Introduction
End-of-life of care is defined as the last weeks of life in which a patient with a life-limiting illness is approaching death (Rosenwax et al., Reference Rosenwax, McNamara and Murray2011). This phase involves increased use of services and support to maintain a good quality of life. End-of-life and anticipatory prescribing include the prescribing of certain medications to relief pain and control symptoms of deteriorating patients (Finucane et al., Reference Finucane, Stevenson and Gardner2014). Anticipatory prescribing is the proactive prescribing of medicines that are commonly required to control symptoms in community palliative care (Faull et al., Reference Faull, Windridge and Ockleford2013). These medications may be used to control symptoms at the last days of life (Finucane et al., Reference Finucane, Stevenson and Gardner2014). Anticipatory medications (AMs) have been widely used in various health care settings for people approaching end-of-life (Faull et al., Reference Faull, Windridge and Ockleford2013; Finucane et al., Reference Finucane, Stevenson and Gardner2014). Reasons for their use include: worsening of existing symptoms, the appearance of new symptoms, decrease in oral absorption of medications, inability of patients to swallow and anticipation for end-of-life symptoms, and patient distress (Faull et al., Reference Faull, Windridge and Ockleford2013; Finucane et al., Reference Finucane, Stevenson and Gardner2014). Lack of access to AM at times of need may result in unnecessary hospital admissions, increased patient and family distress, and decreased confidence in managing palliative care at home at end-of-life. AMs enable prompt relief when patients develop distressing symptoms (Baker et al., Reference Baker, Dargan and Smith2019; Thorns et al., Reference Thorns, Ward and Parker2019).
A recent survey of community palliative care and district nurses in Gippsland undertaken by our research team found community nurses played a substantial role in the management of AM for community palliative care patients (Khalil et al., Reference Khalil, Poon and Byrne2019b). Almost a third of all nurses surveyed did not have specific guidance regarding the use of AM for their patients. These results are also consistent with a qualitive study by Staats et al. (Reference Staats, Tranvåg and Grov2018) where home care nurses felt unsupported with the responsibility for assessing patients and their medications which often led to decisions being made at night shifts. Bowers and Redsell et al. (Reference Bowers and Redsell2017) have also explored the issue of prescribing these medications using interviews. On the contrary to the above, the authors found that the nurses in their study felt in control of advocating for their patients about when to recommend and prescribe medications and managed to alter the barriers between general practitioners (GPs) and nurses. However, this model is only applicable where nurses have the authority to prescribe medications which is only limited to certain countries.
Nurses also reported doctors were not willing to prescribe AM on some occasions due to the fear of drug misuse and/or abuse. Other challenges included lack of confidence about the usage and doses of AM, pharmacy shortages, and inability to access medications. These challenges are exacerbated by the rural and remote setting (Khalil et al., Reference Khalil, Poon and Byrne2019a).
Moreover, a recent systematic review found that there is a paucity of evidence on the current practice of end-of-life and anticipatory prescribing practice and policy (Khalil et al., Reference Khalil, Downie and Ristevski2020). The authors also found that current practice is lacking around end-of-life and AM prescribing and there was no reliable data on how often these drugs are used or prescribed (Khalil et al., Reference Khalil, Downie and Ristevski2020), as only 5 studies out of their 1,405 total included studies addressed end-of-life and AM prescribing. Robust evidence on the clinical effectiveness and their cost benefit was also lacking, although it is a low-cost intervention (Bowers et al., Reference Bowers, Ryan and Kuhn2019; Khalil et al., Reference Khalil, Downie and Ristevski2020).
