Introduction
In the past decades, the understanding of pregnancy and neonatal losses in the lives of parents and families has increased considerably. Until the 1970s, the death of an unborn child or a neonatal death was considered a mischance and judged unimportant (Lewis, Reference Lewis1976; Lewis and Page, Reference Lewis and Page1978). Perinatal grief was not understood. A rather common practice was to encourage parents to become pregnant again quickly to forget the loss (LaRoche et al., Reference LaRoche, Lalinec-Michaud and Engelsmann1982). Kennel et al. (Reference Kennel, Slyter and Klaus1970), pediatricians, were pioneers in the 1970s in studying the reactions of parents after the loss of a newborn. They created what they called “a mourning score,” based on their studies of mother-baby attachment, showing that a clear and identifiable process of grieving was present in women who had lost a newborn baby (Kennel et al., Reference Kennel, Slyter and Klaus1970). Their work changed the understanding and acceptance of parents’ grieving processes after perinatal loss. Kersting and Wagner (Reference Kersting and Wagner2012) also found that despite the short life of the child and the little time to build a relationship, grief intensity did not differ significantly from other losses.
Grieving, the process of accepting a loss and readapting to the new reality, involves intense suffering (Bonanno and Kaltman, Reference Bonanno and Kaltman2001). Reactions such as sadness, depressed mood, irritability, preoccupation, anxiety, and changes in eating and in sleeping patterns are seen as part of the process. Disbelief, guilt, numbness, social isolation, and anger are expected. The intensity tends to subside with time (Bonanno and Kaltman, Reference Bonanno and Kaltman2001; Shear, Reference Shear2012). When these reactions are too intense, persistent, distressing, and incapacitating, they can signal a serious health concern. Some authors refer to it as pathological grief (Gentile, Reference Gentile2004), others (Prigerson et al., Reference Prigerson, Horowitz and Jacobs2009) use prolonged grief disorder and others prefer the term “complicated grief” (Shear, Reference Shear2012). Throughout this article we will be using the term complicated grief according to Shear (Reference Shear2012): a chronic impairing form of grief that delays the healing process by changing its course for the worst. The pain and suffering do not subside over time, the loss is not accepted or integrated into the reality of ongoing life, and no joy or satisfaction with life can be expected in the future.
In perinatal death, defined as a loss from any gestational age or in the neonatal period, the grieving process involves extra losses. According to Côté-Arsenault and Denney-Koelsch (Reference Côté-Arsenault and Denney-Koelsch2011, Reference Côté-Arsenault and Denney-Loelsch2016), besides the deep sense of loss for a wished-for child there is also the feeling of losing the own sense of self, the role as a parent, potentially the loss related to one's sense of being a biological woman, and a sense of safety in the world. Recovering from perinatal loss has been reported to take very long, sometimes as long as 5–18 years (Gravensteen et al., Reference Gravensteen, Helgadottir and Jacobsen2012). Cacciatore (Reference Cacciatore2013) suggests that grieving after perinatal loss can have long-term effects on parents who live through the experience. Some parents may experience bereavement-related mental health problems such as depression, anxiety, suicidal ideation and post-traumatic stress disorder, among others. Studies have revealed that the loss of an unborn child after the diagnosis of a fetal malformation or severe chromosomal disorders during pregnancy can be considered a traumatic life event with high psychological impact (Kersting and Wagner, Reference Kersting and Wagner2012).
Since the Kennel et al. (Reference Kennel, Slyter and Klaus1970) pioneer publication, the literature on the grieving process after perinatal loss has flourished. Many instruments to quantitatively measure the presence and intensity of perinatal grief were developed to help health professionals to detect parents in need of further clinical and psychological support earlier on into their bereavement process preventing further damage (Bennett et al., Reference Bennett, Ehrenreich-May and Litz2012). In the early 2000s, perinatal palliative care (PPC) emerged with the goal of providing integrated follow-up after prenatal diagnosis of life-limiting conditions continuing through pregnancy, birth and loss (Denney-Koelsch et al., Reference Denney-Koelsch, Perry Black and Côté-Arsenault2016). PPC programs should include screening of families to identify those more vulnerable to complicated grief and its consequences in order to offer more opportunities for follow-up. This model of using an instrument to evaluate grief after any perinatal loss could be spread to every service who deals with families living through this experience.
Learning about these instruments and their clinical and research applications can help clarify and disseminate to clinicians dealing with such families the knowledge about the nature of grief following perinatal loss, the incidence of complicated grief, the role of cultural beliefs, religious, social support, and other factors.
Thus, this review examined the literature on perinatal loss searching for studies that used instruments specifically built to measure grief reactions after perinatal loss. The aim is to determine which instruments are available and to verify whether there is a consensus in the literature regarding factors that potentially moderate grief intensity and duration. We also intend to learn whether grief scores measured by such scales are used to evaluate interventions designed to better assist families in the bereavement process.
Methods
A search strategy for this systematic review was formulated based on the study objectives and inclusion criteria registered as a review protocol in the International Prospective Register of systematic review (PROSPERO) number CRD42018092555 (Setubal et al., Reference Setubal, Bolbio and Francisco2018). A PUBMED, Cochrane, and PsycINFO electronic search was conducted using the keywords “perinatal” AND (“grief” OR “bereavement” OR “mourning”) AND (“scale” OR “questionnaire” OR “measure” OR “assessment”) up to May 2018. Eligibility criteria included articles in English, which used standardized measures to assess perinatal grief after any kind of perinatal loss: from early pregnancy loss such as miscarriages and abortions, to stillbirths, neonatal death, and pregnancy termination due to fetal malformation. Articles reporting translation and validation of any perinatal grief instrument to other languages were included. Articles written in languages other than English or measuring health care providers perceptions of grief were excluded. Two reviewers independently extracted data on: specific instruments evaluating perinatal grief; other instruments assessing different variables related to grief such as depression and anxiety inventories or questionnaires, authors, year, journal, and country of publication; study design; kinds of losses; sample size and factors associated with grief reactions. Both reviewers revised the search independently to eliminate duplicates. Discrepancies between coders in what articles were eligible were re-examined and discussed reaching consensus to determine which ones to include.
