Introduction
Cancer is the second most common cause of death worldwide, causing more than 8 million deaths each year. The incidence of cancer is expected to increase by more than 50% in the next decade (The ICGC/TCGA Pan-Cancer Analysis of Whole Genomes Consortium, 2020). One of the factors that impacts cancer patients’ health is spirituality, which can be seen as a universal attribute that individuals seek to develop and maintain hope and meaning in their lives (Cheng et al., Reference Cheng, Liu and Li2019). Spirituality is a dynamic and intrinsic dimension of human life that relates to the way individuals experience life, express themselves, and seek meaning, purpose, and transcendence (de Oliveira et al., Reference de Oliveira, Anderson and Lucchetti2019). Spiritual well-being is an important and positive tool for managing the often difficult changes in emotions, cognition, and behavior that come with a cancer diagnosis and living with the disease (Rademacher, Reference Rademacher2006).
Spiritual well-being is considered a multidimensional concept. Spiritual well-being is defined as “the affirmation of life in a relationship with God, self, community, and environment that nurtures and celebrates wholeness” (Ellison, Reference Ellison1983). Some cultures believe that suffering from a chronic condition like cancer is a punishment from God (Tabrizi et al., Reference Tabrizi, Radfar and Taei2016). Spiritual well-being is composed of two dimensions: existential, which is related to the meaning and purpose in life that is not dependent on one's religious thoughts, and religion, which deals with an individual's relationship with a greater power in the form of religious beliefs (Varner, Reference Varner2009). A definitive diagnosis of cancer does not necessarily mean the end of life; however, it raises the question, “What is the meaning and purpose of life?” (Rademacher, Reference Rademacher2006).
Spiritual well-being has been shown to positively impact an individual's hope, quality of life, life satisfaction, reduces one's mental stress (Boscaglia et al., Reference Boscaglia, Clarke and Jobling2005), and increases the survival chances of patients with cancer (Ahmad et al., Reference Ahmad, Binti Muhammad and Abdullah2011). Previous studies have also demonstrated that spiritual well-being is associated with lower levels of anxiety and depression (Martins et al., Reference Martins, Dias Domingues and Caldeira2019), better psychological well-being (Cheng et al., Reference Cheng, Liu and Li2019), and increased support and social interaction (Penman et al., Reference Penman, Oliver and Harrington2009). Generally, in major health crises, such as chronic and life-threatening diseases (e.g., cancer, diabetes, cardiovascular disease), spirituality and religion can play an important role in promoting quality of life and are valuable factors for adapting to cancer (Wilson et al., Reference Wilson, Forchheimer and Heinemann2017).
The concept of spiritual well-being is embedded in the culture and religious background of individuals. There is a need for an accurate tool to measure this concept among patients with cancer in the country of Iran, where Islam is the official religion. In Iran, there is increasing interest in the assessment of spiritual well-being as well as validation of a spiritual well-being scale among specific sub-populations, such as healthy people (Dadfar et al., Reference Dadfar, Lester and Turan2019), older populations (Hallaj et al., Reference Hallaj, Sahaf and Rafiey2014), psychiatric outpatients (Kazemzadeh Atoofi et al., Reference Kazemzadeh Atoofi, Dadfar and Turan2020), and patients with acute myocardial infarction (Soleimani et al., Reference Soleimani, Sharif and Allen2017).
Several scales have been developed to evaluate spiritual well-being: the Functional Assessment of Chronic Illness Therapy — Spiritual Well-Being (FACIT-Sp) scale, with 12 items and 3 subdomains: peace, meaning, and faith (Bredle et al., Reference Bredle, Salsman and Debb2011); Fisher's Spiritual Health and Life-Orientation Measure (SHALOM), with 20 items in 4 domains: personal, communal, environmental, and transcendental (Fisher, Reference Fisher2010); and the spiritual well-being scale (SWBS), comprised of 20 items with 2 subscales: existential well-being (EWB) and religious well-being (RWB) (Paloutzian and Ellison, Reference Paloutzian and Ellison1982).
Given that the concept of spiritual well-being is a structure that is influenced by culture and beliefs, accurately measuring the concept requires a scale appropriate to the Iranian-Islamic context. In the present study, psychometric evaluation of the Persian version of the SWBS was performed because it is a widely used and appropriate tool for patients with cancer and has been used in the Iranian population for other chronic diseases. The aim of this study was to evaluate the psychometric properties of the Persian version of the SWBS among Iranian patients with cancer.