Wilson et al. (Reference Wilson, Morbey and Brown2015) examined nurses’ decisions and concerns when using AMs in the UK. The authors found that nurses had a good understanding of when to initiate AM medications and how to assess patients appropriately for their need of AM. However, some nurses found the decision to initiate those actions to be emotionally demanding. These findings indicate that support and training are essential for these nurses to enable them to make the right choices for patients in need without thinking about avoiding hospital admissions or other urgent needs that patients may experience in the last days of life. Many factors are associated with prescribing and accessing AM, including clinicians’ confidence to prescribe and administer them, the presence of guidelines that govern their use in community settings, appropriate knowledge and education on their use, and potential risks such as overdose, death, and misuse (Khalil et al., Reference Khalil, Poon and Byrne2019a, Reference Khalil, Poon and Byrne2019b). In rural and remote areas, where there is limited access to specialist palliative care services and practitioners, there is a need to utilize shared care models of service delivery between specialists, generalists (e.g., GPs), and community-based services (e.g., community nursing) to support palliative care patients and their families (Khalil et al., Reference Khalil, Byrne and Ristevski2019c). Community-based palliative care models are important in Australia which has a geographically distributed population with rural and remote areas having a high number of people with lower socio-economic status and experiencing health workforce shortages (Khalil et al., Reference Khalil, Poon and Byrne2019a, Reference Khalil, Byrne and Ristevski2019c).
Given the importance of access to end-of-life and AM to ensure optimal end-of-life care, reduce suffering, and avoiding unnecessary admissions to hospital, our study aimed to map the use of end-of-life and AM in a cohort of palliative care patients visiting general practice through the use of the Population Level Analysis and Reporting (POLAR) Data Space and to discuss the results through stakeholders’ consultation of the relevant palliative care organizations.
Methods and analysis
Ethics clearance to collect data from general practice facilities has been obtained by the data provider from the Royal Australian College of General Practitioners National Research and Evaluation Ethics Committee (NREEC 17-008). Approval for the research group to use these data has been obtained from Monash and La Trobe Universities (Application number 19388).
Study design
A retrospective observational cohort study of Australian general practice clinical records was undertaken. This was followed by stakeholders’ consultation with community nurses and nurse managers working in palliative care organizations.
Data sources
Data were collected via the POLAR tool. The POLAR tool extracts de-identified data from consenting general practices on behalf of six Australian Primary Health Networks (PHNs). Data access to approved de-identified data from research-approved practices is managed via the Aurora research platform. The data are longitudinal in nature and include medications, diagnoses, visit details, and demographics. This study reports on data collected from 25 research-approved practices in the Gippsland PHN catchment. Only GPs were able to enter patient's records and management in the database. This database was not available to other service providers.
The data are structured in a relational database built on a unique identifier (%PatientSiteKey). This key represents a combination of the patient ID (in-practice) and the unique Practice ID resulting in patient activity being tracked in the practice. This database was described elsewhere and has been used in Australia by other research groups to study population health projects (Pearce et al., Reference Pearce, McLeod, Rinehart, Ohno-Machado and Seroussi2019; Youens et al., Reference Youens, Moorin and Harrison2020).
For this study, the extract was prepared using the flag “palliative” present in a patient's referral history. This exercise resulted in a cohort of 799 patients. In other words, 799 patients had a referral generated from their GP's medical software to a palliative care service. The extract included all patients with a palliative care referral independent of referral service. Free mapped and grouped as “palliative care” include (not an exhaustive list) palliative medicine specialist, palliative % rebab, pain management palliative, acute palliative care, service palliative, palliative care renal, community palliative care, geriatrics palliative, hematology and palliative, palliative care consultancy, palliative care inpatient-outpatient, and palliative home care service. The term free mapped or grouped mapped refers to whether it was entered as free text (free mapped) or chosen from a selection of terms (group termed).
Study population
The study population consists of all patients who attended any of the 25 general practices included in the study and had a “palliative” flag recorded in the practices’ electronic medical records software between 2009 and June 2019 irrespective of age or other services where patients received elsewhere.
Variables
The following variables were extracted from the Aurora database: patients’ status (active, inactive, or deceased), age, diagnosis (converted into ICD-11 classifications), number of visits, and medications. “Non-active” refers to patients not visiting GP in the last 5 years from their last appointment in the POLAR database where active refers to patients still current and still visiting the practice. For the purpose of this study, the AMs used are listed by PalliMEDS and included into the better safer care Victoria guidance (State of Victoria, 2020). These drugs include opioids, benzodiazepines, antiemetics, and anti-secretory in any form (oral and injectable).