Results
A total of 141 articles described specific instruments to evaluate perinatal grief. Of these, we excluded 74: articles written in another language rather than English; the ones examining grief reactions after the loss of an older child; articles using a more general grief instrument which was not specifically built to measure perinatal grief were not included; articles evaluating parents’ perception of care; and the ones evaluating health care team perceptions. Sixty-seven articles met the inclusion criteria. Figure 1 shows a PRISMA flowchart (Moher et al., Reference Moher, Liberati and Tetzlaff2009) of selected articles, the included scales and the omitted articles stating the reasons for exclusion. Supplementary Table S1 shows all included articles.

Fig. 1. PRISMA flowchart showing the search method, inclusion and exclusion criteria.
Types of perinatal grief instruments found in the search
Seven different instruments published between 1984 and 2002 were found in this review and are described below according to their publication date.
1) Mourning Scale: One article found in the review used this scale. La Roche et al. (Reference LaRoche, Lalinec-Michaud and Engelsmann1984) created this scale as an objective clinical evaluation to identify grief reactions to perinatal death. Although the scale was built to measure grief, it was called “Mourning Scale.” The authors stated that “…grief reactions are measurable and it is possible to distinguish the degree and quality of mourning….” The scale evaluated a group of 30 women and 7 men 1 and 2 years after the loss. All women had received crisis intervention immediately after the loss and had a follow-up contact at three weeks and at 3 months. The Mourning scale was based on the six items of the original instrument by Kennel et al. (Reference Kennel, Slyter and Klaus1970), adding two new variables to it to yield a cumulative mourning score. The items comprised of sadness, loss of appetite, inability to sleep, increase in irritability, preoccupation with lost infant, inability to return to normal activities, lack of expected affect, guilt feelings, and each one of them was scored on a scale from 0 to 4 yielding a score ranging from 0 to 32. An item score of 4 indicated the highest severity and duration of a problem for more than 1 month
2) Perinatal Grief Scale (PGS): There were 53 articles using the short PGS version by Potvin et al., Reference Potvin, Lasker and Toedter1989. The original scale by Toedter et al. (Reference Toedter, Lasker and Alhadeff1988) consisted of 104 Likert-type items whose answers vary from 1 (strongly agree) to 5 (strongly disagree). The short version of the PGS (Potvin et al., Reference Potvin, Lasker and Toedter1989) created just 1 year after the first one by the same team consists of 33 items and was found to be essentially equivalent to the long version. The PGS measures a wide range of reactions to perinatal loss, including depression, anger, social functioning, spirituality, desire for counseling, loss of control, and guilt. It includes three subscales (Active Grief, Difficult Coping, and Despair) with 11 items, each varying from 11 to 55 points, and is considered a reliable and well-validated measure of grief in the perinatal setting, including underestimated grief related to early loss. The three subscales were built upon extensive research using factor analysis and carefully checked for reliability and internal consistency and are considered relevant and robust (Potvin et al., Reference Potvin, Lasker and Toedter1989). The subscale “Active Grief,” or the normal grief reactions that may follow pregnancy loss, includes items regarding sadness, missing the baby, and crying for the baby. A score of 34 or more is considered high. “Difficulty Coping” includes items suggesting difficulty in dealing with normal activities and with other people, indicating withdrawal and depression. High scores in this subscale are 30 or more. “Despair” represents feelings of worthlessness and hopelessness, and a score over 27 points is considered high. Total score varied from 33 to 165, and a score over 91 is considered worrisome, indicating a higher probability of greater vulnerability to the loss. The subscales “Difficulty Coping” and “Despair” represent increasingly severe forms of grieving, and high scores on these two subscales are considered predictors of complicated grief.
3) Perinatal Bereavement Scale (PBS): Two articles found in this review used the PBS scale. In the first one, Theut et al. (Reference Theut, Pedersen and Zaslow1989) described the 26-item instrument developed and designed especially for the study to measure couples’ bereavement reactions during a subsequent pregnancy after a perinatal loss (including miscarriage, stillbirth, or neonatal death) that had occurred within the previous 2 years. Couples, separately, completed the PBS twice: once, while in the eighth pregnancy month and the second time, six weeks after the birth of that other child. PBS required approximately 15 min to be completed. Responses were scored on a 4-point Likert-type scale ranging from “almost never” to “almost all the time.” Items such as “I daydream about my lost child,” “I still feel sad about my pregnancy loss,” or “I have resources to help cope with my loss” appear in both positive and negative directions to minimize responses sets. The focus is on the thoughts and feelings of the parents, including sadness, guilt, anger, and preoccupation with the loss. The scale showed good internal consistency. In a follow-up study by the same group (Theut et al., Reference Theut, Zaslow and Rabinovich1990), the authors evaluated this same group of parents 16 months after the birth of the subsequent child using the PBS. They compared the group which had a previous early loss with the previous late loss group. Mothers from the late loss group had significantly higher PBS scores than either the early group mothers or fathers from both groups, early or late loss.
4) Munich Grief Scale (MGS): Beutel et al. (Reference Beutel, Willner and Volkl1995) developed a questionnaire by modifying and shortening the PGS to distinguish depressive symptoms from grief after miscarriage. MGS 22 items were rated on a 5-point scale from “not true” to “completely true” divided in five parts: (1) sadness (six items: measured sad, painful feelings, and recollections and the need to talk about the loss of and crying and yearning for the dead child); (2) fear of future (five items: assessed fear of future miscarriage or of not being able to have children at all); (3) guilt (five items: measured guilt feeling, consisting of self-blame for not having done enough to avoid the miscarriage and a sense of personal failure); (4) anger (three items: measured irritability toward others); and (5) search for meaning (three items: seeking consolation and support from others). Higher scores indicate more severe grief. The MGS was developed in Germany and is not extensively used in English speaking countries. Only three articles were found in English: The original article by Beutel et al. (Reference Beutel, Willner and Volkl1995) showing the construction and validation of the MGS. One evaluating individual attachment styles, social support and quality of current relationship in relation to grief reactions after perinatal loss (Sheidt et al., Reference Scheidt, Hasenburg and Kunze2012), another is a review on scales used to measure grief after miscarriage (Brier, Reference Brier2008).
