Background
According to the World Health Organization (2020), Palliative Care is “an approach that improves the quality of life of patients (adults and children) and their families who are facing problems associated with life-threatening illnesses; it prevents and relieves suffering through the early identification, correct assessment, and treatment of pain and other problems, whether physical, psychosocial or spiritual”. The experience of suffering or exposure to it is inevitable for those involved in providing palliative care — whether as a patient, family member, or healthcare provider (Garcia et al., Reference Garcia, Domingues Silva and Oliveira da Silva2021). This reality is mostly owing to the nature of palliative care, which involves dealing with and alleviating suffering during and at the end of life (Hartogh, Reference Hartogh2017).
Given that healthcare providers working in palliative care commonly deal with contexts of cumulative loss and suffering (Mills et al., Reference Mills, Ramachenderan and Chapman2020), there is a perceived need to expand the knowledge of strategies that can promote personal well-being for these providers. In a study that aimed to explore distress, self-care, and debriefing practices of palliative care workers, results of the multivariate analysis identified that suffering decreased with the increase in self-care (White et al., Reference White, Murphy and Jeuland2019). The proactive practice of self-care is an important approach to promoting well-being for this population (Beng et al., Reference Beng, Chin and Guan2015; Sansó et al., Reference Sansó, Galiana and Oliver2015; Adams et al., Reference Adams, Chase and Doyle2020), although it is not practised widely across it. For instance, traditionally self-care has not featured prominently in education curricula for healthcare providers in training, so it is perhaps not surprising that many of these providers may find it challenging to balance caring for others with caring for themselves (Mills, Reference Mills2021).
Mindful self-care has been conceptualized as an iterative process that involves (a) mindfulness and assessment of internal needs and external demands and (b) intentional engagement in specific self-care practices to meet needs and demands in a way that effectively addresses personal well-being (Hotchkiss and Cook-Cottone, Reference Hotchkiss and Cook-Cottone2019). Meta-analytic studies have provided growing evidence that mindfulness-based interventions are associated with improved well-being among healthcare providers (Burton et al., Reference Burton, Burgess and Dean2017; Lomas et al., Reference Lomas, Medina and Ivtzan2017).
In developing the Mindful Self-Care Scale (MSCS 33-item), Cook-Cottone(Reference Connor and Davidson2015) integrated elements of mindfulness and other conventional self-care practices. The development of the MSCS (33-item) stemmed from the need to assess mindful self-care in daily life, and also to assess planned mindfulness meditation or other mind-body practices (Cook-Cottone and Guyker, Reference Cook-Cottone2018). The MSCS (33-item) evaluates both formal and informal mindfulness practices. Formal mindful self-care practices usually require the setting aside of time for any given practice (e.g., attending yoga classes, setting aside time for formal meditation), whereas informal practices are generally integrated into daily personal and professional behaviors (Hotchkiss and Cook-Cottone, Reference Hotchkiss and Cook-Cottone2019).
As a middle-income country and the largest country in Latin America, Brazil's health system has seen significant growth in need and provision of hospice and palliative care (Garcia et al., Reference Garcia, Spineli and Eduardo2019). However, despite the subsequent rise in the need for mindful self-care practices to support wellbeing, language limitations have prevented the MSCS (33-item) from being utilized in this population. In that context, the present study aimed to translate, culturally adapt, and validate the MSCS (33-item) in a Brazilian hospice and palliative care context (Supplementary material — Brazilian-Portuguese version of the MSCS).
Methods
Study design
This cross-sectional study was conducted in two stages: (1) translation and cultural adaptation of the MSCS (33-item) (Cook-Cottone and Guyker, Reference Cook-Cottone2018); and (2) evaluation of the psychometric properties of the Brazilian-Portuguese version of the MSCS (33-item).
Participants and sampling
The sample of 330 participants greatly exceeded the recommended 10-subject minimum for investigating validity through factor analysis (Terwee et al., Reference Valentini and Damásio2007). Study participants were Brazilian palliative care providers.
Measures
Participant demographics questionnaire
Participants completed an initial questionnaire, asking about their age (years), gender, marital status, level of education, professional category, and time working in the palliative care field.