Data analysis
Data were analyzed using IBM SPSS Statistics package version 24.0. Descriptive statistics was undertaken to determine the characteristics of palliative care patients. Correlational analysis as well as non-parametric tests such as Pearson's chi-square test were used to determine the association between patients’ characteristics, number of visits, and number of medications. Statistical significance is determined as p < 0.05.
Stakeholder consultation
Stakeholder consultation was undertaken in collaboration with the project advisory group consisting of members from Gippsland Palliative Care Consortium and Gippsland PHNs. Nurse practitioners in palliative care and GPs were contacted to participate in this stage of the project. The questions of the consultation were derived from the results obtained from the initial analysis of the POLAR database as shown in Table 1. A total of 13 health care practitioners were invited to a semi structured interview to seek their views on AM use in palliative care. The consultation was undertaken by a palliative care manager who coordinated services across the region. It is consisted of the following questions: understanding of AM prescribing and administration, awareness of referral pathways to palliative care services, barriers and facilitators to AM prescribing, and awareness of health pathways for GPs, which is a database of resources for those involved with caring for palliative care patients. The interviews were all hand-written by the manager and were sent to the lead researcher for analysis. The initial thematic analysis was done by the lead researcher and was verified by the manager later on to verify the meanings intended by the participants. Thematic analysis based on Braun and Clarke (Reference Braun and Clarke2006) was used to identify key issues arose from the consultation.
Table 1. Stakeholders’ consultations

Results
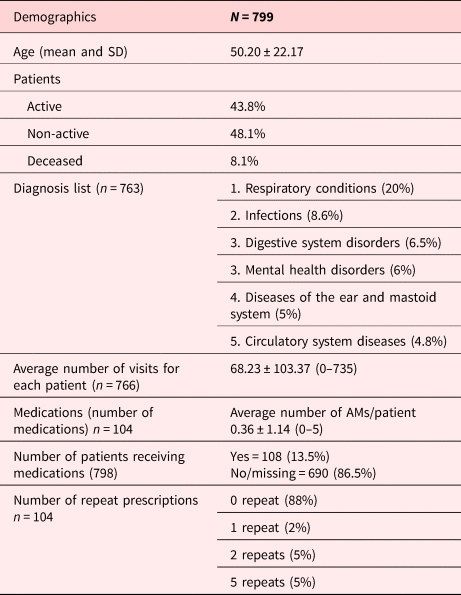
We identified within the data a total of 799 patients, with an average age of 50 years. The patients were almost equally divided between active (44%) and non-active (48%) and deceased patients were less than 8%. Active refers to current patients visiting that general practice, and non-active refers to patients who no longer visit that general practice (as marked by the practice). Patients visited the practice on average 68 times during the data collection period which is 10 years for some patients (see Table 2). Diagnosis was plotted as a frequency table for all patients. There was a total of 763 diagnoses. 20% of all patients had no specific symptoms matching a diagnosis recorded. Respiratory tract diseases, infections, digestive system diseases and mental health disorders are amongst the highest diagnosis. Diagnosis was also missing in 9% of patients. ICD-11 classification was used instead of SNOMED, as there were many symptoms that could not be mapped correctly to SNOMED texts as shown in Figure 1. Examples of these symptoms included tiredness, lightheadedness, dizziness, cough, etc.

Fig. 1. List of ICD-11 diagnosis (per cent of patients with a palliative care referral), n = 799 patients.