5) Perinatal Grief Intensity Scale (PGIS): In this review, we found five articles that used the PGIS. This scale was developed by Hutti et al. (Reference Hutti, DePacheco and Smith1998) to measure grief intensity after miscarriages. According to the authors, the way people perceive this event, rather than the miscarriage itself, influences the intensity of behaviors and actions. The PGIS has 36 Likert-type items, ranging from strongly agree (4 points) to strongly disagree (1 point). The items are distributed in three factors thought to be measuring different facets of grieving and influencing its intensity: (1) “Reality,” which included six items capturing the feelings of mothers regarding the perceived reality of the pregnancy and the baby; (2) “Confront Others” included four items about the mother's ability to make decisions or act in ways that would help the experience to be as she would have desired. It encompassed her ability to assert her needs to others; and (3) “Congruence” included four items and related to satisfaction with the way the experience of miscarriage unfolded, given that the mother had to go through it. The first article is about the scale validation (Hutti et al., Reference Hutti, DePacheco and Smith1998). Two more recent articles by the same authors (Hutti et al., Reference Hutti, Armstrong and Myers2013, Reference Hutti, Armstrong and Myers2015) evaluated the dimensionality of PGIS not only in immediate subsequent pregnancy after a miscarriage but also in stillbirth or neonatal death. The fourth article by the same group (Hutti et al., Reference Hutti, Myers and Hall2017) compared PGIS with anxiety and depression inventories. The fifth article (Hutti et al., Reference Hutti, Myers and Hall2018) measured the validity of the PGIS via its ability to predict future intense grief based on a PGIS score obtained early after a perinatal loss. The authors compared PGIS’ validity and reliability with the PGS and concluded that the PGIS is comparable to the PGS, has a lower response burden, and can reliably and validly predict, one to eight weeks after the loss, women who may experience future complicated grief associated with perinatal loss.
6) Perinatal Bereavement Grief Scale (PBGS): Two articles in this review used the PBGS: the original one which describes the scale and its validation (Ritsher and Neugebauer, Reference Ritsher and Neugebauer2002) and a second one by Koch et al. (Reference Koch, Santos and Santos2012), which compared the PBGS with the Well-Being Questionnaire (WBQ-12) in the process to validate the WBQ-12. Developed by Ritsher and Neugebauer (Reference Ritsher and Neugebauer2002), the PBGS is a 15-item scale designed as a measure of grief and yearning for the lost pregnancy and the lost baby derived from a review of the theoretical, clinical, counseling, and research literature. The authors suggested that the PBGS can facilitate research on epidemiology of yearning and on the relationships between yearning for the lost pregnancy and baby with other well-studied bereavement reactions such as shock and numbness, depression, and disorganization. Seven pregnancy items contain statements such as “you dreamed you were still pregnant,” “you patted or held your belly as though you were still pregnant,” “you wanted to hold the baby in your arms,” and “you imagined what the baby would have looked like.” The remaining item asks whether “you felt physically ill when you thought about the miscarriage.” Respondents indicate how often the statement has been true in the past week, using a 4-point Likert-type scale ranging from 1 (rarely or none of the time, less than one day) to 4 (most or all the time, five to seven days). Responses were added to a total score (possible range, 15–60). One item: “you found it easy to think about things other than the baby” was reversed scored.
7) Attachment in Perinatal Bereavement Scale (APBS): One article using the APBS was found. The scale was created by Uren and Wastell (Reference Uren and Wastell2002) based on the perinatal bereavement literature, looking for aspects of the phenomenological experience of perinatal death, comparing its results with attachment and trauma scales as well as with the PGS, used in this study as an outcome variable. This 20-item scale selected aspects of the phenomenological experience of perinatal death. Participants were asked to indicate the degree to which various feelings or experiences had been true for them at any time during their grief process. Ratings ranged from (1) not at all to (5) extremely. The APBS comprises four subscales, each with five items, measuring the phenomena of numbness, disorientation, yearning, and despair. A 5-item scale measured the extent to which participants experience a continuing relationship with their baby, ranging from (1) very uncharacteristic of me to (5) very characteristic of me.
Included studies
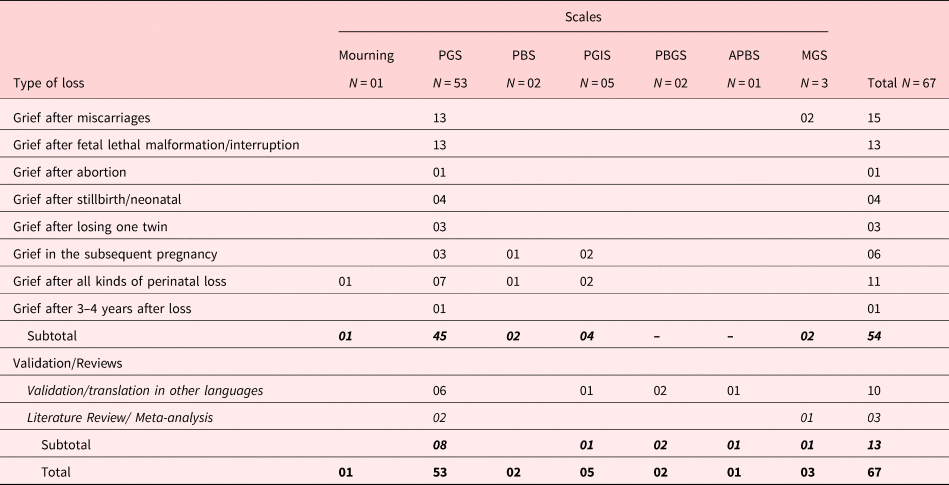
Table 1 shows the distribution of the 67 included articles according to the instruments used to measure grief, the type of loss, validation, or translation of the scale or previous literature review.