Mindful self-care scale (MSCS)
The MSCS (33-item) was developed in the United States as a measure of the self-reported frequency of self-care behaviors (Cook-Cottone and Guyker, Reference Cook-Cottone2018). The instrument consists of 33 items which are divided into six subscales, namely: Physical Care (8 items); Supportive Relationships (5 items); Mindful Awareness (4 items); Self-Compassion and Purpose (6 items); Mindful Relaxation (6 items); and Supportive Structure (4 items) (Hotchkiss and Cook-Cottone, Reference Hotchkiss and Cook-Cottone2019). Additionally, there are three general items, which do not factor into the calculation of the scale's mean score. The total score is the sum of the mean scores of the subscales. The MSCS (33-item) is free to use, the authors request only to be notified regarding the use of the scale in research (Cook-Cottone and Guyker, Reference Cook-Cottone2018).
Self-Compassion Scale—short form (SCS-SF)
Self-compassion involves responding with kindness and compassion to one's own suffering and failures rather than neglecting one's own well-being or engaging in harsh judgements and self-criticism (Neff, Reference Neff2016). The SCS-SF, a scale designed to assess self-compassion (Raes et al., Reference Raes, Pommier and Neff2011), is a shortened version of the self-compassion Scale (SCS) (Neff, Reference Neff2003), validated in Brazil by Souza and Hutz (Reference Souza and Hutz2016). Although the SCS has been the subject of some criticism in the literature, there is compelling evidence supporting its use as a valid and theoretically coherent measure of self-compassion (Neff, Reference Neff2016). The SCS-SF consists of 12 items and has demonstrated a very high correlation with the 26-item SCS when examining total scores. The items are distributed into six subscales, three of which are positive [Self-Kindness (α = 0.55), Common Humanity (α = 0.60) and Mindfulness (α = 0.64)], and three which are negative [Self-Judgement (α = 0.81), Isolation (α = 0.77), and Over-Identification (α = 0.69)] (Raes et al., Reference Raes, Pommier and Neff2011). Response options are arranged on a five-point Likert-type scale, ranging from 1 (Almost never) to 5 (Almost always). When computing a total self-compassion score, the negative subscale items are reverse scored and the mean scores of each subscale calculated, with the total mean scores (the average of the six subscale means) then computed. The scale is available for use on the author's website in several languages (https://self-compassion.org/), including in the Brazilian-Portuguese language.
Brief resilience scale (BRS)
The BRS is an instrument that assesses the level of resilience in adults. It was developed by Smith and colleagues (Reference Smith, Dalen and Wiggins2008) and validated for use in Brazil by Coelho et al. (Reference Coelho, Cavalcanti and Rezende2016). Resilience is generally defined as an individual's ability to overcome stress and adversity and to recover from stressful events (Babić et al., Reference Babić, Babić and Rastović2020). The BRS is a one-dimensional instrument (α = 0.76), consisting of six items (Coelho et al., Reference Coelho, Cavalcanti and Rezende2016). Responses to the items are given from a 5-point Likert scale, ranging from 1 (strongly disagree) to 5 (strongly agree).
Procedures
Translation and cultural adaptation
The translation and adaptation process of the MSCS (33-item) was carried out according to a standardized process as outlined by the European Organisation for Research and Treatment of Cancer — Quality of Life Group Translation Procedure: (1) Forward translations (English-Brazilian Portuguese) performed by two bilingual professionals; (2) Reconciliation (review of the translated versions by a committee of judges to establish a single version in Brazilian Portuguese); (3) Back translations of the revised version (Brazilian Portuguese-English); (4) Proofreading; (5) Pilot-testing; and (6) Final translation (Kulis et al., Reference Kulis, Bottomley and Velikova2017).
In addition to this, the back-translated version was sent to the author of the original instrument for approval, ensuring its conceptual congruence. Before running the pilot test, the Brazilian-Portuguese version of the MSCS (33-item) was subjected to the evaluation of three experienced Brazilian mindfulness instructors who were proficient English speakers and verified that the final version translated into Brazilian Portuguese remained faithful to the conceptual principles related to mindfulness present in the original scale. Based on these evaluations and the standardized procedure of translation and cultural adaptation, the final Brazilian-Portuguese version of the MSCS (33-item) was developed.
Evaluation of psychometric properties of the Brazilian-Portuguese version of the MSCS
Data collection took place between January and April 2021. Recruitment of participants was carried out using a snowball sampling method. More specifically, we invited individuals with the desired characteristics to participate in the study through internet messaging applications (WhatsApp, Telegram, Facebook, and Instagram). The participants’ contact information was obtained through groups of palliative care providers where the authors of this study were members. The aforementioned groups on these apps are composed exclusively of palliative care providers and are aimed at sharing professional information and experiences, including participation in research studies. The providers were contacted individually and were invited to participate voluntarily in the study, as well as to use their personal connections to recruit other palliative care providers who might be interested and eligible to participate in the study (Sadler et al., Reference Sadler, Lee and Lim2010).