Methods
This cross-sectional, methodological study was conducted among patients with cancer admitted to hospitals affiliated with the Iran University of Medical Sciences from June to December 2019.
Study sample
According to Kellar and Kelvin (Reference Kellar and Kelvin2012), the minimum sample size for conducting a factor analysis is equal to between 5 and 10 times more than the number of items of the intended instrument. As the Persian version of the SWBS contains 20 items, 400 patients with cancer were recruited into the study via convenience sampling. The first 200 participants in the sample were used to conduct the exploratory factor analysis (EFA) and the second 200 were used to evaluate the confirmatory factor analysis (CFA). The researcher explained study goals to the patients with cancer in the oncology wards of the university hospitals, and selected the patients who were willing to participate in the study and also met the inclusion criteria. The inclusion criteria for participants required that individuals be literate, an adult (≥18 years of age), and free from any psychological disorders (and not using psychiatric drugs).
Instruments
In this study, the questionnaire consisted of two parts. First, demographic and cancer information was collected, including age, sex, marital status, educational level, employment, economic status, type of cancer, type of treatment, cancer stage, and years of being a patient with cancer. The second part included the Persian version of the SWBS (Abhari et al., Reference Abhari, Fisher and Kheiltash2018). The permission for the use of this scale was obtained from Dr. Marzieh Nojomi. The Persian version of the SWBS consisting of two subscales: religious well-being (10 items) and existential well-being (10 items). The religious well-being subscale provides a self-assessment of one's relationship with God, while the existential well-being subscale offers a self-assessment of one's sense of life purpose and life satisfaction (Paloutzian and Ellison, Reference Paloutzian and Ellison1982). The Persian version of the SWBS is scored on a 6-point Likert-type scale from 1 (completely disagree) to 6 (completely agree), with a reversed scoring method used for negative questions (items 1, 2, 5, 6, 9, 12, 13, 16, and 18). The range of scores for each of the subscales was between 10 and 60. Higher scores indicated higher religious or existential well-being.
Content validity
In this phase, content validity ratio (CVR) and content validity index (CVI) for the items were calculated by 10 faculty members in psychiatric nursing. The CVR examined the items’ necessity (not necessary = 1, useful but not essential = 2, essential = 3). The formula for CVR is (Ne − N/2)/(N/2), in which the Ne is the number of experts indicating “essential” and N is the total number of experts (Zamanzadeh et al., Reference Zamanzadeh, Ghahramanian and Rassouli2015). When the number of experts is 10, the minimum acceptable CVR is equal to 0.62 (Lawshe, Reference Lawshe1975). To calculate CVI, ten experts (same as for CVR) evaluated the relevancy of items by dichotomous response: relevant = 4 and irrelevant = 1. The CVI was calculated by dividing the number of items experts rated as relevant (rating of 4) by the total number of experts (i.e., 10) (Zamanzadeh et al., Reference Zamanzadeh, Ghahramanian and Rassouli2015).
Construct validity
In this study, construct validity was measured using the EFA, CFA, and discriminant and convergent validity. Construct validity was evaluated through maximum-likelihood exploratory factor analysis (MLEFA) with Varimax rotation on the first set of 200 responses. The Kaiser–Meyer–Olkin test (KMO) and the Bartlett's test of sphericity were used to check the appropriateness of the study sample and the model. The number of factors was determined based on parallel analysis and exploratory graph analysis (EGA; Ledesma and Valero-Mora, Reference Ledesma and Valero-Mora2007; Golino and Epskamp, Reference Golino and Epskamp2017). Items with absolute loading values of 0.3 or greater were considered appropriate (Çokluk and Koçak, Reference Çokluk and Koçak2016).
The presence of an item in a latent factor is determined based on a factor loading of almost 0.3, which is estimated using the following formula: ![]() ${\rm CV} = 5.152 \div \surd ( n\ndash 2)$, where CV is the number of extractable factors and n is the sample size (n = 200). Next, items with communalities less than 0.2 were excluded from the EFA.
${\rm CV} = 5.152 \div \surd ( n\ndash 2)$, where CV is the number of extractable factors and n is the sample size (n = 200). Next, items with communalities less than 0.2 were excluded from the EFA.
For the assessment of the structural factors, a CFA was conducted using the maximum-likelihood method and the most common goodness-of-fit indices among 200 samples. The model fitness was assessed according to root mean square of error of approximation (RMSEA), comparative fit index (CFI), parsimonious comparative fit index (PCFI), parsimonious normed fit index (PNFI), incremental fit index (IFI), and CMIN/DF. For the CFA, items with a standardized factor loading lower than 0.5 were removed from the model.