Table 1. Types of scales and number of articles distributed by themes
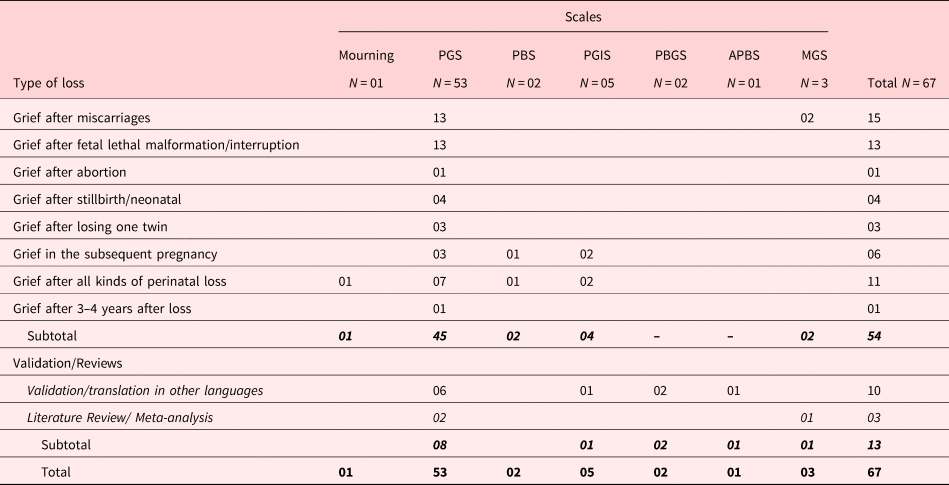
Types of perinatal loss
The perinatal losses evaluated by each instrument range from early miscarriages, abortions, interruptions, late pregnancy loss to early neonatal loss. Fifty-three articles described the kind of perinatal loss being measured (abortion, miscarriage, fetal death, postnatal loss, termination due to malformation, twin loss, subsequent pregnancy, or all losses). The PGS was used in 45 of these articles. Most of them are about lethal fetal malformation/interruption (N = 13) and miscarriages (N = 13). Two articles measured grief after miscarriage using MGS. Seven of the articles used the PGS to measure grief in all kinds of perinatal loss as the one article using the Mourning scale, one using the PBS, and two using the PGIS. To evaluate grief in subsequent pregnancies, three articles used the PGS, two used the PGIS, and another used the PBS. One recent article measured grief 3–4 years after perinatal loss (Van Veen-Doornenbal et al., Reference Van Veen-Doornenbal, Derks and Van Leeuwen2017).
Translations or validations
All six articles found in the review describing translations to other languages and cultures used the PGS: one to Swedish (Adolfsson and Larsson, Reference Adolfsson and Larsson2006); two to Chinese (Yan et al., Reference Yan, Tang and Chung2010; Lai et al., Reference Lai, Chung and Lee2013); one to Greek (Maniatelli et al., Reference Maniatelli, Zervas and Halvatsiotis2018); one to Spanish (Capitulo et al., Reference Capitulo, Cornelio and Lenz2001); and one to Dutch (Hunfeld et al., Reference Hunfeld, Wladimiroff and Passchier1993). Six articles described validations: one regarding the PGS (Toedter et al., Reference Toedter, Lasker and Alhadeff1988), another the PGIS (Hutti et al., Reference Hutti, DePacheco and Smith1998), one the MGS (Beutel et al., Reference Beutel, Willner and Volkl1995), two others the PBGS (Ritsher and Neugebauer, Reference Ritsher and Neugebauer2002; Koch et al., Reference Koch, Santos and Santos2012), and one the APBS (Uren and Wastell, Reference Uren and Wastell2002).
Previous literature review
Three articles were earlier reviews on the use of the PGS to measure grief after perinatal loss (Toedter et al., Reference Toedter, Lasker and Jansen2001; Brier, Reference Brier2008; Adolfsson, Reference Adolfsson2011).
Factors associated with perinatal grief reactions
Thirty-nine articles using PGS scores, examined factors associated with perinatal grief reactions. Grief generally refers to the general score obtained in the scale. General scores over 91 are considered worrisome, indicating a higher probability of greater vulnerability to developing mental health problems. High scores in the subscales “Difficulty Coping” and “Despair” represent increasingly severe forms of grieving and are considered predictors of complicated grief.
All kinds of factors were studied and they varied according to each study. For didactic reasons, we grouped the factors in four categories: (1) social-demographics; (2) support; (3) reproductive history; and (4) mental health status. Supplementary Table S2 presents every article according to the kinds of losses studied.
Social-demographic factors
The social-demographic factors examined in these studies comprised of age, parent's gender, ethnicity, socio-economic status, education, employment, and income. In most of them (Toedter et al., Reference Toedter, Lasker and Alhadeff1988; Conway and Russell, Reference Conway and Russell2000; Serrano and Lima, Reference Serrano and Lima2006; Adolfsson and Larsson, Reference Adolfsson and Larsson2010; Cowchock et al., Reference Cowchock, Ellestad and Meador2011; Ridaura et al., Reference Ridaura, Penelo and Raich2017), age was not associated with high scores on the PGS. In three of them, however (Lin and Lasker, Reference Lin and Lasker1996; Zeanah et al., Reference Zeanah, Dailey and Rosenblatt1993; Curley and Johnston, Reference Curley and Johnston2013), younger women, when compared to older ones, showed significantly higher grief scores. On the other hand, Jansen et al. (Reference Jansen, Cuisinier and de Graauw1997) found the opposite, while for Van (Reference Van2010), older age found to be protective against high grief scores. As for gender, some studies found no differences between men's and women's grief (Harrigan et al., Reference Harrigan, Naber and Jensen1993; Johnson and Puddifoot, Reference Johnson and Puddifoot1996; Hunfeld et al., Reference Hunfeld, Mourik and Passchier1996; Lin and Lasker, Reference Lin and Lasker1996, Puddifoot and Johnson, Reference Puddifoot and Johnson1998 and Reference Puddifoot and Johnson1999) Swanson et al. (Reference Swanson, Kane and Pearsall-Jones2009) looked at gender differences in coping strategies after loss and found that women scored higher on the scale immediately after loss compared to men, similarly to other three studies (Cuisiner et al., Reference Cuisiner, Kiupers and Hoogdiun1993; Serrano and Lima, Reference Serrano and Lima2006; Barr, Reference Barr2012). Ethnicity (Kulathilaka et al., Reference Kulathilaka, Hanwella and de Silva2016) was not associated with grief scores. Most studies reported no association between socio-economic status or income and grief scores (Toedter et al., Reference Toedter, Lasker and Alhadeff1988, Lasker and Toedter, Reference Lasker and Toedter1991; Johnson and Puddifoot, Reference Johnson and Puddifoot1996; Barr, Reference Barr2012; Purandare et al., Reference Purandare, Ryan and Ciprike2012; Kulathilaka et al., Reference Kulathilaka, Hanwella and de Silva2016, Druguet et al., Reference Druguet, Nuño and Rodó2018). Nevertheless, two studies (Al-Maharma et al., Reference Al-Maharma, Abujaradeh and Mahmoud2016; Paris et al., Reference Paris, Montigni and Pelloso2016) found that less educated women or unemployed had significantly higher grief scores than did women with high income.
