice presented with a classic parasitemia curve peaking at day 8 after inoculation (Fig. 3), leading to the death of all (100%) the animals between 13 and 18 days post-infection (Table 1). All treatments were effective in reducing parasitemia compared with that in the untreated infected control (P = 0.0007) (Fig. 3A). The area under the parasitemia curve of the animals treated with the drug combinations was significantly reduced compared to those in the respective monotherapies (Fig. 3B).

Fig. 3. Acute treatment with benznidazole (BZ), nifurtimox (NFX), the sulfone metabolite of fexinidazole (fex-SFN) or their combinations in mice infected with Trypanosoma cruzi Y strain. Parasitemia profile in mice treated for 20 days with BZ 100 or 25 mg kg−1; NFX 25 mg kg−1; fex-SFN 50 mg kg−1; their combinations (BZ 50 mg kg−1 + fex-SFN 50 mg kg−1 and NFX 25 mg kg−1 + fex-SFN 50 mg kg−1) and infected untreated control. Parasitemia was assessed during the treatment until 30 days post-treatment. (B) Area under the parasitemia curves of treated and infected mice.
Table 1. Effect of treatment with nitro compounds (monotherapy or combination) in acute infection of mice by Trypanosoma cruzi Y straina

BZ, benznidazole; NFX, nifurtimox; fex-SFN, sulfone metabolite of fexinidazole.
a Female Swiss (18–22 g) were inoculated with 5 × 103 trypomastigotes of Y T. cruzi strain. Treatments were started on the 4 days after infection, by gavage, for 20 consecutive days.
b Positive results in FBE (fresh blood examination) before immunosuppression with cyclophosphamide and PCR (polymerase chain reaction) assays, performed 30 days post-treatment. Parasitemia relapse after the end of treatment and the time (days) ± standard deviation.
c Cure rates based on negative results in fresh blood examination before and after immunosuppression with cyclophosphamide; blood qPCR (polymerase chain reaction) assays, performed 30 and 180 days post-treatment and tissue qPCR assays performed 180 days post-treatment.
Additionally, suboptimal doses of fex-SFN, BZ and NFX alone, although not inducing cure in animals, were able to reduce the parasitic load to levels undetectable by fresh blood tests and prevent mortality in all treated mice (Table 1). As the number of doses required to induce suppression of parasitemia is an indication of the activities of nitro compounds, we analysed the time to suppress the parasitemia among the groups. Treatment with fex-SFN suppressed parasite detection after 11.43 ± 4.58 doses; for BZ 50 mg kg−1, 5.40 ± 4.96 doses were required and for NFX, 7.71 ± 4.89 doses. Interestingly, nitro drug associations led to a faster suppression of parasitemia than with monotherapies, with 1.28 ± 0.49 doses of BZ/fex-SFN and 1.37 ± 0.52 doses of NFX/fex-SFN comparable to standard treatment with BZ 100 mg kg−1 (1.43 ± 0.77 doses) (Table 1). After the end of the treatment, a natural parasitemia relapse was observed in all groups; however, this relapse was faster and in a larger number among those animals treated with monotherapies compared to those treated with combined therapy (Table 1).
To effectively verify the therapeutic potential of combined treatment using fex-SFN with BZ or NFX, we performed a stringent cure control protocol. The investigation of the reactivation of parasitism until 180 days after treatment was performed using blood/tissue PCR and immunosuppression with cyclophosphamide. In all monotherapy-treated mice, the parasite or its DNA was detected, evidencing therapeutic failure, as expected. Interestingly, when these suboptimal doses were administered in combination, they induced complete neutralization of parasitism in 83.3% (4 out of 6) of mice in the BZ/fex-SFN-treated group and in 75.0% (6 out of 8) of mice treated with NFX/fex-SFN, as these cure rates were higher than those observed with the reference treatment of BZ 100 mg kg−1 (57.1%, 4 out of 7) (Table 1). Likewise, the parasitic cardiac load confirmed the results, since in the group treated with NFX/fex-SFN, parasite DNA was detected in 25% of animals (2 out of 8, with 1.22 ± 0.31 parasites/25 μg of DNA). Trypanosoma cruzi DNA was not detected in the cardiac tissue of animals treated with BZ/fex-SFN (0 out of 6).