Table 2. Patients demographics

Medications profile
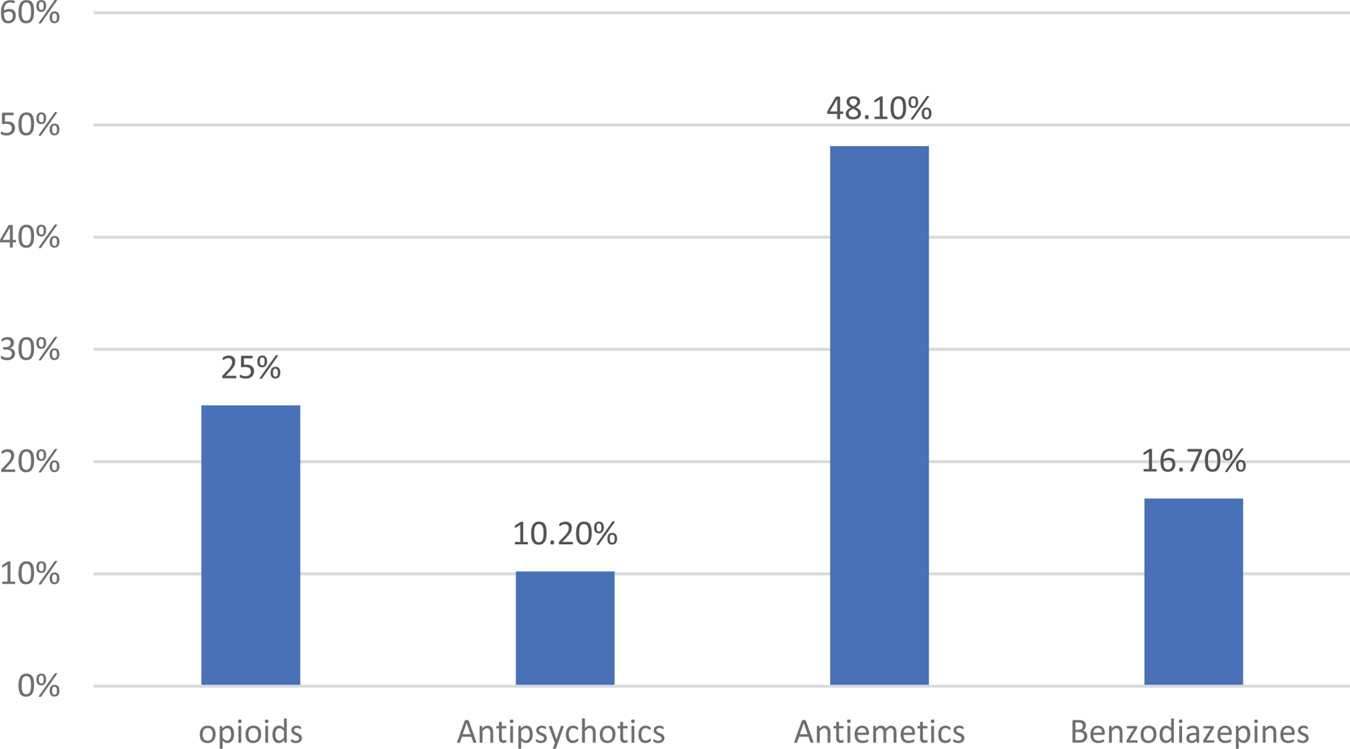
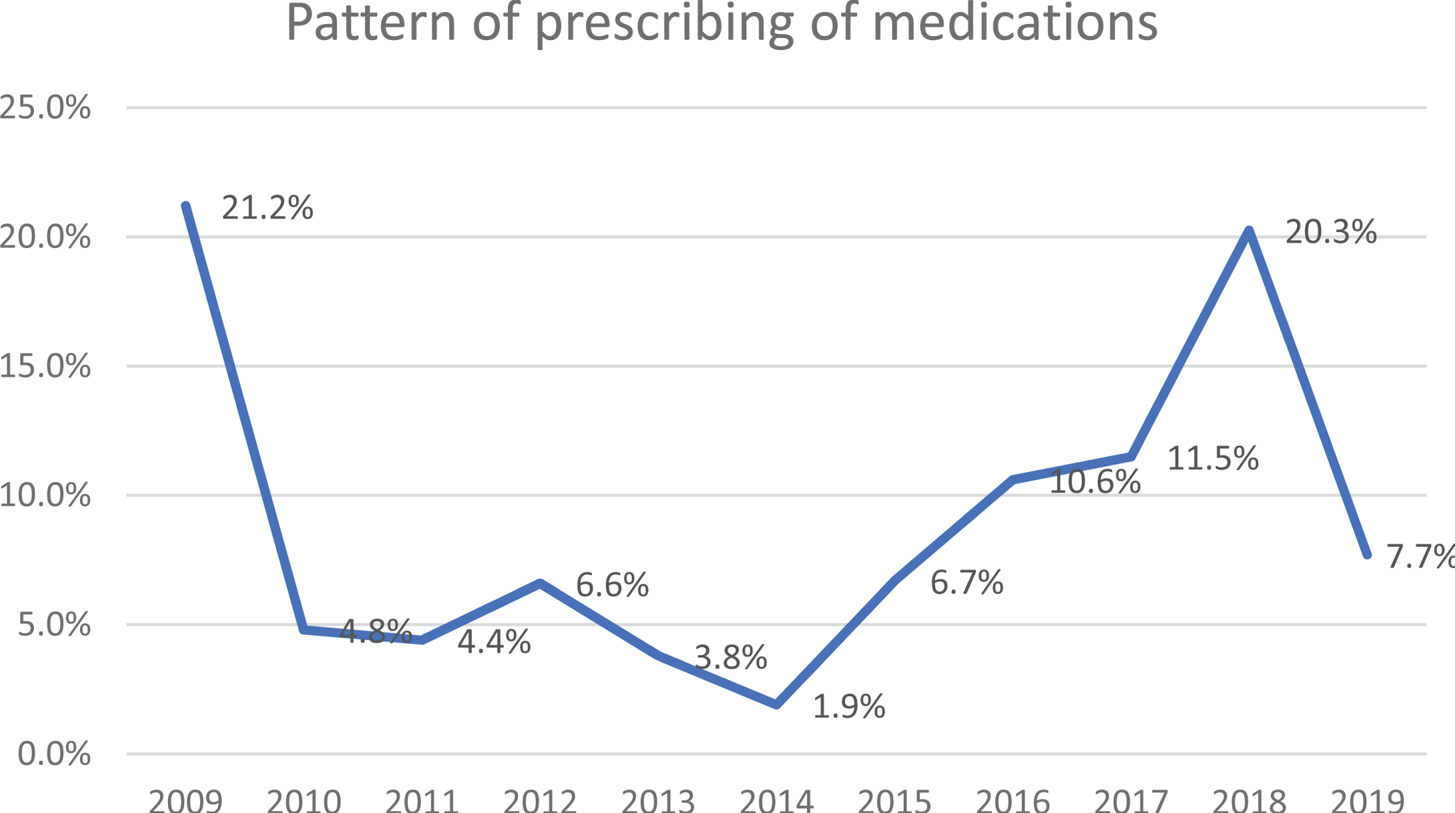
Only 104 (13.5%) patients had medications prescribed to them. The most frequently prescribed medications were antiemetics and opioids (see Figure 2). The pattern of prescribing of end-of-life and AM was plotted against the number of years as shown in Figure 3. Overall, there has been a steady increase in medications prescribing over the years up until 2018. The decrease seen in 2019 was due to the incomplete data collection for the year ending 2019. Drugs with different formulations were combined together as shown in Figure 2. Given the small sample size and lack of data for controlling other cofounding factors and/to compare the findings against, it is not quite clear if the dramatic dip from 2009 to 2010 is reflecting a real change or being affected by small sample size and perhaps some extreme outliers.

Fig. 2. End-of-life and AM prescribed by class (2009–2019).

Fig. 3. Pattern of prescribing of medications (per cent of patients with a palliative care referral), 2009–2019.