Support
Marital, social, professional, and religious support were examined in some studies. Marital support and marital satisfaction were associated with lower grief scores (Toedter et al., Reference Toedter, Lasker and Alhadeff1988; Lasker and Toedter, Reference Lasker and Toedter1991; Jansen et al., Reference Jansen, Cuisinier and de Graauw1997; Kroth et al., Reference Kroth, Garcia and Hallgren2004; Purandaree et al., Reference Purandare, Ryan and Ciprike2012; Paris et al., Reference Paris, Montigni and Pelloso2016). Social support was found to be associated with lower grief scores (Lasker and Toedter, Reference Lasker and Toedter1991; Jansen et al., Reference Jansen, Cuisinier and de Graauw1997; Kroth et al., Reference Kroth, Garcia and Hallgren2004) or not (Zeanah et al., Reference Zeanah, Dailey and Rosenblatt1993; Lin and Lasker, Reference Lin and Lasker1996). Professional support groups (Kulathilaka et al., Reference Kulathilaka, Hanwella and de Silva2016; Paris et al., Reference Paris, Montigni and Pelloso2016) and religiosity were associated with lower grief scores (Lasker and Toedter, Reference Lasker and Toedter1991; Cowchock et al., Reference Cowchock, Lasker and Toedter2010, Reference Cowchock, Ellestad and Meador2011; Cope et al., Reference Cope, Garrett and Gregory2015; Kulathilaka et al., Reference Kulathilaka, Hanwella and de Silva2016; Paris et al., Reference Paris, Montigni and Pelloso2016).
Reproductive history
Many studies examined women's reproductive history such as gestational age at the loss, infertility history, planned pregnancy, anticipating the loss, previous losses, having other children trying to conceive after the loss, elapsed time since the loss, pregnancy termination, and subsequent pregnancies. Nine articles examined gestational age and five of them (Toedter et al., Reference Toedter, Lasker and Alhadeff1988; Zeanah et al., Reference Zeanah, Dailey and Rosenblatt1993; Hunfeld et al., Reference Hunfeld, Tempels and Passchier1999; Jansen et al., Reference Jansen, Cuisinier and de Graauw1997; Kulathilaka et al., Reference Kulathilaka, Hanwella and de Silva2016) found significantly higher grief scores when the loss occurred in more advanced pregnancies. On the other hand, three other articles (Cuisinier et al., Reference Cuisinier, Janssen and de Graauw1996; Serrano and Lima, Reference Serrano and Lima2006; Ridaura et al., Reference Ridaura, Penelo and Raich2017) found no association between gestational age and higher grief scores. History of infertility (Lasker and Toedter, Reference Lasker and Toedter1991), planned pregnancy (Lin and Lasker, Reference Lin and Lasker1996), anticipating the loss (Cuisinier et al., Reference Cuisinier, Janssen and de Graauw1996), or previous losses (Lasker and Toedter, Reference Lasker and Toedter1991; Cuisinier et al., Reference Cuisinier, Janssen and de Graauw1996; Lin and Lasker, Reference Lin and Lasker1996; Adolfsson et al., Reference Adolfsson, Berterö and Larsson2006; Druguet et al., Reference Druguet, Nuño and Rodó2018; Curley and Johnston, Reference Curley and Johnston2013; Ridaura et al., Reference Ridaura, Penelo and Raich2017) were not predictive of higher grief scores. Having a previous child was neither associated with high grief scores (Hunfeld et al., Reference Hunfeld, Tempels and Passchier1999; Johnson and Puddifoot, Reference Johnson and Puddifoot1996; Lin and Lasker, Reference Lin and Lasker1996; Van, Reference Van2010; Lafarge et al., Reference Lafarge, Mitchell and Fox2017; Druguet et al., Reference Druguet, Nuño and Rodó2018) nor considered predictive of low grief scores (Hunfeld et al., Reference Hunfeld, Wladimiroff and Passchier1994; Cuisinier et al., Reference Cuisinier, Janssen and de Graauw1996; Johnson and Puddifoot, Reference Johnson and Puddifoot1996; Purandare et al., Reference Purandare, Ryan and Ciprike2012; Kulathilaka et al., Reference Kulathilaka, Hanwella and de Silva2016). Only one article (Barr, Reference Barr2006) found that women who were trying to conceive or who had a living child prior to loss presented higher grief levels. One study from Jordan (Al-Maharma et al., Reference Al-Maharma, Abujaradeh and Mahmoud2016) found that women's reproductive history of not conceiving 1 year after the loss, conceiving to replace the loss child, having a subsequent female child and losing a male child were all associated with higher levels of grief. According to five studies, the more recent the loss, higher the grief (Harrigan et al., Reference Harrigan, Naber and Jensen1993; Conway and Russell, Reference Conway and Russell2000; Barr, Reference Barr2006, Reference Barr2012; Cowchock et al., Reference Cowchock, Ellestad and Meador2011; Cope et al., Reference Cope, Garrett and Gregory2015). On the other hand, Cowchock et al. (Reference Cowchock, Ellestad and Meador2011) found that time elapsed since the loss was not associated with higher grief scores. Alexandre et al. (Reference Alexandre, Votino and De Noose2016) looked at subsequent pregnancies and found that time since the loss was not associated with higher grief scores. Hunfeld et al. (Reference Hunfeld, Wladimiroff and Passchier1994) found that parent's perceived control by choosing pregnancy termination did not diminish grief levels and Davies et al (Reference Davies, Gledhill and McFadyen2005) as well as Cope et al. (Reference Cope, Garrett and Gregory2015) found that termination is associated with high levels of grief. Induction methods were found to not interfere with grief intensity (Burgoine et al., Reference Burgoine, Van Kirk and Romm2005).