Convergent and discriminant validity
The convergent and discriminant validity of the Persian version of the SWBS were estimated using Fornell and Larcker's approach (Fornell and Larcker, Reference Fornell and Larcker1981). Based on the results of the CFA, the two indices of average variance extracted (AVE) and maximum shared squared variance (MSV) were estimated to assess the convergent and discriminant validity of the extracted factors. According to recent studies, to establish convergent validity, (a) AVE should be greater than 0.5 or (b) composite reliability (CR) should be greater than AVE, (c) and all factor loadings should be significant, (d) and all standardized coefficients of the final model in CFA should be equal or greater than 0.5 (Malhotra and Dash, Reference Malhotra and Dash2016; Pahlevan Sharif et al., Reference Pahlevan Sharif, Mostafiz and Guptan2018b; Pahlevan Sharif and Sharif Nia, Reference Pahlevan Sharif and Sharif Nia2020). To meet the discriminant validity criteria, the MSV of each construct should be less than its AVE (Henseler et al., Reference Henseler, Ringle and Sarstedt2015).
Reliability
Internal consistency was assessed using Cronbach's alpha (α), McDonald's omega (Ω), and average inter-item correlation (AIC). Coefficients Ω and α values greater than 0.7 were acceptable (Mayers, Reference Mayers2013). An AIC between 0.2 and 0.4 indicated good internal consistency (Mohammadbeigi et al., Reference Mohammadbeigi, Mohammadsalehi and Aligol2015). CR, which replaces Cronbach's alpha coefficient in structural equation modeling, was then evaluated, with a CR value greater than 0.7 considered acceptable (Sharif Nia et al., Reference Sharif Nia, Shafipour and Allen2019).
Multivariate normality and outliers
Univariate distributions were examined for outliers, skewness, and kurtosis. Multivariate distributions were evaluated for normality and multivariate outliers. Multivariate normality can be evaluated through the use of the Mardia's coefficient of multivariate kurtosis. One indication of deviation from the normal distribution is a Mardia's coefficient greater than 8. Multivariate outliers were evaluated through the evaluation of a Mahalanobis distance. Items with a Mahalanobis distance of p < 0.001 were considered to be multivariate outliers (Esposito Vinzi et al., Reference Esposito Vinzi, Chin and Henseler2010). All of the statistical procedures were analyzed using SPSS-AMOS (V. 24), JASP (V. 13.1), SPSS R-menu (V. 2), and R software.
Ethical considerations
Informed consent was obtained from all individual participants included in the study. Patients were informed about the study aims and procedures. Moreover, they were assured that participation was voluntary and that it would not affect the course of their treatments and all their information will be confidential. The protocol of this study was approved by the Mazandaran University of Medical Sciences Research Ethics Committee (IR.MAZUMS.REC.1399.8740).
Results
The mean age of patients was 51.31 years old (SD = 15.9; range = 19–91) and most of them were married (83%). The mean number of years patients reported having cancer was 4.24 (SD = 3.7). Other socio-demographic and cancer information about patients is provided in Table 1.
Table 1. Socio-demographic and cancer information of participants (n = 400)

Regarding CVR and CVI, all items had an acceptable CVR between 0.8 and 1, and acceptable CVI (>0.7). Skewness, Kurtosis, and Mardia's coefficient confirmed that the data were normal (see Table 2).