Correlational analysis
The frequency of the number of visits and medications to patient's age and diagnosis were compared separately by Pearson correlation or the non-parametric Pearson's chi-square test. There was a significant association between age of patients and number of visits (r = 0.440, p < 0.05) but not with patients’ age and number of medications (r = 0.07, p = 0.416). There was also a significant difference between patients’ diagnosis and number of visits [χ(840) = 901.15, p < 0.05; rs = 0.091, p < 0.05] but not with medications [χ(7) = 12.92, p > 0.05].
Stakeholder consultation
Despite vigorous attempts to elicit clinician responses to the questions on anticipatory prescribing in palliative care, the feedback was limited. The stakeholder consultation feedback consisted of a total of five nurse practitioners and GPs (response rate 39%).
In general, there was an agreement about when to prescribe AM. There was consensus that this was when a person is deteriorating or if the practitioner anticipates issues arising as a result of their diagnosis/prognosis. One practitioner stated prescribing when the patient becomes “home bound,” or when the community palliative care service is engaged. It was noted that a referral to community palliative care triggers a standard request for AM; however, the medications may not be required until end-of-life care months later, with scripts at the ready. Conversely, one respondent identified that AM prescribing varies enormously in palliative care because many prescribers believe it is only for the end-of-life; however, injectable medications may be required earlier due to the patient being unable to swallow oral medications or they have gastroparesis. Stakeholder engagement responses were consistent regarding specific medications required, particularly morphine, which did not align with the POLAR data on prescribing patterns. The POLAR database included information from the last decade of prescribing which could have changed over the years depending on guidelines used and prescribing patterns of GPs. The stakeholders’ consultation responses were based on an interview at one point of time where their responses reflected their current practice rather than their previous practice.
Although most stakeholder respondents reported that they had sufficient knowledge about referral pathways for palliative care patients, the knowledge of publicly available resources regarding AM prescribing, administration, and referral of patients to services varied amongst them. One respondent mentioned that knowing how to refer to community palliative care but did not know how to refer to palliative care physician; another referred to palliative care but was not aware of any other referral pathways such as community palliative care services; another was aware of the Primary Health Care Network Palliative Care Pathways but had not utilized them in their practice. Some practitioners were aware of the differing pathways across the subregions for referral to community and palliative care and palliative care consultancy service. Others provided several options for referrals for patients depending on the stage of their disease.
The response to end-of-life and AM barriers included identifying the right stage of patients’ condition at which medications can be prescribed. The fear of expediating death was also raised; opioid prescribing fear was voiced. However, the prescribing of oxycodone was more acceptable than parenteral morphine; prescriber lack of trust in the nurses arose from a perceived knowledge deficit in the identification of advanced disease. Medications access and ensuring that AMs were still within the correct expiry date for use were also raised as barriers. Some AM can be costly and not within some patients reach to access. Facilitators of AM prescribing included relationships and conversations with prescribers and nurses involved in patient's care and forward planning regarding when AM can be prescribed and used.
The knowledge about publicly available resources varied from knowing of them to knowing specific sites and pathways to refer patients in need to. For example, Health pathways is an evidence-based resource portal that has a wealth of information on chronic conditions and referral pathways. There was lack of knowledge about the website and the available resources.
Discussion
Main findings
In this retrospective cohort study, we investigated the prescribing patterns of end-of-life and AM in general practice over a 10-year period. To our knowledge, this is the first study to map end AM prescribing patterns in this setting. Previous studies were derived from clinicians’ surveys and their perspectives around AM use (Wilson et al., Reference Wilson, Seymour and Seale2016; Back, Reference Back2020; Bowers et al., Reference Bowers, Ryan and Kuhn2019).
Our study included a total of 25 general practices in a large regional area in Victoria, Australia. The study found that only 13.5% of all palliative care patients in the database received AM. The pattern of prescribing steadily increased between 2009 and 2018 and then dropped significantly in 2019 because of incomplete data collection. The 2019 data were incomplete as data were collected only until mid-year rather than a full-year cycle. This also coincided with the introduction of the Voluntary Assisted Dying (VAD) legislation in Victoria. We believe that if the data were extracted at the end of 2019, a consistent rise would have been observed. The VAD legislation raised awareness of prescribers about the importance of AM prescribing in end-of-life care. This was implemented through the release of guidance from the Royal College of General Practitioners about VAD and AM (RACGP, 2020).