The potential participants received a message containing an explanatory text regarding the study and a link that allowed them access more detailed study information and forms. By clicking the link, participants were directed to the consent form, which was completed electronically. Where participants agreed to participate in the study, they were directed to the instruments, all of which were self-applicable. When providers did not consent to participate in the study, they were directed to a page with a message thanking them for considering participation in the study.
The online form was developed using the Google Forms platform, and it was tested for usability and functionality prior to data collection commencing. All the instruments used in the study, along with the consent form, were presented on a specific page of the online form, with a total of five pages altogether. After submitting their responses, participants received an e-mail confirmation of the submission with a link that allowed them to review and change their answers in case participants deemed it necessary.
Data analysis
Socio-demographic data were described in terms of frequencies and percentages. Validity evidence based on the internal structure (AERA et al., 2014; Rios and Wells, Reference Rios and Wells2014) of the Brazilian-Portuguese version of the MSCS (33-item) was assessed through confirmatory factor analysis (CFA) with the weighted least squares mean and variance adjusted (WLSMV) estimation method using the Mplus 8 statistical program (Muthén and Muthén, Reference Muthén and Muthén1998–2017). The following criteria were defined to judge the goodness of fit of the factor model: Comparative Fit Index (CFI) and Tucker–Lewis Index (TLI) [values ≥ 0.90 indicate acceptable fit; values ≥ 0.95 being desirable]; Root Mean Square Error of Approximation (RMSEA) [values ≤ 0.06 indicate fit, with a maximum acceptable limit of 0.08] (Hair et al., Reference Hair, Black and Babin2010; Kline, Reference Kline2011).
The criteria used for item removal were poor factor loadings (<0.40) and large inter-item correlations and conceptual overlap with other items (>0.30). To accept the factor model, these items would be flagged for removal. The correlations between factors (Φ) were evaluated by applying GEOMIN correlations. Reliability was assessed by using the composite reliability (CR) coefficient and Cronbach's α, where values greater than 0.70 were expected (Valentini and Damasio, Reference White, Murphy and Jeuland2016).
Finally, to assess validity evidence based on the relationship with external variables (AERA et al., 2014), Pearson's bivariate correlation analyses were performed to assess the extent to which Brazilian-Portuguese version of the MSCS (33-item) scores significantly associate at the level of p ≤ 0.05 with scores from instruments assessing related constructs, namely self-compassion (SCS-SF) and resilience (BRS). It was hypothesized that significant and positive correlation coefficients would be observed with these variables.
Ethical considerations
This study was approved by the Federal University of Alfenas Research Ethics Committee (CAAE: 30928920.4.0000.5142; Number: 4.274.760; September 14, 2020). All participants received written information concerning the research, and all of them granted their informed written consent before participating in the study. No identifying information was recorded within the questionnaire responses collected.
Results
The study sample was composed of 336 participants, with a mean age of 38.56 years (SD = 9.47) and a mean time of professional performance in the PC field of 6.6 years (SD = 5.6). Table 1 describes participants’ demographic characteristics.
Table 1. Participants’ socio-demographic and professional characterization (n = 336)

a f = absolute and percentage frequency.
b Chaplain, beautician, music therapist, nursing technician.
Pilot test — cultural adaptation
Following the pilot test stage, the wording of seven items were adapted to enhance clarity within the Brazilian cultural context (items 2 and 3 of the “Physical Care” subscale, item 4 of the “Supportive Interpersonal Relationships” subscale, items 1, 5 and 6 of the “Self-Compassion and Purpose” subscale, and the first question of the general items).
At the same time, some additional pilot suggestions were not adopted as such changes would likely alter the meaning of the item in relation to what was in the original scale, including conceptual aspects related to mindfulness. For instance, in the subscale “Awareness”, one of the pilot test participants suggested that in item 1 (“I was aware of my thoughts”) thoughts should be classified as good or bad. However, the item proposes being aware of thoughts, regardless of whether they are good, bad, or of any other nature. Another instance concerned item 3 of the same subscale (“I was aware of my body”). In this case, the suggestion was about including in the item whether respondents should think about their body's limitations or strengths. However, originally, the item proposes body awareness, not body judgement regarding its limitations and strengths. Therefore, these suggested changes were not adopted.