Mental health status
Grouped under “Mental health status” were factors such as pre-loss mental health problems, including personality issues, attachment, and coping strategies, that if impairing or at the level of symptomatology, could put someone at more risk for having mental health issues in bereavement. Four articles (Toedter et al., Reference Toedter, Lasker and Alhadeff1988; Lasker and Toedter, Reference Lasker and Toedter1991; Toedter et al., Reference Toedter, Lasker and Jansen2001; Kulathilaka et al., Reference Kulathilaka, Hanwella and de Silva2016) found that pre-loss mental health issues were associated with higher grief scores and complicated grief reactions. Having a more neurotic personality (Hunfeld et al., Reference Hunfeld, Wladimiroff and Passchier1997; Jansen et al., Reference Jansen, Cuisinier and de Graauw1997) or being prone to more problematic social emotions such as shame and guilt (Barr and Cacciatore, Reference Barr and Cacciatore2008; Barr, Reference Barr2012) and having emotional expressiveness (Kroth et al., Reference Kroth, Garcia and Hallgren2004) are examples of prior mental health issues examined in these studies. Continued bond to the lost child was also found to be associated with higher grief scores (Cowchock et al., Reference Cowchock, Lasker and Toedter2010). On the other hand, being more satisfied with their role in life was associated positively with lower grief scores (Van, Reference Van2010) as well as being able to use adaptative coping strategies (Lafarge et al., Reference Lafarge, Mitchell and Fox2017).
Grief measurements before/after interventions
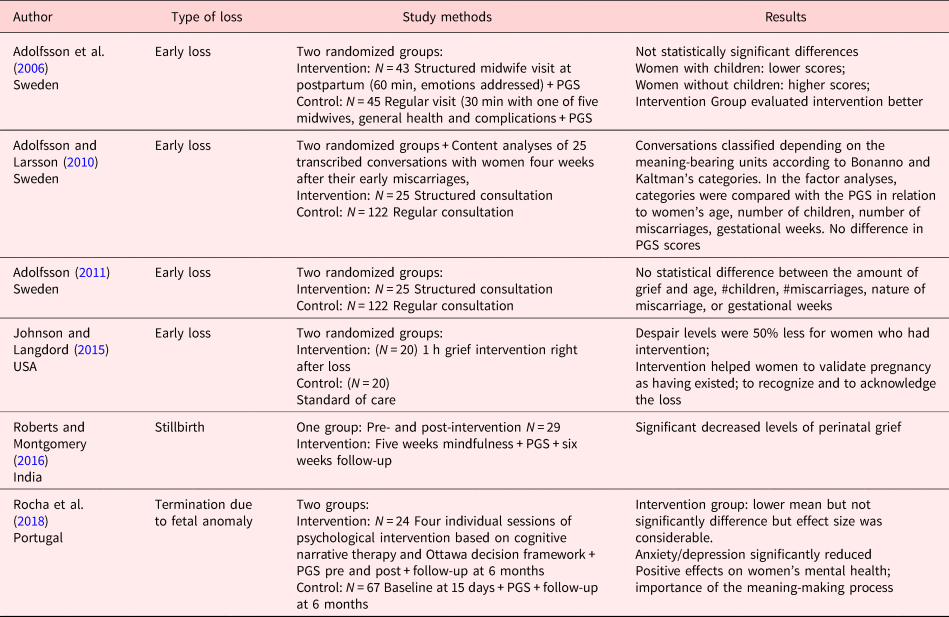
Six studies covered in this review used PGS scores to measure grief before and after interventions designed to help parents through the bereavement process after perinatal loss. Table 2 describes these studies according to the type of loss they looked at.
Table 2. Studies using the Perinatal Grief Scale to measure grief intensity after interventions designed to help women cope with grief after perinatal loss (N = 6)
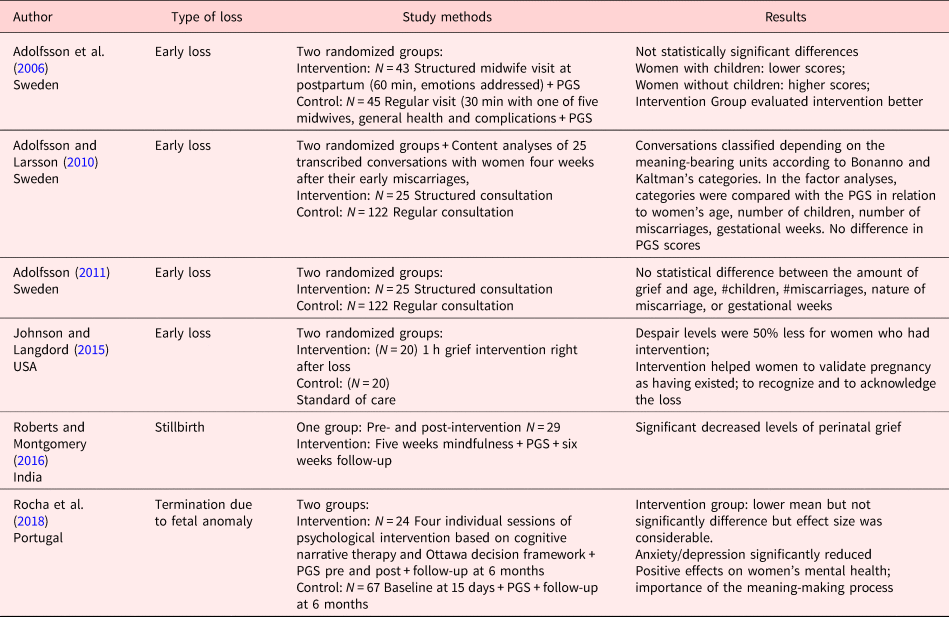
Grief after miscarriage
Four articles examined grief reactions after miscarriages. In three of them, the intervention consisted of a longer structured visit to a midwife trained to focused on woman's experience of her miscarriage, her feelings and emotions. When these women returned to a post-miscarriage follow-up, the midwives devoted extra time to address the loss (Adolfsson et al., Reference Adolfsson, Berterö and Larsson2006; Adolfsson and Larsson, Reference Adolfsson and Larsson2010; Adolfsson, Reference Adolfsson2011). The control group had only the shorter regular follow-up visit. The authors found no significant difference among the PGS scores in intervention groups and the controls but women in the intervention group estimated the importance of a follow-up visit after miscarriage significantly greater than in the controls.
