Introduction
The differentiation between malaria and other febrile infectious diseases, in the absence of laboratory confirmation, represents a great challenge in clinical practice, especially in endemic areas. Although it responds satisfactorily to drug therapy in most cases, malaria is often associated with delayed diagnosis and treatment, which contributes to worse disease progression and increased morbidity and mortality (Raposo, Reference Raposo2006). Several factors contribute to malaria delayed diagnosis, such as the fragile structure of local health services; deficient training of human resources; poor diagnosis quality control; and lack of rapid diagnostic methods in remote areas. The presence of asymptomatic patients and little information among the population about malaria transmission are factors that also contribute to the problem (Raposo, Reference Raposo2006).
In the study conducted by Moura and Ferreira (Reference Moura and Ferreira2010), involving patients infected with Plasmodium vivax malaria at the city of Belém, Pará/Brazil, it took an average of 10 days for the diagnosis suspicion. This period was significantly longer than the period for diagnosis of malaria cases occurring in the countryside of Pará, in other states, and in others countries, especially those in the mining area. This lag is attributed to a delayed suspicion of malaria from health professionals, commonly associating it with an exclusive disease of forest areas and disregarding the possibility of its occurrence in a city, for instance Belém, capital of Pará state, and its metropolitan region (Moura and Ferreira, Reference Moura and Ferreira2010).
However, clinical analysis of risk factors could help health professionals to determine when a patient, with a history of fever, is most likely to be diagnosed with malaria. This would be possible in areas devoid of haemoscopy, as suggested by Genton et al. (Reference Genton, Smith, Baea, Narara, Al-Yaman, Beck, Hii and Alpers1994), or even in areas where haemoscopy is available, considering the difficulty in differentiating malaria – which is a febrile and systemic disease – from other infectious diseases that also have fever as an important clinical manifestation (Genton et al., Reference Genton, Smith, Baea, Narara, Al-Yaman, Beck, Hii and Alpers1994). Malaria surveillance includes knowledge and analysis of clinical factors, to allow the immediate referral of patients to diagnostic reference institutes for early treatment and, therefore, shorten the disease cycle, mitigating social losses and economic costs. This research aims to determine whether the combination of epidemiological characteristics of the patient's history and clinical manifestations predict malaria.
Materials and methods
This is a diagnostic test study, with a cross-sectional design, using the clinical prediction rules (Fletcher and Fletcher, Reference Fletcher and Fletcher2006). The research was conducted and coordinated by the Laboratory of Clinical Essays in Malaria of the Evandro Chagas Institute (IEC), in Ananindeua, Pará/Brazil, from December 2012 to June 2013. The research was approved by IEC Research Ethics Committee (opinion number 162 500, of 03/12/2012), following the guidelines of the National Council for Research Ethics (CONEP). A clinical−epidemiological questionnaire was filled with relevant information to malaria diagnosis, such as history of travel to an endemic malaria area, past malaria history, signs and symptoms (fever, chills, headache, arthralgia, low back pain, nausea, vomiting, abdominal pain, diarrhoea, asthenia, cough, anorexia, pallor, hepatomegaly, splenomegaly, altered consciousness). Subsequently, the participants underwent a thick blood smear test to seek for Plasmodium.
Recruitment criteria
In the Malaria Clinical Trial Program of Evandro Chagas Institute, individuals look for malaria diagnosis spontaneously or referred by the public or private health network because they have clinical–epidemiological data suggestive of malaria. It is important to mention that about 80% of this demand is spontaneous.
One hundred sixty-six adult individuals were invited to participate in the research, presenting clinical findings suggestive of malaria, of both genders and aged 18 years or over, excluding patients who refused to sign the informed consent form (ICF), patients who sought the programme with a confirmed diagnosis of malaria and pregnant patients. As the clinical prediction rule was used, individuals without clinical and epidemiological findings were also not included in the research.