These findings are somewhat consistent with an Australian study by Bullen et al. (Reference Bullen, Rosenberg and Smith2015) where the authors found low use of emergency medication kits in community palliative care. There were also significant variations in their use across different services depending on their jurisdiction. Antiemetics followed by opioids and benzodiazepines were found to be the highest prescribed AM (Leach, Reference Leach2019). This is somewhat different from other studies where opioids were considered the main AM prescribed for end-of-life care (Khalil et al., 2019) but consistent with other studies by Bowers et al. (Reference Bowers, Ryan and Kuhn2019) where midazolam and opioids were cited as the most prescribed drugs. Antiemetics are used for nausea and vomiting which are commonly experienced in palliative care patients due to impaired gastric emptying, chemotherapy, constipation, and other factors. They are also used as “when needed” medications for patients prescribed opioids and hence the reason for their high prescription rates in the database (Wiley, Reference Wiley2016; Milton-White and Linhartova, Reference Milton-White, Linhartova, Arora and Laha2018; Johnstone, Reference Johnstone2020). Masman et al. (Reference Masman, van Dijk and Tibboel2015) also found that morphine, midazolam, and haloperidol to be the most frequently prescribed medications at the day of death for patients in the largest palliative care study in the Netherlands in 2015.
This study found that advanced age and increased number of conditions significantly associated with increased visits to GPs for palliative care patients. A study by Le et al. (Reference Le, Eastman and Vij2017) highlighted that GPs are an integral part of these patients’ management. The authors suggested that increased resources and education to GPs has the potential to optimize the quality of care to these patients particularly in-home settings.
Moreover, a study by Wagner et al. (Reference Wagner, Patrick and Khandelwal2019) revealed that patients at end-of-life with increased number of chronic conditions had significantly higher use of health care services, including hospital admissions, emergency visits, and intensive care units (Milton-White and Linhartova,, Reference Milton-White, Linhartova, Arora and Laha2018). The authors also found that chronic obstructive pulmonary disease was the second highest diagnosis for which patients were admitted to hospital. This is also consistent with our findings of respiratory conditions to represent the most common diagnosis reported in the database.
The low number of palliative care patients prescribed AM recorded in the database triggered the need for the researchers to investigate reasons for the low numbers through stakeholders’ consultations of various community health provider groups including the regional palliative care consortium, community nurses, specialist nurses, and the regional primary health (general practice) network where education and training are offered to primary health practitioners in the regions.
A few concerns were raised through stakeholders’ consultation, and these were mainly around the correct identification of the stage of the patients’ condition to initiate AM prescribing. This could be facilitated with ongoing conversation with the patients’ family, and carers in conjunction with advance care planning, which is integral to optimal palliative care, especially in patients suffering from chronic conditions. A well-structured approach has the potential to improve the quality of care provided to these patients (Seeber et al., Reference Seeber, Pols and Hijdra2019).
Knowledge about appropriate referral pathways for palliative care patients visiting general practice was also raised during consultation. Similarly, knowledge of screening tools to identify patients with palliative care needs may be useful for health care practitioners to support patients and ensure timely care is provided. A recent study found that GPs rarely used prognostication tools to identify patients at end-of-life. Moreover, this process is even more challenging in frail and elderly patients (Pocock et al., Reference Pocock, Wye and French2019). The authors found that GPs would benefit from better screening tools to identify patients at end-of-life and more support from secondary care organizations with better communication and planning to improve patients care (Pocock et al., Reference Pocock, Wye and French2019).
This study is timely due to the approval of the VAD legislation in some parts of Australia and the release of Victoria state government guidelines for health care practitioners about the use of AMs.25,26 Currently, there is a plethora of research being undertaken in palliative care as shown by a recent systematic review by Khalil et al. (Reference Khalil, Downie and Ristevski2020). However, research into the barriers and facilitators of AM use and prescribing and end-of-life care need further attention. There is a wide variety of resources available to health care professionals working in palliative care; however, a more comprehensive resource is needed for not just management of palliative care patients but also identifying their stage of illness and prognosis to ensure optimal care (State of Victoria, 2017, 2020).