Interestingly, despite combining compounds that belong to similar therapeutic classes, we did not observe toxic effects resulting from the combined therapies. The analyses of the body weight of the mice during the treatment period demonstrated that, while 28.6% infected and untreated mice lost weight as a result of acute infection, the treatments prevented this effect (Table 2). In addition, the weight gain observed in treated groups was significantly higher than in infected control, except for the NFX-treated groups. Similarly, all treatments were able to reduce liver enzyme levels in T. cruzi infection. Table 2 shows the levels of AST and ALT enzymes evaluated in the mice serum on the last day of treatment (and 15 days post-infection for infected and untreated mice). The BZ/fex-SFN-treated group reached AST and ALT levels similar to uninfected animals, and the NFX/fex-SFN-treated group showed ALT levels similar to uninfected controls. These reduced levels may reflect the decreased parasitic load in liver tissue, which would correspond to a decrease in tissue damage and safety of treatment.
Table 2. Toxicity of treatment with nitro compounds (monotherapy or combination) in acute infection of mice by Trypanosoma cruzi 1

BZ, benznidazole; NFX, nifurtimox; fex-SFN, sulfone metabolite of fexinidazole.
1Female Swiss (18–22 g) were inoculated with 5 × 103 trypomastigotes of Y T. cruzi strain. Treatments were started on the 4 days after infection, by gavage, for 20 consecutive days.
2Levels of liver enzymes aspartate aminotransferase (AST) and alanine aminotransferase (ALT) in the animals' serum on the last day of treatment. Levels of AST and ALT in serum of infected control animals were measured on the 15th day of infection.
a = statistical difference among infected control, P < 0.05.
b = statistical difference among non-infected control, P < 0.05.
Discussion
Incremental innovation to existing pharmaceutical products has been occurring in the form of supplementary approvals for new dosages, formulations and indications (Berndt et al., Reference Berndt, Cockburn and Grépin2006). This strategy has been fruitful in expanding the pharmacotherapeutic options of a number of diseases, and it is especially relevant to neglected ones. In this line and considering the scarce panel of new anti-T. cruzi molecules, alternative formulations (Leonardi et al., Reference Leonardi, Bombardiere and Salomon2013; Spósito et al., Reference Spósito, Mazzeti Silva, de Oliveira Faria, Urbina, Pound-Lana, Bahia and Mosqueira2017; Seremeta et al., Reference Seremeta, Arrúa, Okulik and Salomon2019; Mazzeti et al., Reference Mazzeti, Oliveira, Gonçalves, Schaun, Mosqueira and Bahia2020; Rial et al., Reference Rial, Arrúa, Natale, Bua, Esteva, Prado, Laucella, Salomon and Fichera2020) and dosing regimens to reference medicines (Rial et al., Reference Rial, Scalise, Arrúa, Esteva, Salomon and Fichera2017; Kratz et al., Reference Kratz, Garcia Bournissen, Forsyth and Sosa-Estani2018; Mazzeti et al., Reference Mazzeti, de Diniz, Gonçalves, Nascimento, Spósito, Mosqueira, Machado-Coelho, Ribeiro and Bahia2018; Perin et al., Reference Perin, da Fonseca, de Carvalho, Carvalho, Madeira, da Medeiros, Molina, Correa-Oliveira, Carneiro and de Vieira2020) have been explored in chemotherapy for Chagas disease. In parallel, the trypanocidal potential of another nitro drug has been revisited, allowing the identification of a promising candidate, such as fexinidazole, which has been recently included as a possible candidate to treat chronic T. cruzi infection (Patterson and Fairlamb, Reference Patterson and Fairlamb2019; DNDi, 2020). Despite the safety concerns regarding this pharmacological class, nitro compounds have been explored with success as a source of a potential treatment for other kinetoplastid-related diseases (Patterson and Fairlamb, Reference Patterson and Fairlamb2019), such as human African trypanosomiasis (Janssens and De Muynck, Reference Janssens and De Muynck1977; Torreele et al., Reference Torreele, Bourdin Trunz, Tweats, Kaiser, Brun, Mazué, Bray and Pécoul2010; Eperon et al., Reference Eperon, Balasegaram, Potet, Mowbray, Valverde and Chappuis2014; Tarral et al., Reference Tarral, Blesson, Mordt, Torreele, Sassella, Bray, Hovsepian, Evène, Gualano, Felices and Strub-Wourgaft2014; Mesu et al., Reference Mesu, Kalonji, Bardonneau, Mordt, Blesson, Simon, Delhomme, Bernhard, Kuziena, Lubaki, Vuvu, Ngima, Mbembo, Ilunga, Bonama, Heradi, Solomo, Mandula, Badibabi, Dama, Lukula, Tete, Lumbala, Scherrer, Strub-Wourgaft and Tarral2018) and leishmaniasis (Wyllie et al., Reference Wyllie, Patterson, Stojanovski, Simeons, Norval, Kime, Read and Fairlamb2012; Koniordou et al., Reference Koniordou, Patterson, Wyllie and Seifert2017).
