Published online by Cambridge University Press: 01 March 2004
Objective: Understanding the construct of hopelessness in the context of a life-threatening or terminal illness is a complex and challenging undertaking. The objective of this study was to examine the construct of hopelessness in patients with advanced AIDS by examining the structure of the Beck Hopelessness Scale in this specific population.
Methods: For the past three decades, the primary measure used to study hopelessness in a variety of populations has been the Beck Hopelessness Scale. Several factor analytic studies have been published using this scale, with studies of nonclinical samples typically describing a two-factor model (optimism and pessimism), whereas clinical samples have consistently generated a third factor (lack of motivation to make changes). We used confirmatory factor analysis to analyze two data sets in patients with AIDS.
Results: Confirmatory factor analysis of the Beck Hopelessness Scale in two samples of patients with far advanced AIDS revealed a clear superiority for a three-factor model.
Significance of results: The Beck Hopelessness Scale has unique characteristics when applied to a terminally ill population. The implications of these results for studies of terminal illness are discussed.
After nearly three decades of psychological research, the construct of hopelessness still remains enigmatic. Long considered merely a symptom of depression, Aaron Beck and his colleagues are credited with having first operationalized this construct with their publication of the Hopelessness Scale (HS; Beck et al., 1974). This 20-item self-report questionnaire was designed to tap a general tendency toward pessimism and negative expectancies (Beck et al., 1974). Since that time, researchers and clinicians have expanded upon Beck's original work with numerous studies focusing on the extent to which the construct of hopelessness informs our understanding of a wide range of social and psychological problems such as depression and other mental disorders, physical health and coping abilities, and behaviors such as suicide. Particular emphasis has been placed on hopelessness as a predictor of suicide among individuals with depression and other mental disorders (e.g., Beck et al., 1974; Steer et al., 1993; Aish & Wasserman, 2001), and hopelessness has more recently emerged as a strong predictor of desire for hastened death and refusal of life-sustaining interventions in the elderly and terminally ill (e.g., Breitbart et al., 2000; Menon et al., 2000). Yet although many researchers have noted the importance of hopelessness in understanding both psychological adjustment and behavior, considerably less attention has been focused on understanding precisely what is meant by the term “hopelessness,” particularly in the context of a life-threatening medical illness.
Understanding the construct of hopelessness is complicated considerably when an individual is diagnosed with a life-threatening or terminal illness. Clinicians and researchers often confuse the pessimistic cognitive style that was initially described by Beck and his colleagues with the prognostic assessments offered by medical professionals. Many individuals assume that an individual who is aware that he or she has a terminal illness must necessarily be “hopeless.” For example, one might presume that a patient with an incurable cancer, who is informed that there is “no hope” of a cure, would by definition be “hopeless” and accordingly would score high on a measure of hopelessness (e.g., the Hopelessness Scale). Yet, clinical observation and empirical research have not supported this assumption, as many medically ill or terminally ill individuals do not endorse large numbers of items on the HS (e.g., Greene et al., 1982; Breitbart et al., 2000; Menon et al., 2000). Hence, the need for a more thorough understanding of the construct of hopelessness clearly exists, particularly in the context of terminal illness.
The medical literature has typically linked hopelessness to the disease process in two ways. First, hopelessness in medically ill patients has been found to have a direct impact on health status. For example, several researchers have suggested that hopelessness may increase one's susceptibility to illness (e.g., Visintainer et al., 1982; Peterson et al., 1993; Everson et al., 1996), even after controlling for the effect of depression and other medical risk factors. Second, hopelessness appears to negatively influence disease course, in part by hindering patients' motivation to improve their health status. For example, Watson (1999) reported that hopelessness was negatively associated with survival in a sample of cancer patients. Scheier et al. (1989) found that dispositional optimism (often conceptualized as the opposite of hopelessness) predicted higher levels of problem-focused coping, faster recovery, and better postsurgery quality of life in coronary bypass surgery patients. This literature, drawing on Lazarus and Folkman's (1984) theory of coping, has suggested that patients who are extremely pessimistic are unlikely to utilize problem-solving coping strategies, possibly explaining their overall poorer health outcomes. Although several possible pathways between hopelessness, medical illness, and psychological well-being exist, relatively little empirical research has attempted to explore the construct of hopelessness in the context of medical illness.