Psychometric properties
Validity evidence based on the internal structure and reliability of the Brazilian-Portuguese version of the MSCS (33-item)
The six-factor model was specified as detailed in a previous study using the MSCS (33-item) (Cook-Cottone and Guyker, Reference Cook-Cottone2018): Factor 1. Physical Care (items 01 to 08); Factor 2. Supportive Relationships (items 09 to 13); Factor 3. Mindful Awareness (items 14 to 17); Factor 4. Self-Compassion and Purpose (items 18 to 23); Factor 5. Mindful Relaxation (items 24 to 29); and Factor 6. Supportive Structure (items 30 to 33). Following the analysis, all items presented saturation higher than 0.30 in their respective factors, with estimated factor loadings at p < 0.01 level. The tested factor model presented acceptable fit indices (CFI = 0.93; TLI = 0.92; RMSEA = 0.08 [CI: 90% = 0.07 to 0.08]). The estimated factor loadings for this model are presented in Table 2.
Table 2. Estimated factor loadings across the six MSCS factors (N = 336)
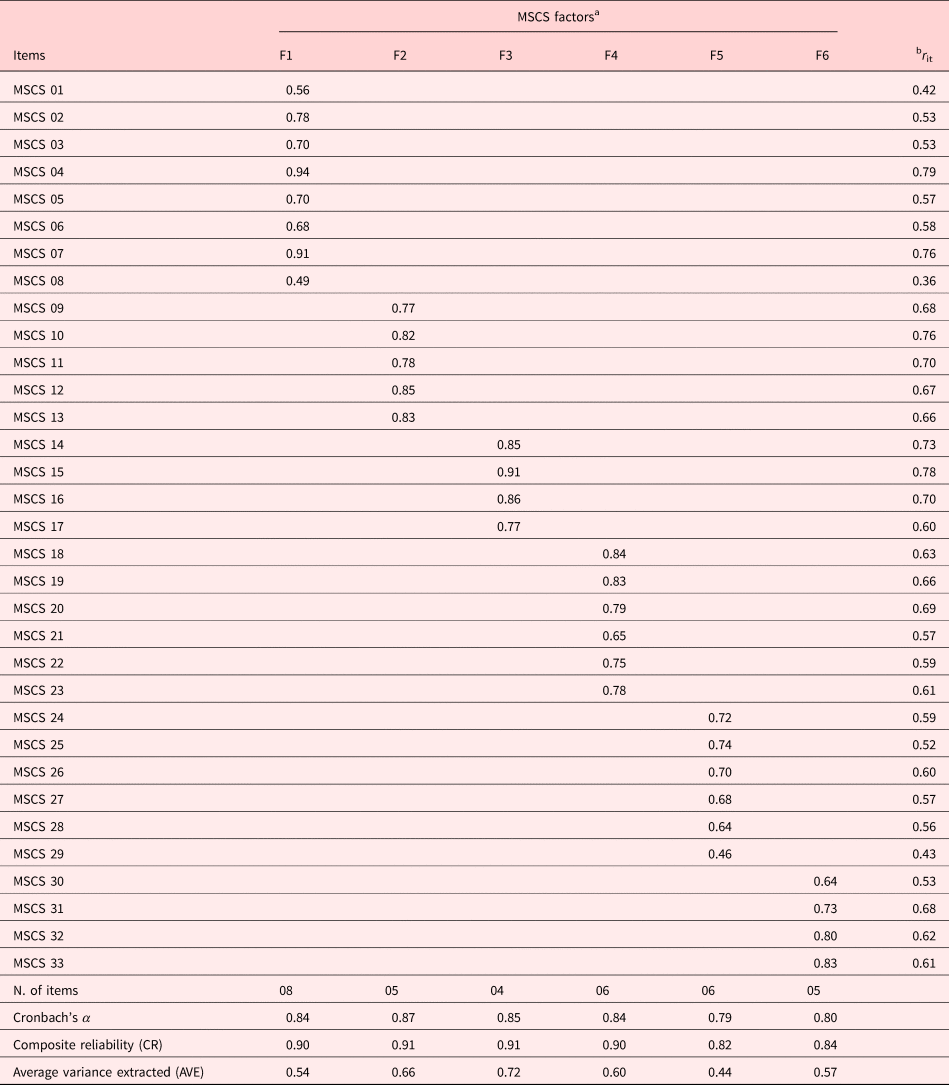
a Key: F1 = Physical Care; F2 = Supportive Relationships; F3 = Mindful Awareness; F4 = Self-Compassion and Purpose; F5 = Mindful Relaxation e F6 = Supportive Structure.
b Item-total correlation.
