Published online by Cambridge University Press: 24 August 2005
Objective: To identify criteria for measuring the eligibility of patients with end-stage noncancer diseases for palliative care services in Australian residential aged care facilities.
Methods: No validated set if guidelines were available so five instruments were used: an adaptation of the American National Hospice Association Guidelines; a recent adaptation of the Karnofsky Performance Scale; the Modified Barthel Index; the Abbey Pain Score for assessment of people who are nonverbal and a Verbal Descriptor Scale, also for pain measurement. In addition, nutritional status and the presence of other problematic symptoms and their severity were also sought.
Results: The adapted American National Hospice Association Guidelines provided an initial indicative framework and the other instruments were useful in providing confirmatory data for service eligibility and delivery.
In the course of conducting a study to investigate the extent and nature of the provision of palliative care in residential aged care facilities for residents with end-stage noncancer diseases, we realized we lacked adequate criteria for identifying whether these people were nearing the end of their lives. Although palliative care has been advocated as a right for every person who is dying (Field & Addington-Hall, 1999) few palliative care services have focused on the needs of patients who die with conditions other than cancer.
The benefits and extension of palliative care beyond the limits of cancer have been recognized for well over two decades (Saunders, 1978; Wilkes, 1980, von Gunten & Twaddle, 1996), and techniques for physical and emotional palliation learned in the care of advanced cancer are often relevant to those with noncancer diagnoses, for example, in the use of small doses of opioids for severe dyspnea in cardiac failure or respiratory disease or for the persistent pain of advanced arthritis. Yet in the United Kingdom, New Zealand, and Australia only 3–16% of hospice patients have a noncancer diagnosis (Health Funding Authority, 1999; National Council for Hospice and Specialist Palliative Care Service, 2001; Palliative Care Australia, 2003) despite the fact that the noncancer deaths that could use palliation are estimated at 50% (Palliative Care Australia, 2003). This percentage is supported by U.S. figures where 49.5% of patients served by hospices had a noncancer diagnosis in 2002 and these figures have shown a dramatic increase from 38% in 2000.
Clearly, patients with noncancer diseases can benefit from specialist palliative care services, skills, and hospice philosophy (Kite et al., 1999). However, assessing the palliative care needs of these patients is dependent on identifying the terminal phase, which can be problematic (Luddington et al., 2001). A large U.K. national multimethod study on the management of death and dying in residential and nursing homes for older people conducted by Sidell et al. (1997) found that managers found it difficult to identify the beginning of the terminal phase of an illness and tended to make decisions related to functional demise.
In an attempt to address the disparity and provide clinicians and policy makers with some framework for assessing which patients could be eligible for hospice services, the American National Hospice Organization (NHO; National Hospice Organization, 1996) published medical guidelines for determining prognosis in selected noncancer diseases. These guidelines specified eligibility criteria for patients who could be enrolled in hospice services in the United States and, thus, are markers of prognosis and specific advanced morbidity. However, the prime purpose of the NHO guidelines was to qualify patients for the Medicare Hospice Benefit, which requires a prognosis of 6 months. The NHO guidelines suggest that patients who have a Karnofsky Performance Status Scale (KPS) of 50 or less and require others to perform at least three of the six activities of daily living are more likely to die within the next 6 months. The activities of daily living used to determine the dependency of an individual on others and level of impaired functional status included “bathing, dressing, feeding, transferring, continence of urine and stool, (and) ability to ambulate independently to the bathroom” (von Gunten & Twaddle, 1996).
In assessing Medicare's proposed hospice eligibility criteria for select noncancer patients it was found that these criteria would “not have identified accurately those patients with less than six months to live upon admission to hospice” (Schonwetter et al., 1998). Lynn (2001) subsequently adapted the NHO guidelines, presenting them in two parts: Part one consisted of three criteria with subgroups that require the patient to meet all the criteria in order to be enrolled in a hospice program in the United States, and are illustrated in Table 1.
NHO general guidelines (Lynn, 2001)

Part two highlighted guidelines for specific diseases ranging from blood tests to clinical descriptors. For example, serum levels: creatinine clearance <0.17 ml/s (10 ml/min) and serum creatinine greater than 707.2 μmol/l (8.0 mg/dl). Table 2 shows the inclusion criteria (clinical descriptors) for specific noncancer diseases that require the clinical judgment of health care professionals (Lynn, 2001). However, blood tests to elicit such results are not routinely conducted in aged care facilities in Australia, so further adaptation of these guidelines was required.
NHO specific disease criteria (Lynn, 2001)