In this work, we demonstrated in a well-established preclinical model that combinations using fex-SFN with BZ or NFX are well tolerated and more effective than monotherapies at the same doses and even higher than standard BZ treatment, suggesting a positive interaction among the drugs. Although a number of studies have investigated the potential of combination therapy to increase the efficacy and reduce the toxicity of the reference treatments for Chagas disease (Araujo et al., Reference Araujo, Martins-Filho, Pereira and Brener2000; de Diniz et al., Reference Diniz, Urbina, Andrade, Mazzeti, Martins, Caldas, Talvani, Ribeiro and Bahia2013; Strauss et al., Reference Strauss, Lo Presti, Bazán, Baez, Fauro, Esteves, Sanchez Negrete, Cremonezzi, Paglini-Oliva and Rivarola2013; Assíria Fontes Martins et al., Reference Assíria Fontes Martins, de Figueiredo Diniz, Mazzeti, da Silva do Nascimento, Caldas, Caldas, de Andrade, Ribeiro and Bahia2015; Providello et al., Reference Providello, Carneiro, Portapilla, do Vale, Camargo, Tirapelli and de Albuquerque2018; Guedes-da-Silva et al., Reference Guedes-da-Silva, da Batista, Da Silva, Pavão, Batista, Moreira, Souza, Britto, Rachakonda, Villalta, Lepesheva and de Soeiro2019; Mazzeti et al., Reference Mazzeti, de Diniz, Gonçalves, WonDollinger, Assíria, Ribeiro and Bahia2019; Rocha Simões-Silva et al., Reference Rocha Simões-Silva, Brandão Peres, Britto, Machado Cascabulho, de Melo Oliveira, Nefertiti da Gama, França da Silva, Lima da Costa, Finamore Araújo, Diego de Souza Campos, Meuser Batista, Cristina Demarque, da Cruz Moreira and de Nazaré Correia Soeiro2019), to the best of our knowledge, the interaction among nitro drugs has been sparsely studied (Cencig et al., Reference Cencig, Coltel, Truyens and Carlier2012).
First, the toxicity profile and nature of the interaction between BZ/fex-SFN and NFX/fex-SFN were assessed in vitro. The results confirmed that nitro drug derivatives are active on the micromolar scale (Bahia et al., Reference Bahia, Nascimento, Mazzeti, Marques, Gonçalves, Mota, de Diniz, Caldas, Talvani, Shackleford, Koltun, Saunders, White, Scandale, Charman and Chatelain2014; Moraes et al., Reference Moraes, Giardini, Kim, Franco, Araujo-Junior, Schenkman, Chatelain and Freitas-Junior2015; Mazzeti et al., Reference Mazzeti, de Diniz, Gonçalves, WonDollinger, Assíria, Ribeiro and Bahia2019) and showed that such combinations resulted in an additive effect in the absence of toxicity to host cells, with mean ΣFIC ranging from 0.57 to 0.84 (Fig. 1). Although there are no clear parameters to guide in vitro to in vivo progression related to anti-T. cruzi combinations (Machado et al., Reference Machado, Bahia, Caldas, Mazzeti, Novaes, Vilas Boas, de Santos, Martins-Filho, Marques and de Diniz2020), we believe that is useful to move additive and non-toxic mixtures to evaluation in murine infection as a way to expand the preclinical data on combination therapy for Chagas disease.
In the next step, we performed an in vivo evaluation of combined treatments using suboptimal regimens – half of the standardized dose of each drug considering experimental chemotherapy (Filardi and Brener, Reference Filardi and Brener1987; Bahia et al., Reference Bahia, de Andrade, Martins, da Silva do Nascimento, de Diniz, Caldas, Talvani, Trunz, Torreele and Ribeiro2012, Reference Bahia, Nascimento, Mazzeti, Marques, Gonçalves, Mota, de Diniz, Caldas, Talvani, Shackleford, Koltun, Saunders, White, Scandale, Charman and Chatelain2014; Mazzeti et al., Reference Mazzeti, de Diniz, Gonçalves, Nascimento, Spósito, Mosqueira, Machado-Coelho, Ribeiro and Bahia2018) as monotherapy and combined. These doses, while effective in suppressing the parasitemia, were unable to induce parasitological cure when used as monotherapy (Fig. 1, Table 1). On the other hand, when used concomitantly, they induced complete resolution of parasitism in 75.0% (NFX/fex-SFN) to 83.3% (BZ/fex-SFN) of infected mice (Table 1), suggesting a benefit from combined therapy. Classifying the nature of the interaction between drugs in vivo in the context of experimental Chagas disease remains a challenge. Unlike what is observed in in vitro experiments, where FIC and combination indexes can be calculated from dose-effect curves, in vivo analyses do not allow the estimation of parameters such as IC50 or IC90. As a result, the effect of the combination was determined from the comparison with monotherapy and the reference treatment (Cencig et al., Reference Cencig, Coltel, Truyens and Carlier2012; Assíria Fontes Martins et al., Reference Assíria Fontes Martins, de Figueiredo Diniz, Mazzeti, da Silva do Nascimento, Caldas, Caldas, de Andrade, Ribeiro and Bahia2015; de Diniz et al., Reference Diniz, Mazzeti, Caldas, Ribeiro and Bahia2018; Mazzeti et al., Reference Mazzeti, de Diniz, Gonçalves, WonDollinger, Assíria, Ribeiro and Bahia2019; Rocha Simões-Silva et al., Reference Rocha Simões-Silva, Brandão Peres, Britto, Machado Cascabulho, de Melo Oliveira, Nefertiti da Gama, França da Silva, Lima da Costa, Finamore Araújo, Diego de Souza Campos, Meuser Batista, Cristina Demarque, da Cruz Moreira and de Nazaré Correia Soeiro2019).