After prior consent, a clinical–epidemiological form was filled out, where the following were evaluated: origin, history of travel to an endemic area, past malaria, time of illness, signs and symptoms (fever, chills, headache, arthralgia, low back pain, nausea, vomiting, abdominal pain, diarrhoea, asthenia, cough, anorexia, pallor, hepatomegaly, splenomegaly, altered consciousness). Later, the individual was submitted to the laboratory diagnosis of malaria, therefore, it was an independent ‘blind’ comparison with a confirmative laboratory diagnosis.
Diagnosis of malaria
The search for plasmodium in peripheral blood was performed using the thick blood smear method according to Antuñano (Reference Antuñano, Antuano and Schumunis1988), using blood obtained by digital puncture. Thick blood smear remains the gold standard method for malaria diagnosis. Evandro Chagas Institute is a reference centre for malaria in the Brazilian Amazon with expert microscopists in malaria diagnosis. In this study, each sample was independently evaluated by two microscopists, both expert in performing malaria diagnosis through thick blood smear method. There were no discrepancies in their diagnosis.
The thick blood smear has reduced sensitivity in cases of asymptomatic malaria in which, in general, individuals have a parasitaemia of less than 10–20 parasites mm−3 of blood (Brasil, 2020). Asymptomatic individuals were not included in this study. Polymerase chain reaction (PCR) exams were not performed. When the microscopists of the Malaria Clinical Trial Program of Evandro Chagas Institute do not find the parasite in the 100 fields they routinely extend the reading of the slides up to 500 fields.
Statistical analysis
Quantitative results were stored in Microsoft Office Excel 2007 spreadsheet software. Statistical analysis was performed using BioEstat 5.0 software (Ayres et al., 2007). Multiple logistic regression analysis was used to determine which clinical and epidemiological findings were the most associated with malaria. Those findings associated with malaria outcome were considered independent predictors.
Then, the conditional probability was calculated, evaluating the sensitivity and specificity, with their respective estimates of uncertainty (Herbert, Reference Herbert2013), positive and negative predictive value and the likelihood ratios, which can be used to calculate the probability of having or not the disease after a positive or negative test, and the accuracy, which gives a proportion of correct answers for the test. The calculation was made for one of the findings alone and with the combination of two or more findings. Hypotheses: HO: It is not possible through clinical–epidemiological analysis to make the presumptive diagnosis of malaria. H1: It is possible through clinical analysis. A threshold of 0.05 (5%) was adopted for rejection of the null hypothesis (H0).
Results
In the period from December 2012 to May 2013, 166 patients with an average age of 14.3 ± 39.7 years old were included, 53.6% male and 46.4% female. The sample size (166 individuals) was not calculated in advance, but was the result of the spontaneous demand of individuals who sought a diagnosis of malaria at the Malaria Clinical Trial Program of Evandro Chagas Institute during the specified period because they had signs and symptoms suggestive of malaria.
Diagnostic investigation detected 22.3% (37/166) of individuals with positive thick blood smear for plasmodium, all due to P. vivax. There was a male predominance, without statistical significance (Table 1).
Table 1. Epidemiological and clinical features among individuals who performed thick blood smear for malaria diagnosis, followed by multiple logistic regression analysis

a Corrected χ 2 (Yates).
b Exact Fisher's test.
Malaria has a classic clinical triad of fever, headache and chills. For all patients, the following symptoms most frequent were fever (63.1%), chills (7.5%) and headache (6.3%). In positive cases for malaria, the triad had a more expressive frequency, 81.1%, compared to cases of negative thick blood smear, 65.1% (Table 1). In isolation, the most frequent signs and symptoms in patients with positive thick blood smear were fever (94.6%), chills (91.9%), headache (83.8%), low back pain (78.4%), asthenia (75. 7%), anorexia (69.4%), abdominal pain (2.9%) and cough (2.9%).
Among the variables analysed as predictive for positive thick blood smear, it was observed that personal history of travel to an endemic malaria area and past malaria infection (PMI) were significantly associated with malaria (P < 0.05, χ 2 test). The malaria triad, fever and headache had no significant association with a positive thick blood smear, as shown in Table 1 (χ 2 test and exact Fisher's test, P > 0.05).