The fourth study (Johnson and Langford, Reference Johnson and Langford2015) analyzed the impact of an immediate intervention after miscarriage. The intervention was conducted by the investigator and a trained research assistant at the emergency center at the time the miscarriage occurred. It included moving the patient to a private area, allowing time for questions, asking the woman if she wants to see the product of conception, assessing individual needs such as religious or emotional support, mailing sympathy card a week or two after the loss, following up with telephone call. The control group had the regular care, which did not include any of the above actions. All women filled the PGS during the two-week follow-up. They found no significant differences in the general PGS scores between groups although women who participated in the intervention had scores 50% lower in the subscale “Despair.”
Grief after stillbirth
A fifth article evaluated a five-week intervention, based on mindfulness exercises consisted of two group exercises (first and fifth session) in the health center and training at home in dyads and triads with a nurse. Between sessions, participants were encouraged to practice mindfulness exercises, keeping a simple daily log. The intervention was designed to help women in the grieving process after experiencing a third trimester stillborn. The authors compared women's PGS scores before and after the intervention and found no significant decline from first to second measurements. The study had no comparison group (Roberts and Montgomery, Reference Roberts and Montgomery2016).
Grief after pregnancy termination
A randomized controlled trial used a cognitive narrative intervention and measured its effect in preventing depression and anxiety symptoms after termination of pregnancy in comparison with a control group which had the usual treatment. The intervention group participated in four weekly sessions of 60 min each with a trained psychologist, beginning before the termination and ending 1 month after, comprising the following themes: decision, subjectivation, metaphorization, and projecting. The first session focused on decision-making by understanding the meaning of the problem, clarifying the values related to termination using the Ottawa Decision framework. The other three sessions explored the emotional/cognitive contents of the termination process, the sense of authorship and coherence, generating a metaphor that carried the best meaning, promoting a new organization. The intervention group had a lower mean in the PGS scores compared to the control group, but the difference was not significant, although the effect size was considerable. In general, the article showed positive effects on women's mental health, emphasizing the importance of meaning-making process in the context of terminating a wanted pregnancy.
Discussion
Worldwide, each year, the incidence of miscarriages is approximately 10–15% of all pregnancies (Campaña et al., Reference Campaña, Monica Rittler and Gili2017). About 2.6 million babies are stillborn and about the same number or neonates die annually (Farrales et al., Reference Farrales, Cacciatore and Jonas-Simpson2020). Congenital anomalies are responsible for an estimated 303,000 newborns deaths within four weeks of birth every year (WHO, 2016). Perinatal loss and grief-related symptoms affect too many people around the globe. According to Toedter et al. (Reference Toedter, Lasker and Alhadeff1988), one-third of all women are affected by a perinatal loss and of those 10% suffer from complicated grief. Kersting et al. (Reference Kersting, Kroker and Steinhard2007) found that 14% of women who interrupted pregnancy due to fetal malformation filled all criteria for complicated grief 14 months after the procedure. A large epidemiologic longitudinal study to measure the psychological impact on bereaved women after perinatal loss by Gold et al. (Reference Gold, Leon and Boggs2016) found high levels of distress and limited rates of treatment 9 months after the loss.
As grief after the loss of another loved person, perinatal loss needs support and time to heal (Lasker and Toedter, Reference Lasker and Toedter1991; Toedter et al., Reference Toedter, Lasker and Jansen2001). On the other hand, because of its specificities, it is quite different: it is related to the loss of a dreamed ideal loved one, to whom parents had an intense but brief time to know and interact, usually indirectly, through images or some brief contact after birth. Grief reactions to perinatal loss includes the loss for and the feeling of losing the own sense of self and the role as a parent, besides the ability to produce life (Côté-Arsenault and Denney-Koelsch, Reference Côté-Arsenault and Denney-Koelsch2011). These circumstances may complicate the grieving process (Kersting and Wagner, Reference Kersting and Wagner2012) and parents facing perinatal loss may develop more disruptive or long-lasting symptoms associated with complicated grief or other psychiatric illnesses such as depression. It is, therefore, important to distinguish complicated grief from other disorders as it is necessary to be able to distinguish normative grief after perinatal loss from complicated grief. So, when the measurement of a perinatal loss is done in terms of grief, by using a rating instrument specifically designed to measure perinatal grief, parents’ reactions due to the specificities of the bereavement process can be regarded as normal and transitory and not as depressive symptoms (Toedter et al., Reference Toedter, Lasker and Jansen2001). On the other hand, high grief scores could alert to possible severe reactions to the loss, which could progress to complicated grief. If not cared for, it could leave various psychological sequelae related to complicated grief such as “guilt, envy, bitterness, or anger that are relentlessly activated and excessively painful, without periods of respite from positive emotions” (Shear, Reference Shear2012). Or could even turn into other psychiatric illnesses such as depression or PTSD among others. Thus, it is relevant to evaluate grief after perinatal loss, from miscarriage to neonatal, as a preventive mental health measure.
The seven instruments found in the search are standardized measures of grief specific to pregnancy loss. Although they differ in terms of what types of grief manifestations they measured — some focused in behaviors, others in physical manifestations, or in affects such as anger or sadness; others looked into psychological issues such as yearning, or search for meaning — they captured some elements unique to perinatal loss. The Mourning scale includes preoccupation with lost infant; the PGS looks into loss of control, guilt among others. The PBS focus is on the thoughts and feelings of the parents, including depression, anger, social functioning, and spirituality. The MGS looked into feelings of missing the baby, painful memories of the loss, and difficulty relinquishing the hopes for, expectations of, and fantasies about the unborn child. The PGBS emphasizes the construct yearning for the lost pregnancy and the lost baby, while PGIS captures the way people perceive the event rather than the loss in itself. The APBS measures numbness, disorientation, yearning, despair, and the extent to which participants experience a continuing relationship with their baby.