Considering that the total dose of nitro compounds in the combination was equivalent or higher than the full standard dose (BZ 100 mg kg−1 or NFX 50 mg kg−1), it would be reasonable to assume that the observed effects were the result of the total concentration of nitro drugs in the combination. However, the cure rates observed for combinations were higher than those obtained for the reference treatment with BZ (57.1%) (Table 1), demonstrating the greater effect of the drug combinations, particularly BZ/fex-SFN, compared to those with each drug alone. The mechanism of action of nitro drugs is not fully understood, but it involves similar pathways to BZ, NFX and fex-SFN. Further PK/PD analyses need to be performed to investigate the molecular basis of the in vivo interaction among BZ/fex-SFN and NFX/fex-SFN. Interestingly, pharmacodynamically additive and synergistic drug combinations from molecules in the same pharmacological class and with the same mechanism of action have been demonstrated in the context of antiretroviral (Wertheimer and Morrison, Reference Wertheimer and Morrison2002) and antibacterial chemotherapy (Jia et al., Reference Jia, Zhu, Ma, Cao, Li and Chen2009).
Herein, the data presented provide important information for the evaluation of reduced doses of nitro drug combinations in the treatment of human diseases in an attempt to increase efficacy. While one of the goals of combination therapy is to reduce drug doses and adverse effects, the potential for toxicity of the combined treatment in the host needs to be monitored to ensure that there is no potentiation of the adverse effects. In preclinical assays, an important aspect to note is whether the treatment induces liver damage (Amacher, Reference Amacher1998). Likewise, our data showed that the level of liver enzymes (AST and ALT) detected in the serum of the animals treated with nitro drug combinations on the last day of treatment was significantly lower than those in the serum of the infected control animals and close to the level found in the serum of uninfected and untreated animals. In addition, this may be a reflection of the decrease in the parasitic load in hepatic tissue that would correspond to a decrease in tissue damage (Novaes et al., Reference Novaes, Santos, Cupertino, Bastos, Oliveira, Carvalho, Neves, Oliveira and Talvani2015). In the same way, weight gain and mortality rates of infected and treated mice demonstrated the benefit of treatment in the absence of apparent toxicity.
Altogether, our results indicated that the combination of fex-SFN with the first-line drugs BZ or NFX is a promising alternative for the treatment of Chagas disease. Considering that the toxicological profile of this pharmacological class is related to higher doses or prolonged regimens (Pérez-Molina and Molina, Reference Pérez-Molina and Molina2018), the positive interaction observed could allow the reduction of the doses of each compound without changing or increasing the effectiveness of the treatment. Further experiments using different T. cruzi strains, infection phases and PK/PD profiles of monotherapy vs combination therapy need to be carried out to validate this strategy. Although many answers are needed, this study is the starting point to explore the potential effects of nitro drug combinations in preclinical models of T. cruzi infection and other kinetoplastid-related diseases.
Acknowledgements
We also thank the ‘Laboratório Piloto de Análises Clínicas’ (LAPAC/UFOP) for the help with hepatic enzyme analyses.
Financial support
This work was funded by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) – Brazil (research fellowship to MTB and fellowship ALM); Universidade Federal de Ouro Preto (UFOP) – Brazil; Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) – Brazil; Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ) – Brazil (post-doctoral fellowship to ALM number E-26/202.368/2019).
Conflict of interest
None.
Ethical standards
The Ethics Committee in Animal Research at the Federal University of Ouro Preto, Minas Gerais, Brazil (UFOP), approved in vivo procedures and experimental conditions (number 2009/17).