Table 2. Exploratory factors extracted from 17 items of the Persian version of the SWBS (n = 200)
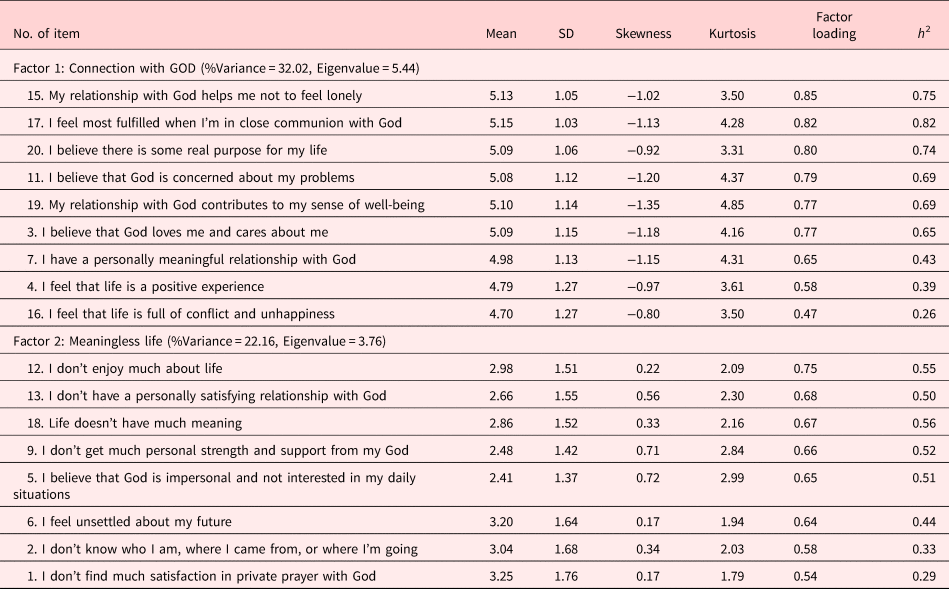
In the MLEFA, the KMO test value was 0.89 and Bartlett's test value was 1874.30 (p < 0.001). The MLEFA revealed a two-factor structure for the Persian version of the SWBS (n = 17) with the two factors of connecting with God (9 items) and meaningless life (8 items) (see Figures 1 and 2). The eigenvalues of these two factors were 5.44 (extracted variance: 32.02%) and 3.77 (extracted variance: 22.17%), respectively. These two factors explained 54.19% of the total variance of the Persian version of the SWBS in Iranian patients with cancer (see Table 2 and Figure 3).

Fig. 1. Parallel analysis scree plot.

Fig. 2. Exploratory graph analysis.

Fig. 3. Loading strength of each item.
After modifying the CFA, all goodness-of-fit indices confirmed the model fit (χ 2 = 211.996; n = 200; df = 100, p < 0.001; PCFI = 0.778; PNFI = 0.735; CMIN/DF = 2.120; RMSEA = 0.075 (CI 90%, [0.061, 0.081]); IFI = 0.934; CFI = 0.933; see Table 3 and Figure 4). Item 16 was removed from the model because it has a standardized factor loading lower than 0.5 (0.45); thus, the total number of scale items is 16.

Fig. 4. Model of confirmatory factor analysis of the Persian version of the SWBS (n = 200).
Table 3. Fit model indices of the CFA of the Persian version of the SWBS

a Acceptable values are as follows: >0.5 for CMIN/DF, PCFI, and PNFI; <0.08 for RMSEA; and >0.9 for CFI and IFI.
The MSV smaller than AVE, and CR greater than AVE, indicating both factors have good divergent and convergent validity, respectively (see Table 4). The Cronbach's alpha, McDonald's omega, and the AIC values of the factors indicated excellent internal consistency (see Table 4).
Table 4. Internal consistency, convergent and discriminant validity, and composite reliability indices of the Persian version of the SWBS

Discussion
The results of the present study supported a two-factor structure: connecting with God and meaningless life, with 16 items from the Persian version of the SWBS. An EFA showed that these two factors explained 54.189% of the total variance of the Persian version of the SWBS in Iranian patients with cancer. The findings of Soleimani et al.'s study supported two factors (relation with God, relation with life) in patients with acute myocardial infarction, which explained 50.65% of the variance (Soleimani et al., Reference Soleimani, Sharif and Allen2017). Another study conducted with veterans who experienced chemical weapon exposure, extracted three factors (relationship with God, belief in fate and destiny, and life optimism), explaining 48.20% of the total variance (Sharif Nia et al., Reference Sharif Nia, Pahlevan Sharif and Boyle2018). The difference in the number of factors extracted may be due to differences in participants’ views and responses. It should be noted that just as spiritual beliefs vary from person to person, so will spiritual well-being be different in cultural subgroups (Pahlevan Sharif et al., Reference Pahlevan Sharif, Lehto and Sharif Nia2018a).
The internal consistency of items of the Persian version of the SWBS was good, and the high Cronbach's alpha signifies suitable internal consistency of the scale and correlation between items. The reliability of this scale was evaluated separately for each exploratory factor using CR, which was at a high level. An advantage of measuring CR rather than Cronbach's alpha is that CR is not affected by the number of scale items or obtained structure and is dependent, rather, on the actual factor loading of each item on the latent variable (Vinzi et al., Reference Vinzi, Chin and Henseler2010). To the best of our knowledge, the present study is the first to calculate the CR value of the SWBS.