Past infection of malaria (odds ratio (OR) = 3.9, confidence interval (CI) (95%) = 1.6–9.4; P = 0.0021) and travel history (TH) to an endemic area of malaria (OR = 4.15, CI (95%) = 1.5–10.1; P = 0.0038) remained significant among all clinical and epidemiological variables submitted to multiple logistic regression (Table 1).
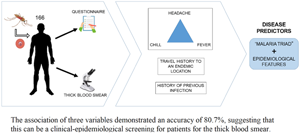
In the isolated assessment of epidemiological data and clinical signs and symptoms by calculating the conditional probability (screening test), there was a higher sensitivity for fever (94.6%) and greater specificity for past malaria history (68.2%), respectively with 23.5% (low) and 67.5% accuracies (CI 95%, respectively = 82.3–98.5 and 59.7–75.6). The malaria triad showed a sensitivity of 81.1% (CI 95% = 65.8–90.5) and an accuracy of 45.2%. PMI and history of travelling to an endemic malaria area showed above 60% of sensitivity (CI 95%, respectively = 48.7–78.1 and 60.0–87.5) and accuracy. In combined analysis of these variables, fever with chills had the highest sensitivity (91.9%) (CI 95% = 78.7–97.2), but low accuracy (38.5%). High specificity (91.5%) was found in the association of malaria triad, PMI and history of travel to endemic malaria area (which along with anorexia, was higher – 94.6%), with good accuracy (80.7%) (CI 95%, respectively = 85.3–95.1 and 91.2–98.3) (Table 2).
Table 2. Probability calculation (screening test) on epidemiological and clinical features among individuals who performed thick blood smear for malaria diagnosis

Discussion
Malaria is a highly prevalent endemic disease in areas of low socioeconomic development. The most affected sites include Africa, Southeast Asia and Brazilian Amazon (Menkin and Winders, Reference Menkin and Winders2019; WHO, 2019). Prevalence of malaria in the state of Pará in 2013 was 0.32%, according to the number of new cases in the Epidemiological Bulletin (Brasil, 2015) and the population of the state registered in the census by Brazilian Institute of Geography and Statistics (IBGE) in 2010 (IBGE, 2010).
Clinical diagnosis is a tool widely used in tropical countries, due to the difficult access to laboratory tests (Gitta and Kilian, Reference Gitta and Kilian2019), although the World Health Organization (WHO) recommends the thick blood smear parasitological test in all suspected cases of malaria (WHO, 2015). In addition, because of poor conditions experience and absence of reliable technology, health professionals may even treat patients with negative rapid diagnostic test (RDT) result, ignoring the test's predictive value (Ansah et al., Reference Ansah, Narh-Bana, Epokor, Akanpigbiam, Quartey, Gyapong and Whitty2010; Reynolds et al., Reference Reynolds, Wood, Mikhail and Ahmad2012).
In this study, was found that the choice of covariates for malaria prediction shows significant deviation in sensitivity and specificity. As shown in Table 2, TH to malaria endemic places and PMI are the most accurate covariates, and when associated to the clinical triad, present 80.7% of accuracy, being the best form of variables association.
Among variables analysed separately, fever was the most prevalent, present on 63.1% of the suspected cases and 94.6% (CI 95% = 82.3 – 98.5) of the positive cases, with no significant association. Also, the variable headache had no significant association in this study (exact Fisher's test P = 0.56). Anorexia seems to be the best symptom as a lone predictor, but when associated with the malaria triad, its specificity is lower than association with TH and PMI. Other similar studies have concluded that the malaria triad can be very useful in endemic areas, however it is important to remember that fever, chills and headache are common symptoms for other tropical diseases, which explains the clinical tool's low specificity (Tangpukdee et al., Reference Tangpukdee, Duangdee, Wilairatana and Krudsood2009). Also, one of these studies concluded that this tool has better use for children than for adults (Genton et al., Reference Genton, Smith, Baea, Narara, Al-Yaman, Beck, Hii and Alpers1994).