Following the debates above, members of the research team in our study further adapted the work of Lynn (2001) for use in Australian residential aged care facilities. Table 3 outlines the adapted inclusion criteria.
NHO guidelines (adapted) for Australian residential aged care facilities

Other broad criteria for hospice/palliative care eligibility used to predict prognosis without taking into account specific diagnoses but including a number of disparate “clinical indicators which taken together, are predictive of a short life expectancy on the order of 6 months or less” (von Gunten & Twaddle, 1996, p. 352) can be grouped under two categories: impaired functional status and impaired nutritional status. Those used in this study are listed below.
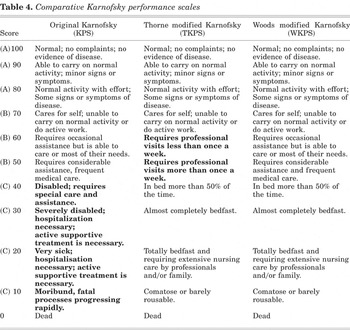
The Karnofsky Performance Scale (KPS; Karnofsky et al., 1948; Karnofsky & Burchenal, 1949) is one of the better known prognostication scales in oncology and has been a method of “quantifying patients' status relative to degree of independence in carrying out normal activities and self care” (Yates et al., 1980, p. 2220). Some have considered the KPS tool to have high predictive capacity for quantifying the physical functioning of patients with cancer (Hutchinson et al., 1979; Grieco & Long, 1984; Mor et al., 1984; Schag et al., 1984; Conill et al., 1990; Nikoletti et al., 2000) and in assisting with prognostication because there is an association between low KPS scores and shortened life expectancy. The tool has 11 levels ranging from normal functioning (100) to dead (0). A patient with a terminal disease and a KPS score of 50 or less is deemed to have a limited prognosis (Evans & McCarthy, 1985).
However, there have been problems with the scoring system when using the KPS in the home palliative care setting (Nikoletti et al., 2000). Specifically, the first problem is the descriptor related to the location of care. Descriptors for ratings at 20 and 30 in the KPS include assessing the need for hospitalization. Philosophically, this descriptor is at odds with the goal of supporting patients and families in their wish for a home death (Nikoletti et al., 2000). Indeed, one could argue that residents in aged care facilities consider this setting their home and their bed to be the place where they wish to die, thus the need to provide quality palliative care in the domiciliary setting is unequivocal. In addition, Nikoletti et al. (2000, p. 301) state: “the second concern is that the KPS scores in advanced cancer populations tend to cluster at the low end of the scale, indicating the need for more sensitive descriptors that reflect clinically significant changes in physical function.” David Thorne developed the Thorne KPS (TKPS; unpublished but delineated in Nikoletti et al., 2000, and tested in a pilot study against the KPS for use in the home hospice setting by Kristjanson et al., 1998). It specifically does not assess the location of care, nor the need for hospitalization, and modifies the descriptors in the middle and lower levels of the scale. The usefulness of the KPS and the TKPS was evaluated by Nikoletti et al. (2000), who suggested that although agreement was only 47%, the TKPS identified a larger proportion of home hospice patients at lower levels of function and may be a more sensitive indicator of performance at these levels, which would be a distinct advantage for palliative care populations.
The middle range of scores in the TKPS refers to professional visits that the patient may need either less (B 60) or more than once a week (B 50; see Table 4). These particular functional status indicators are neither relevant nor useful for patients in hospitals or in aged care facilities (Woods, 2001). Moreover, in relation to the TKPS functional assessment tool, Woods (2001, p. 2) states, “the measure does not appear to reflect perceived need for services rather than perceived functional status—professional visits may be required frequently for symptom control reasons or interventions not related to functional status, e.g., frequent dressing changes in patients able to carry on normal activity.” In addition, Woods reports that, in order to develop a functional status score that would be suitable to be used in both in-patient and domiciliary settings, modification of both the KPS and TKPS was necessary. He developed a new functional status assessment tool known as the WARP Karnofsky WKPS (illustrated below). The emboldened areas in Table 4 represent scale definitions discarded in the development of the WKPS (Woods, 2001).
Comparative Karnofsky performance scales
The Barthel Index (BI) measures performance based on the degree of assistance required by an individual to perform 10 items of mobility and self-care, including dressing, eating, elimination, hygiene, mobility, working, and shopping. Validity and reliability of the Barthel Index have been established (van der Putten et al., 1999). In palliative care, Bennett and Ryall (2000, p. 158) noted that “in patients in hospice the rate of change in physical functioning was a more useful indicator of survival then absolute measures.” In our study, we utilized the 10-item modified Barthel Index (McDowell & Newell, 1986) in the initial and final assessment of participants, spanning a 10-week period.
Impaired nutritional status has predictable consequences. An increased probability of death correlates with patients who demonstrate more than 10% weight loss over a previous 6-month period that is unplanned and progressive (NHO, 1996; von Gunten & Twaddle, 1996). Also, a broad correlation can be drawn with impaired performance status in patients. In other words, there is a strong likelihood that impairment of nutritional and performance status exists in patients who have advanced noncancer diseases.
This is a 1-min numerical indicator of pain status developed for people with end-stage dementia and limited verbalization in residential aged care facilities who require palliative care (validated in Abbey et al., 2004). Vocalizations, facial expressions, body language, and behavioral, physiological, and physical changes are monitored and rated to give an overall score.
This instrument was developed to assess pain in cancer patients and its reliability has been indicated (Grossman et al., 1992). Patients' rate their pain on a 6-point scale ranging from no pain to mild, discomforting, distressing, horrible, or excruciating pain.
The study wherein these inclusion criteria were used, aimed to describe the demographic and clinical profiles of residents with noncancer diagnoses who die in aged care facilities in urban and rural South Australia, to assess the palliative care needs of these residents, to examine the current contribution and demand for palliative care services to aged care facilities, and to provide strategies to address unmet needs.
A multimethod two-stage approach utilizing quantitative and qualitative methods was used. In Stage 1 a representative sample of the 298 residential aged care facilities in South Australia were surveyed to quantify the extent of specialist palliative care involvement, provide information on resident death rates, and to estimate the current need for palliative care for those with noncancer diagnoses. In Stage 2 a random sampling of metropolitan and rural facilities identified 23 in whom there were participants with noncancer disease who were considered, using the NHO's adapted guidelines and following discussion with registered nurses in each residential aged care facility, to be nearing the end of life, and from these, 69 residents agreed to participate (see Fig. 1).