In the current study, the first factor extracted was connecting with God, which addressed, for example, close communication with God and help and attention from God. In line with this, previous studies reported that a strong relationship with God can reduce stress and anxiety, and increase hope and a sense of purpose in life among patients with chronic illnesses (Cheng et al., Reference Cheng, Liu and Li2019; Martins et al., Reference Martins, Dias Domingues and Caldeira2019). In Iran, being Muslim is associated with increased faith in God. When Muslims are affected by chronic or intolerable diseases such as cancer, they often report that their religious beliefs and practices are a source of comfort in reducing physical and spiritual distress (Sajadi et al., Reference Sajadi, Niazi and Khosravi2018). In general, experiencing an interconnectedness with self, others, and God, and providing guidance in the search for life's meaning and purpose, may help patients with cancer tolerate suffering and decrease burden throughout the disease (Spatuzzi et al., Reference Spatuzzi, Giulietti and Ricciuti2019).
The second factor extracted, meaningless life, included, for example, not having joy and meaning in life and experiencing dissatisfaction about one's relationship with God. The need for meaning is a universal trait that is essential to life itself. Meaning and purpose of life impacts individuals’ spiritual well-being differently depending on one's worldview. Indeed, these patients may struggle with questions about mortality or the meaning of life, possibly without coming to positive conclusions. Similar to previous studies, spiritual well-being comes from the positive emotional experience that results from one's ability to experience meaning and purpose in life through one's relationship with oneself, others, and a higher power (Soleimani et al., Reference Soleimani, Sharif and Allen2017; Sajadi et al., Reference Sajadi, Niazi and Khosravi2018; Rabitti et al., Reference Rabitti, Cavuto and Iani2020).
In the Islamic belief system, there is no difference between religion and spirituality. Religion and spirituality are largely considered the most important social factors in determining value and behavioral structures in human beings. One of the foundations of Islam is the belief in the afterlife. In accordance with these beliefs, the resurrection of the soul and body will take place on the “day of judgment” with either reward (paradise) or punishment (abyss of hell) as the final destination of every human being for eternity (Sharif Nia et al., Reference Sharif Nia, Ebadi and Lehto2015a). For patients with serious illnesses such as cancer, many consider the disease as torment or a test from God. When individuals feel that they have reached the end of their lives, they will suffer from anxiety and fear of death. Religious beliefs in these circumstances can create a positive attitude toward death, and communication with God can bring peace to these patients (Sharif Nia et al., Reference Sharif Nia, Haghdoost and Ebadi2015b; Komariah et al., Reference Komariah, Hatthakit and Boonyoung2020).
As the majority of Iranians are Muslim, Islamic teachings encourage people to tolerate negative life events; this particular religiosity may have a strong influence on spiritual well-being among Iranian patients with cancer. The results of this study showed that connecting with God, and creating meaning and purpose in life, explained the spiritual well-being of patients with cancer. Spiritual care is a neglected part of holistic care that helps patients with cancer to endure the therapeutic process. Religion plays an important role in the way individuals perceive suffering and illness and potentially contributing to mental health when facing a life-threatening stressor such as cancer.
Limitation
One limitation of the present study is that while participants were cancer patients with various types of cancer, the particular type or stage of cancer was not taken into account. For example, there may be differences in the spiritual well-being of end-stage cancer patients compared with those with stage one cancer. The generalizability of the study is another limitation, since the present study focused on one geographical region and religious group. Finally, there may be information bias as the data were collected via self-report.
Implication for practice
This study has demonstrated the value of understanding the spiritual well-being of patients at very difficult times in their lives. By being able to understand patient feelings of spirituality, clinicians may be able to tailor non-medical support to the particular needs of the patient. If spirituality is important to some patients, ensuring that this need is addressed may help with psychological as well as physical recovery.
Conclusions
The results of this study demonstrate that the Persian version of the SWBS in Iranian patients with cancer was multidimensional with two factors: connecting with God and meaningless life. These two factors explained 54.189% of the total variance of the concept of spiritual well-being in Iranian patients with cancer. The Persian version of the SWBS is a fundamental approach for measuring and improving cancer patients’ health through connecting with God and creating meaning and purpose in life among Iranian patients with cancer.
Acknowledgments
We thank all the participants who took part in the study.
Author contributions
All authors contributed to the study's conception and design. Data collection was performed by Mobin Mohammadinezhad, and the data were analyzed by Saeed Pahlevan Sharif and Hamid Sharif Nia. The first draft of the manuscript was written by Pardis Rahmatpour, Christopher Boyle, and Kelly A. Allen. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.