One of the most common methods for exploring a theoretical construct such as hopelessness is through the use of factor analysis. Not surprisingly, many researchers have analyzed the factor structure of the Beck Hopelessness Scale over the past 30 years. Unfortunately, most of these studies have used exploratory methods to develop factor models with only superficial comparisons (if any) to other, previously published models. More importantly, none of these studies have investigated the construct of hopelessness in the context of a medical or terminal illness, despite the importance of this construct for medically ill individuals. We sought to fill this void in the empirical literature by examining the construct of hopelessness in patients with AIDS.
Our review of the literature concerning Beck's Hopelessness Scale revealed a surprising number of published studies employing factor analytic methods. It quickly became apparent that important differences might exist between studies of psychiatric patients (typically patients with depression) and nonclinical samples (typically college students or young adults), and therefore we discuss these literatures separately. Although some note is made of the different factor analytic methods, interested readers unfamiliar with the terms and elements of factor analysis and the differences in the various methods should consult one of the many available texts as a detailed review of factor analysis is beyond the scope of this article.
The first factor analysis of the hopelessness scale (HS) was conducted by Beck and his colleagues in their initial validation studies of the newly developed instrument (Beck et al., 1974). Using a sample of 294 hospitalized psychiatric patients who had made recent suicide attempts, they performed a principal components analysis with a varimax rotation (see Table 1). They extracted three factors based on the eigenvalues greater than 1.0. The first factor, which contained five of the positively worded items, was described as the “affective” factor because most of the items pertained to feelings of hope and enthusiasm. The second factor, which contained eight items (seven of which were negatively worded), was characterized as the “motivational” factor, with item content primarily focused around giving up and not wanting to try and achieve goals. The third factor, which contained four negatively worded items and one positively worded item, was labeled the “cognitive” factor, because item content was primarily focused on expectations of the future. Although not discussed by Beck et al., the influence of item phrasing on this factor solution has been noted by others (Steed, 2001) and has recurred in numerous studies, leading some writers to suggest that the positively worded items tap “optimism” whereas negatively worded items reflect “pessimism.”
Factor analytic studies of the Beck Hopelessness Scale

Nearly a decade elapsed before other researchers began analyzing the hopelessness scale, but the rate of published studies grew rapidly in the mid-1980s. Two studies published in 1983 (Mendonca et al., 1983; Nekanda-Trepka et al., 1983), both of which utilized psychiatric outpatients, generated markedly different findings that those of Beck et al. (1974). Both, however, utilized small sample sizes (78 and 86, respectively), making their findings, one-factor and five-factor models, respectively (both of which were based on a principal components extraction method), somewhat unstable. This instability was evidenced in the analyses reported by Mendonca, as their data revealed that a three-factor model was equally plausible (i.e., three factors had eigenvalues greater than 1.0 and their justification for rejecting this model in favor of a single factor was unclear).
Sample size concerns were not implicated in the analysis by Young et al. (1992), as these authors studied responses to the HS among two large samples of psychiatric outpatients. Using a maximum likelihood method, they found that a four-factor solution provided the “best fit” to their data but they concluded that a one-factor solution was preferable because the first factor accounted for such a large proportion of the variance and additional factors were largely uninterpretable.
Hill et al. (1988) used a principal components method to factor analyze the HS in a sample of 120 depressed elderly outpatients. Like Beck's earlier study, Hill et al. concluded that a three-factor model was the best fit for their data. But although their factor model overlapped somewhat with Beck's, Hill et al. labeled the three factors differently (see Table 2). Factor 1 was labeled “Hopefulness about the future,” Factor 2 was labeled “Giving up” and Factor 3 was labeled “Future anticipation.”