Although the malaria triad (fever, chills and headache) had a sensitivity of 81.1% (CI 95% = 65.8 – 90.5), it had low accuracy (45.2%) and, therefore, had a low proportion of correct answers in the diagnosis of malaria (due to its low specificity), not being feasible to carry out an accurate diagnosis of the disease. In 2012, Oladosu and Oyibo (Reference Oladosu and Oyibo2012) pointed out the excess of diagnosis and treatment (respectively, overdiagnosis and overtreatment) for malaria on endemic areas, based only on clinical features. They found that in a group of 1211 Nigerian children and adolescents (0–12 years), only 20.7% (251) of them had a positive microscopic examination for malaria, although the rest (79.3%) had mistakenly received antimalarials, thus losing their opportunity to investigate other causes of febrile syndrome. Other studies carried out in the African continent (Kenya and Guinea-Bissau) also demonstrated an association of clinical diagnosis with overdiagnosis and overtreatment (O'Meara et al., Reference O'Meara, Bejon, Mwangi, Okiro, Peshu, Snow, Newton and Marsh2008; Santoguina et al., Reference Santoguina, Walther, Drakeley, Nwakanma, Oriero, Correa, Corran, Conway and Walther2009).
The acknowledge of malaria clinical manifestations, due to its variable accuracy, as demonstrated in this study, should not be used as the sole criterion for diagnosis and thus establishing malaria treatment in endemic areas. It can, however, decrease morbidity due to the disease, as Amexo et al. (Reference Amexo, Tolhurst, Barnish and Bates2004) pointed out, although this attitude, sometimes observed in remote areas of the Brazilian Amazon, may lead to increase rates of malaria overdiagnosis and overtreatment.
The association of the variables ‘malaria triad’, ‘history of travel to an endemic malaria location’ and ‘history of previous malaria infection’ showed a sensitivity of 43.2% (CI 95% = 28.6 – 59.1), below the recommended for the use of RDTs for malaria, that are at least 95%, to avoid false positives in potentially fatal treatable diseases (WHO, 2000; O'Meara et al., Reference O'Meara, Bejon, Mwangi, Okiro, Peshu, Snow, Newton and Marsh2008; Boyce and O'Meara, Reference Boyce and O'Meara2017). On the other hand, the accuracy of the association of these variables of 80.7% and specificity of 91.5% (CI 95% = 85.3 – 95.1) could better direct patients to perform thick blood smear test, the gold malaria standard exam, to avoid overdiagnosis and overtreatment (Bisoffi et al., Reference Bisoffi, Gobbi, Bounfrate and Ende2012).
RDT's could also be used in remote locations of malaria endemic areas, where the use of microscopy is hampered by geographic access, lack of electricity or a qualified professional. According to the National Plan to Combat Malaria (PNCM), the kit used for the diagnosis of P. vivax (s.d.-BIOLINE MALARIA AG Pf) has 98.2% sensitivity and 99.3% specificity. These values are close to the CareStart Malaria Pf / Pv Combo kit (99% and 99%) and have greater sensitivity than the Falcivax Device Rapid kit (77%), while specificity remains close (99%) (Agarwal et al., Reference Agarwal, Choi, Johnson and Takwoingi2020).
The epidemiological variables TH and PMI showed an accuracy of 60.8% and 67.5%, respectively, surpassing all the isolated variables analysed, which despite not showing superiority when associated with other variables, such as the triad, can be useful in the case of asymptomatic patients. The high transmission in endemic areas provided the creation of a large contingent of asymptomatic infected patients, where the immunological protection developed did not deprive them of the infection (Tangpukdee et al., Reference Tangpukdee, Duangdee, Wilairatana and Krudsood2009). In these cases, with the absence of clinical symptoms, the use of epidemiological variables (TH or PMI) could serve as a screening tool for malaria, to reduce transmission. Therefore, we understand that these clinical tools should be used only to predict malaria, because its use to diagnose can result in overtreatment, mistreatment and iatrogenesis (Ansah et al., Reference Ansah, Narh-Bana, Epokor, Akanpigbiam, Quartey, Gyapong and Whitty2010; Reynolds et al., Reference Reynolds, Wood, Mikhail and Ahmad2012).