This study has a few limitations. Despite the large number of patients enrolled in the POLAR databases, there was only a small percentage of palliative care patients in the database, suggesting a diagnosis may not always be made or recorded even if clinically warranted. There was a high proportion of patients with no specific symptoms matching a diagnosis. This is a major limitation in our study in drawing firm conclusions from our data.
Medication data were provided based on an agreed medication list shared with Aurora staff prior to extract preparation. This list included clonazepam, fentanyl citrate, haloperidol, hydromorphone, hyoscine butylbromide, metoclopramide, midazolam, and morphine sulfate. Script data were provided for patients with a “palliative” flag in their record. It is not known if patients were receiving medications from specialist palliative care physicians, discharges from hospitals or from nurse practitioners in the community setting.
Moreover, the data extracted from the database were based on patients being classified as “palliative” by their GPs. It was difficult to distinguish between whether the extracted data were related to “reactive” or “anticipatory” prescribing, or a mixture of both. Qualitative interviews and focus groups with prescribers would be able to provide some information on this issue.
The number of patients in the database who were recorded with no end-of-life or AMs (86.5%) prescribed could also consist of missing information and not necessarily patients who were not prescribed medications. Our recruitment strategy for the stakeholder consultation was limited due to the availability of health care practitioners during the management of COVID-19 pandemic. This led to a smaller sample size of stakeholders’ participation than we initially anticipated. Nevertheless, the stakeholders involved were experienced practitioners working in palliative care and were well informed of the current issues in palliative care. It was also difficult to draw any conclusions from specialist versus generalist views due to the small sample size of the stakeholders’ group.
This is the first known study to retrospectively map end-of-life and AM use through a large database of palliative care patients from the general practice primary healthcare setting. Kemp et al. (Reference Kemp, Holland and Barclay2012), retrospectively, examined the records of all deaths occurring during 2009 in 12 diverse Cambridgeshire GP practices in the UK and found that preemptive prescribing for palliative care patients in primary care was used in 16% of predictable deaths. However, these were differences amongst practices. This research could be extended to other settings of interest and importance including residential aged care where further information on referral pathways and when medications are initiated would be of clinical value. Associations between AM prescribing and deaths could also be investigated further to guide clinicians about end-of-life and AM prescribing.
Conclusion
Only a small percentage of palliative care patients receive end-of-life and AM through general practice, it is believed the remainder access medications elsewhere. Stakeholder consultations from community palliative care organizations were sought to explain the small number of end-of-life medications and AMs prescribed. Stakeholder consultation highlighted that improved knowledge and information around referral pathways enabling access to palliative care services for general practice patients and their caregivers are needed. Similarly, the increased utility of screening tools to identify patients with palliative care needs may be useful for health care practitioners to ensure timely care is provided.
Availability of data and materials
The anonymized datasets supporting the conclusions of this manuscript are available upon request to the corresponding authors and health outcome.
Acknowledgments
The authors thank Ms Karina Gardner from Outcome Health Australia and her team for support with provision of AURORA data and ensuring it is available in an appropriate format. The authors also thank the stakeholders who provided their feedback on the use of AMs.
Author contributions
HK was the fund holder and the lead researcher, and she was responsible for the research design, data analysis, drafting the manuscript, and the overall completion of the Project. LK was the statistician undertaking the statistical analysis. AB was responsible for stakeholder consultation. KG was involved in data extraction and interpretation. MG was involved with the stakeholder consultation stage. PP was involved in providing a clinical input to the results, DA and LC were involved in commenting on the manuscript.
Funding
This work was funded by Gippsland PHN, Victoria, Australia.
Conflict of interest
The authors declare no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Ethics approval
The project was approved by La Trobe University Human Ethics Research Committee.