Geographical distribution of the sample of residents from aged care facilities (n = 69) in Adelaide and rural and regional centers of South Australia.
Details regarding the palliative care needs and services required for residents with a noncancer diagnosis were collected prospectively over a 10-week period at each metropolitan and rural site. A comprehensive initial assessment was conducted on each participant using the WARP Modified Karnofsky Score, the Modified Barthel Index, the Abbey Pain Score, and the Verbal Descriptor Scale. Case notes and staff interviews enabled nutrition and symptom assessment. Subsequently, four assessments were conducted on a fortnightly basis, and a final assessment was completed at the end of 10 weeks.
The adapted NHO guidelines provided a general tool for the researchers and staff in aged care facilities to identify more precisely residents with noncancer diagnoses who were considered to be nearing the end of life.
The mean initial WKPSs for all residents were well under the 50 indicated by the NHO guidelines. The initial score was 32.6 and the final score 10 weeks later was 31.6. There were no significant differences between the initial and final scores (t = 0.806, df = 68, p = 0.423). However, there was a trend toward a decrease in WKPS from initial to final assessment. Figure 2 compares the mean initial and final WKPS scores for residents who did not die and those who did. There was no statistically significant difference between the initial scores for residents who did and did not die (27.5 and 34.2; t = −1.743, df = 67, p = 0.86). However there was a statistically significant difference between the mean final WPKS for residents who did not die and those who did (35.3 and 19.4; t = −4.0, df = 67, p = 0.00), indicating a decline in functional ability toward the end of life in residents who died.

Initial and final WKPS scores of residents (n = 69).
The maximum score of the Index is 20, which indicates ability to complete activities of daily living with minimal or no assistance. The initial Barthel score in the study was 3.1 and the final was 2.9, indicating a very low level of mobility and self-care capacity. There were no significant differences between the initial and final scores. Figure 3 indicates the initial and final Barthel scores for residents who died and those who did not. For residents who did not die, initial and final scores were equivalent (t = 0.463, df = 67, p = 0.645). However, for residents who died, there was a decline in the Barthel Score, indicating greater dependence, but this difference was not statistically significant (t = 0.56, df = 67, p = 0.577).

Initial and final modified Barthel Index scores by resident death.
Forty-four (64%) residents were on a limited diet (vitamized or soft food) at initial and final assessment. Nine (13%) residents had no oral intake in the final assessment, compared with three (4%) at the beginning of the study (Fig. 4).