We acknowledge that this study faces limitations, as sample size was not calculated in advance. We also faced other limitation regarding the sample size, although the data presented were robust enough to allow statistical analysis. Nevertheless, the results due only by P. vivax should not be extrapolated to P. falciparum malaria, which, by its characteristics, have greater potential for severity, though this plasmodium specie accounted for only 12% of cases of malaria in the Brazilian Amazon I 2016 (Brasil, 2018).
This research protocol showed that an adequate clinical–epidemiological evaluation can serve as a predictor for malaria due to its high specificity, however, the low sensitivity prevents its use as a diagnostic test. On the other hand, the absence of TH to an endemic malaria area and the absence of PMI, both with low specificity and sensitivity, are more useful, to rule out a diagnosis of malaria, due to its accuracy values (60.8% and 67.8%, respectively), which are better than any other variables isolated. We find TH, PMI and the malaria triad the most fundamental variables to predict the disease, being useful for investigation, but not recommended for final diagnosis (Genton et al., Reference Genton, Smith, Baea, Narara, Al-Yaman, Beck, Hii and Alpers1994).
Conclusions
The analysis of the results obtained in the present research leads us to reach the following conclusions: especially in remote areas, where it is difficult to access laboratory confirmation, an excellent clinical–epidemiological assessment associated with malaria classic triad of symptoms may be highly specific for its assumption diagnosis (despite low sensitivity), and may contribute to immediate referral of patients to diagnostic reference institutes for early treatment. Furthermore, even in areas where microscopy is available, malaria clinical–epidemiological predictors can contribute to prevent delayed diagnosis suspicion and impact morbidity and mortality rates.
Data
Data reported in this paper come from patients assisted at Evandro Chagas Institute. The study followed all standards regarding the inclusion of patients in accordance with resolution 196/96 and was approved by IEC Ethics Committee, under protocol number 162 500/2012. If you are interested in accessing the database, it is necessary to contact the corresponding author who will contact the IEC board, asking for the release of data from the institution's collection.
Acknowledgements
We thank Evandro Chagas Institute for technical and administrative support generously provided during this study. Funding for this project was made possible by Amazon Foundation for Support to Studies and Research (FAPESPA).
Author contribution
Ana Maria Revoredo da Silva Ventura: conceptualization, methodology, investigation, project administration and writing (review and editing). Rosana Maria Feio Libonati: conceptualization, methodology, investigation, project administration, funding acquisition and writing (original draft). Tânia do Socorro Souza Chaves: supervision, project administration and writing (review and editing). Paulo Guilherme Souza Lisboa: investigation, data curation and formal analysis. Janaina Maria Rodrigues Medeiros and Juliane Lúcia Gomes da Rocha: writing (original draft, review and editing). Bruno Fernando Barros dos Santos, Wender de Jesus Pena Correa Junior and Henrique Otávio Coutinho Sanches: writing (original draft). Arthur Vinícius de Souza and Gabriela Góes Costa: writing (review and editing).
Financial support
This project is part of the Clinical Trials in Malaria Program of Evandro Chagas Institute parasitology sector, supported by Institutional Program for Scientific Initiation Scholarships of Evandro Chagas Institute (Ananindeua, Brazil)/FAPESPA.
Conflict of interest
The authors declare there are no conflicts of interest.
Ethical standards
This research was approved by Instituto Evandro Chagas Research Ethics Committee under protocol number 162 500/2012. All individuals agreed to voluntarily participate by signing the ICF, after be given full information about possible risks and benefits coming from taking part in the study.