All reliability coefficients (CR and α) estimated for the six factors scored values above 0.70, indicating satisfactory internal consistency. The Average Variance Extracted (AVE) indices higher than 0.50 ratified the adequacy of the endogenous indicators (items) for the representation of the latent factors. The correlation between the latent factors is presented in Table 3.
Table 3. GEOMIN correlation between latent factors (N = 336)

Note: values in italic displayed diagonally represent the square root of the Average Variance Extracted.
Key: F1 = Physical Care; F2 = Supportive Relationships; F3 = Mindful Awareness; F4 = Self-Compassion and Purpose; F5 = Mindful Relaxation e F6 = Supportive Structure.
** p ≤ 0.01.
All correlation coefficients between the Brazilian-Portuguese version of the MSCS (33-item) latent factors were significant at the level of p ≤ 0.01. The Brazilian-Portuguese version of the MSCS (33-item) factors relates to each other positively, with moderate to strong magnitudes. This means that the dimensions of mindful self-care assessed by the instrument are closely related to each other and are directly proportional. The coefficients presented diagonally and italicized in Table 3 were higher than the estimated correlations between the factors, indicating that all dimensions assessed by the Brazilian-Portuguese version of the MSCS (33-item) discriminated adequately in the estimated structural model.
Validity evidence based on associations between Brazilian-Portuguese version of the MSCS (33-item) and external variables
The factor scores were calculated by using the arithmetic mean of the responses to the items that compose all six factors of the scale. These scores were used in correlation analyses with the BRS and SCS-SF scales, with all negative subscale items from the SCS-SF reverse scored prior to calculating a mean. All correlation results are summarized in Table 4. The strongest correlation (r = 0.55**) was found between Self-Kindness (SCS-SF) and Self-Compassion and Purpose (MSCS 33-item); this is noteworthy, given their conceptual similarities.
Table 4. Correlation between Brazilian-Portuguese version of the MSCS, resilience, and self-compassion (N = 336)

Key: F1 = Physical Care; F2 = Supportive Relationships; F3 = Mindful Awareness; F4 = Self-Compassion and Purpose; F5 = Mindful Relaxation; and F6 = Supportive Structure.
** p ≤ 0.01.
All estimated correlation coefficients between mindful self-care practices (Brazilian-Portuguese version of the MSCS — 33-item), self-compassion, and resilience were significant (p ≤ 0.01), with all of them being positive and ranging in magnitude from weak to moderate; the higher the mean scores of mindful self-care practices assessed by Brazilian-Portuguese version of the MSCS (33-item), the higher the scores of self-compassion and resilience.
Discussion
This study aimed to translate, culturally adapt, and validate the MSCS (33-item) in a sample of Brazilian palliative care providers. The results provide evidence that this Brazilian-Portuguese version of the MSCS (33-item) is a reliable and valid measure of the nature and frequency of mindfulness and self-care efforts.
The development of the MSCS (33-item) emerged from the need to assess mindful self-care in daily life, as well as to assess planned mindfulness meditation or other mind-body well-being practices (Cook-Cotton and Guyker, Reference Cook-Cottone2018). Professional quality of life and compassionate care are related to the well-being of care providers: when they care for themselves, this is not only supportive of compassionate care but also healthier and happier care providers (Galiana et al., Reference Galiana, Sansó and Muñoz-Martínez2021).
The factor model tested for the MSCS (33-item) was considered acceptable, adequately replicating the six-factor structure of the MSCS (33-item), with factor model fit indices similar to those observed in the original validation of this scale in a comparable healthcare context (Hotchkiss and Cook-Cottone, Reference Hotchkiss and Cook-Cottone2019). The reliability/internal consistency coefficients obtained for the six factors were satisfactory (α = 0.79 to 0.87; CR = 0.84 to 0.91) and comparable to those obtained in the development and validation study by Cook-Cottone and Guyker (Reference Cook-Cottone2018).