Nutritional status (initial and final assessments).
When the above measurements are matched with information from case notes, the two pain scales, and interviews with clinical staff in the residential aged care facilities, there were a number of symptoms that would have benefited from specialist palliative input. The symptoms experienced by residents during the study were rated by the researchers into three degrees of severity, namely, mild, moderate, and severe, and recorded at each collection point. Mild indicated that there was an issue and it was managed well, sometimes by nonpharmacological means, and was generally resolved. Moderate indicated that there was an issue that was managed with a moderate degree of success, by using regular or prn (pro re nata; as the situation demands) medications in combination or separately, but the issue was an ongoing concern and required ongoing intervention(s). Severe indicated that there was an issue that was not controlled, regardless of interventions tried.
Figure 5 shows the most common symptoms that were rated moderate or severe as weakness/fatigue (49%), restlessness (42%), anxiety (42%), anorexia (38%), constipation (34%), oral discomfort (33%), and dysphagia (30%). While pain had been listed as present for 69% of residents only 16% of residents had pain that was moderate or severe.

Symptoms rated moderate or severe.
These results are similar to those of Cartwright (1991), who identified symptoms of both cancer and noncancer palliative patients. Pain, anorexia, insomnia, incontinence, and confusion were present in both populations, but were less prevalent for those with noncancer diseases, whereas dyspnea, anxiety, and constipation were much the same.
In the current study, symptoms, recorded in order of prevalence, were constipation (75%), pain (71%), dysphagia (57%), weakness (55%), dyspnea (32%), and depression (29%). Prevalence of symptoms does not indicate severity or indicate effectiveness of management techniques.
This study is the first in Australia to attempt to quantify whether resident deaths were related to a cancer or noncancer diagnosis. In Stage 1, four out of five deaths reported were related to a noncancer diagnosis. In Stage 2, only residents with a noncancer diagnosis were included and therefore all deaths were related to noncancer diagnoses. The multiple comorbidities of those 16 residents who died included 13 (81%) with haematological/cardiovascular disorders, 11 (69%) with dementia, six (38%) with pulmonary conditions, and four (25%) with neurological disorders. These figures are reflective of the national trend, where cardiovascular disease is the main cause of death for both males and females aged 85 years and older (Australian Institute of Health and Welfare, 2002). The overwhelming proportion of deaths with a noncancer diagnosis in this setting has important implications for palliative care service provision of support to residential aged care facilities.
This article reports on criteria used in order to identify patients in a study of residents in aged care facilities with end-stage noncancer diagnoses who should be considered for palliative services. Eligibility criteria for palliative care services, be they a palliative care approach, specialist palliative care, and/or palliative interventions, is an important topic within the broader palliative care debates. The inclusion guidelines developed comprised a combination of specially modified NHO guidelines together with the WARP Karnofsky Performance Scale, the 10-item modified Barthel index, two pain scales—one verbal and nonverbal—plus an assessment of nutritional status and identification of other problematic symptoms. Together these provided a useful and accurate approach to identifying patients with a noncancer diagnosis who should be considered for palliative services. The adapted NHO guidelines provided a general framework within which other tests could produce confirmatory data. Over the 10 weeks of data collection, results were consistent. The WKPS indicated that all 69 patients had a score well under the 50 required by the NHO guidelines (average 32); the Barthel Index indicated that patients averaged a low level of 3/20 for mobility and self-care. Nutrition information was equally indicative with 64% of the group being on vitamized or soft food with increasing numbers on nil orally. Although the results regarding pain and other symptoms could equally apply to patients who were not nearing the end of life, this information provided useful insights as to where symptoms were severe, where clinical staffs were having difficulties with management, and where palliative interventions would have been appropriate. The limitation of this study was the time frame of 10 weeks in terms of data collection, during which only 16 of the 69 patients died—a longer time frame may have produced results that were more statistically relevant, but the minimum variation in results between initial and final assessments of those who did and did not die clarified that the adapted guidelines worked well as a primary indicator.
This study has broad implications for service delivery to meet the needs of the increasing numbers of older people who will die from noncancer diagnoses. Given the principle that all people have a right to receive appropriate care and to die with dignity, it can be argued that the use of the adapted NHO guidelines together with pain scales and close monitoring provide a strategy for enabling the provision of appropriate end-of-life care for these patients and their families. Clarifying appropriate eligibility/inclusion criteria for people with noncancer diagnoses is a crucial step within the broader debates about palliative care approaches and specialist palliative care services. This article contributes to these critical debates.

NHO general guidelines (Lynn, 2001)

NHO specific disease criteria (Lynn, 2001)

NHO guidelines (adapted) for Australian residential aged care facilities

Comparative Karnofsky performance scales

Geographical distribution of the sample of residents from aged care facilities (n = 69) in Adelaide and rural and regional centers of South Australia.

Initial and final WKPS scores of residents (n = 69).

Initial and final modified Barthel Index scores by resident death.

Nutritional status (initial and final assessments).

Symptoms rated moderate or severe.