Among these seven instruments, the PGS has been the most extensively used after any kind of loss, in different cultural settings all over the world, even 30 years after its publication (Toedter et al., Reference Toedter, Lasker and Jansen2001). It might be related to how easy and quick its application and analysis are as well as its validation to other languages and cultures confirming its value as a clinical and research measure. Its reliability in detecting high scores in each separate subsection, especially in the subscales “Difficult Coping” and “Despair,” as predictors of complicated grief, can alert health care providers to the need of follow-up. The other scales were restricted to few studies in English-speaking countries only.
Nevertheless, according to Brier (Reference Brier2008), “PGS has been criticized for both overemphasizing feelings related to the “lost baby” at the expense of other potential grief-related feelings, such as yearning for the lost pregnancy and to overlapping too greatly with markers of depression.” Recently published studies by Hutti et al. (Reference Hutti, Myers and Hall2017) have been promoting the PGIS, as an instrument comparable to PGS but shorter, easily to score and theoretically based which can predict grief outcomes at 3–5 months after loss. They advocate for the use of PGIS as a screening instrument, and not diagnosis, of women at greater risk for developing complicated grief, so they can be referred to specialists for further evaluation. More studies are needed to verify its conclusions, especially with different populations and cultures.
Considering factors related to grief scores, some — such as perception of support from friends and family and strong marital relationships — were consistently related to lower grief scores in every PGS subscale (Lasker and Toedter, Reference Lasker and Toedter1991; Kersting and Wagner, Reference Kersting and Wagner2012). Studies that looked at professional support and religiosity also found a positive association with lower grief intensity after perinatal loss, suggesting that these factors can positively influence the bereavement process. Other factors such as previous mental health issues or a personality with higher degree of neuroticism were found to be stronger predictors of complicated grief. Barr and Cacciatore (Reference Barr and Cacciatore2008) suggested that it is not yet clear whether detrimental factors such as pre-existing mental health or emotional issues prior to the loss can minimize the impact of the positive ones.
The cultural setting where a study is conducted may impact the factors being examined. For example, Al-Maharma et al. (Reference Al-Maharma, Abujaradeh and Mahmoud2016) examined the gender of the lost child and the subsequent one and found higher levels of grief associated with the loss of a male child and with having a subsequent female. The authors related to the cultural meaning of having a male child in an Arabic society, including Jordan: “a son can bring a family honor, financially support their families, take care of his parents in their older age, and carry their families’ names into future generations.” According to them, a male child loss often provokes more grief intensity than does the loss of a female child and a subsequent male child may contribute to facilitating the mother's grieving process. These two factors have not been studied in other cultures. Understanding families’ context within the culture where grief is being measured and exploring the many factors which might influence (for better or worse) the intensity of the bereavement process, would help health professionals to guide and to tailor the care provided based on the specific needs of each family. Nevertheless, screening all parents to detect those at risk for complicated grief, independently from any factor associated with severe grief, could prevent further delays in referring those in need to mental health care, in special, the ones who showed high scores in the subscales “Difficult coping” and “Despair” sooner after the loss.
One limitation of this review was including only articles in English, which might have left out some instruments designed in other languages to evaluate grief after perinatal loss. Most notable are the articles written in German referring to the MGS which were excluded and might have limited the scope of our work. Only three articles written in English using the MGS (Beutel et al., Reference Beutel, Willner and Volkl1995; Brier, Reference Brier2008; Scheidt et al., Reference Scheidt, Hasenburg and Kunze2012) were found in our search which shows that the instrument might be mostly used in German-speaking countries but has not been used or translated in other countries and cultures. On the other hand, the PGS has been translated and validated in many languages including German (Lorenzen and Holzgreve, Reference Lorenzen and Holzgreve1995) and has been used to detect grief reactions in different settings and cultures by being more accessible because of the language. Even when the search expanded from “scale” to “questionnaire,” “measure” and “assessment” to eliminate a possible source of bias, the number of studies using PGS dominated the literature. Another limitation was not assessing individual studies’ risk of bias. The reason for it was that the focus in this review was on including every study which used a specific instrument to measure grief in parents after perinatal loss independently from their designs, methodologies, or number of participants which could have limited the number of articles analyzed.
In the last decades, a better understanding of parent's needs after perinatal loss including miscarriages, which, in general, are treated as a simple occurrence in health care settings, increased the awareness for health care interventions that can help prevent complicated grief. Perinatal grief instruments have been used to evaluate pre- and post-interventions designed to help men and women deal with perinatal loss. In our review, we found five studies evaluating specific interventions and their impact on a family's bereavement process. Though interventions differ in format, length, and number of participants they showed decreased grief levels, but the difference was not always significant. Two interventions (Johnson and Langford, Reference Johnson and Langford2015; Roberts and Montgomery, Reference Roberts and Montgomery2016) showed significant effect on grief scores. Rocha et al. (Reference Rocha, Nunes and Leonardo2018) found no significant difference on grief scores but the effect size was considerable and anxiety and depression was significantly reduced. More studies, with higher numbers of participants are needed to determine which intervention is the most reliable to help parents recover.
Given the usually lmited resources available, programs designed to prevent complicated grief after any kind of perinatal loss should include an after loss follow-up and bereavement care, such as the PPC model. They could use instruments to measure parents’ grief reactions before and after such interventions as an assessment of their effectiveness.
Brier (Reference Brier2008) writing about miscarriages and Lorenzen and Holzgreve (Reference Lorenzen and Holzgreve1995) about pregnancy interruption due to fetal diagnostic suggested that clinicians should be aware of the intensity of grief present in such situations and the expected reactions. This review might help clinicians to better understand all perinatal loss reactions and therefore help guide patients’ expectations and needs, including putting together programs designed to prevent complicated grief or by identifying those parents in greater need to mental health care.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951520000826.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors declares that there is no conflict of interest.