The Brazilian-Portuguese version of the MSCS (33-item) factors relates to each other positively, with moderate to strong magnitudes, indicating that the dimensions of mindful self-care assessed by the Brazilian-Portuguese version of the MSCS (33-item) are closely related to each other and are directly proportional. The factors “Physical Care” and “Self-Compassion and Purpose” address the emotional and cognitive aspects of the self. The factors “Supportive Relationships” and “Supportive Structure”, on the other hand, refer to practices aligned with the external experience of the self, providing a framework for choosing and maintaining positive relationships, creating a supportive environment, and balancing external demands. Finally, “Mindful Awareness” and “Mindful Relaxation” are centering practices that evaluate internal and external experiences in an integrative, attuned, and self-regulatory manner (Cook-Cottone and Guyker, Reference Cook-Cottone2018).
In this study, all correlation coefficients estimated between the levels of mindful self-care (Brazilian-Portuguese version of the MSCS — 33-item), self-compassion, and resilience of palliative care providers were significant and positive. That is, the higher the level of mindful self-care assessed by the Brazilian-Portuguese version of the MSCS (33-item), the higher the self-compassion and resilience scores of the participants. These results can be considered as sources of validity evidence based on external criteria (related constructs) for use and interpretation of the Brazilian-Portuguese version of the MSCS (33-item) scores in Brazil.
Self-compassion represents a personal and supportive resource for self-care, ensuring that needs are not overlooked, especially in times of distress (Garcia et al., Reference Garcia, Domingues Silva and Oliveira da Silva2021). Self-compassion also includes acceptance of failure and challenges, the ability to engage in a comforting and supportive internal conversation, permission to feel feelings, and recognition that failure and challenges are part of the human experience (Cook-Cottone and Guyker, Reference Cook-Cottone2018). However, self-compassion may not come naturally for some, and in many cases, it may need to be learned through practice (Mills et al., Reference Mills, Wand and Fraser2018b).
Self-compassion appears an important resource in the palliative care setting, considering it can support the practice of self-care and alleviate suffering by improving the social, psychosocial, and spiritual well-being of patients and healthcare providers (Garcia et al., Reference Garcia, Domingues Silva and Oliveira da Silva2021). In a study that examined the relationship between self-care and self-compassion among palliative care providers, self-compassion and self-care were positively correlated, with increased self-care ability being associated with increased self-compassion (Mills et al., Reference Mills, Wand and Fraser2018a), as observed in the present study.
Resilience is a construct that reflects the personal qualities that allow individuals to adapt and grow in the face of adversity (Connor and Davidson, Reference Coelho, Cavalcanti and Rezende2003). In professional settings, resilience occurs when personal resources are able to withstand stress and meet work demands (Back et al., Reference Back, Steinhauser and Kamal2016). Self-care practice is an important individual approach for promoting well-being and resilience among palliative care providers (Beng et al., Reference Beng, Chin and Guan2015; Sansó et al., Reference Sansó, Galiana and Oliver2015). This is corroborated by the correlations found in the present study (Table 4) between self-care and resilience, especially in relation to Mindful Awareness and Self-Compassion and Purpose (factors 3 and 4 of the Brazilian-Portuguese version of the MSCS — 33-item). Palliative care providers’ well-being and resilience depend largely on self-care and staff support; however, although the importance of self-care may appear evident — to date its role and impact on well-being and resilience among palliative care providers remain under-researched (Mills et al., Reference Mills, Ramachenderan and Chapman2020).
There are some limitations to this study, including the use of convenience sampling and potential influence of social desirability in participants. The relatively low number of social workers, dentists, pharmacists, speech therapists, nutritionists, and occupational therapists in our study could also be considered a limitation. However, it may merely represent an indication of the low proportion of people working in these disciplines in Brazilian palliative care. The higher numbers of medical and nursing practitioners in the present study are consistent with those in similar studies of palliative care providers internationally (Sansó et al., Reference Sansó, Galiana and Oliver2015; Mills et al., Reference Mills, Wand and Fraser2018a). While a larger sample size may have been helpful, the sample size achieved exceeded the guidelines threshold that was followed. Notwithstanding these limitations, the strengths of this study.
In conclusion, findings from this study suggest the Brazilian-Portuguese version of the MSCS (33-item) is a valid, reliable, and culturally appropriate instrument to examine the practice of mindful self-care by palliative care providers in Brazil. More broadly, it represents a promising instrument for future research into self-care practices and well-being among Brazilian healthcare providers. Longitudinal studies are recommended to better understand the effects of self-care on resilience and various aspects of well-being among healthcare providers regardless of clinical specialty, as well as to evaluate the temporal stability of responses to the Brazilian-Portuguese version of the MSCS (33-item) among other populations in Brazil.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951521001802.