Item composition of factor analysis models

Steer et al. (1993) also conducted a series of factor analytic studies in several different clinical populations including adolescent psychiatric inpatients, psychiatric outpatients with anxiety and depression (Steer & Beck, 1997), and substance abusers seeking HIV testing (Steer et al., 1994). In three of these four analyses (outpatients with anxiety and depression were analyzed separately), the authors concluded that a three-factor solution provided the best fit for their data. In two of these analyses (Steer et al., 1993, 1994) the authors characterized their results as essentially replicating Beck et al.'s original three-factor model, although a review of the item loadings revealed that some differences in these models exist (see Table 2). However, their analysis of outpatients with anxiety and depression generated less straightforward findings. They utilized several different methods of analyzing the factor structure of these two samples (weighted least squares analysis of the tetrachoric correlations, principal components analysis of the G-index correlations, and principal components analysis of the phi coefficients), all of which were then rotated using a Varimax rotation, finding that a four-factor model best fit the data for the depressed sample and a three-factor model best fit the anxious sample. Nevertheless, they noted that very little additional variance was accounted for by any factors beyond the first and instead chose to interpret a two-factor model across both samples. Their final model included only seven items, four of which loaded onto the first factor (“pessimism”) and three of which loaded onto the second factor (“resignation to the futility of changing the future”).
Despite this large body of existing research, Dyce (1996) utilized a principal components method with varimax rotation to analyze the factor structure of the HS in a sample of 411 depressed psychiatric outpatients. Dyce retained three factors based on eigenvalues greater than 1.0, that appeared to be heavily influenced by item wording. The first factor, Expectations of success, included eight positively worded items and one negatively worded item. The second factor, Expectations of failure, included five negatively worded items, and the third factor, Future uncertainty, contained five negatively worded items and one positively worded item.
Finally, in the most recent addition to the HS factor analysis literature, Aish and Wasserman (2001) utilized a confirmatory factor analysis approach to compare the fit of their data to a range of different models (including those offered by Beck et al., 1974; Hill et al., 1988; Tanaka et al., 1988; Steer et al., 1993; Dyce, 1996). They found that none of the two- or three-factor models fit their data, derived from 324 Swedish adults recently admitted to psychiatric facilities following a suicide attempt. Instead, they reported that a one-factor model best fit their data set, and added that numerous variations (ranging in complexity from only 4 items to as many as 15) all provided an adequate fit. It should be noted, however, that this study was conducted in Sweden, presumably (although not specified) using a translated version of the HS. The impact of this translation process on the interpretation of HS items and subsequent results is unknown.
In sum, of the 10 studies analyzing the factor structure of the HS in clinical samples, 7 have utilized “exploratory” methods (principal components analysis). Of these 10 studies, 5 have concluded that a three-factor model provided the best fit and 2 more could be described as partially supportive of this model (Mendonca et al., 1983; Steer & Beck, 1997). Of the studies that have not supported Beck's original three-factor model, one used a sample size too small to be considered reliable (Nekanda-Trepka et al., 1983). Thus, only two large-scale studies of using a clinical sample can be characterized as inconsistent with the three-factor solution (Young et al., 1992; Aish & Wasserman, 2001) and one of these two (Aish & Wasserman, 2001) utilized a translation of the HS into Swedish, potentially altering the meaning and interpretation of some items. Although hardly definitive, these 10 studies appear to support Beck's original conclusion that a three-factor model provided the best fit to HS data in clinical populations. Moreover, despite some differences in the composition of these three factors, the labels offered by each author have been largely similar, with the first factor being focused on hope for the future, the second factor targeting motivation to try to achieve goals, and the third focused on future expectations.
In addition to the 10 studies that analyzed the factor structure of the Beck HS in clinical samples, a number of researchers have studied the HS in “normal” populations. Several of these studies have relied on samples of college students, and have typically concluded that a one-factor model provided the best fit (e.g., Ward & Thomas, 1985; Chang et al., 1994; Steed, 2001). Of these studies, only one attempted to systematically compare alternative factor models (Steed, 2001). Using a principal axis factor analysis with oblique rotation, Steed found that a four-factor model provided the best fit to his data (using more than 500 college students) but noted that this model was largely uninterpretable. Because the first factor accounted for the lion's share of the variance, he concluded that a one-factor model was more appropriate. However, a subsequent confirmatory factor analysis of his data comparing several alternative one- and two-factor models indicated that none of the models tested adequately fit his data, leading Steed to conclude that the HS may have limited utility in “normal populations.”
Interestingly, two studies of adult samples have generated somewhat different results than the studies of college students. Marshall et al. (1992) used a principal axis factor method and a varimax rotation to analyze data from two samples of male navy recruits. Their analyses (based on a modified version of the HS in which the true–false response format was replaced with a 5-point Likert-type scale), yielded a three-factor solution for each sample although the authors noted that examination of the scree plot was more supportive of a two-factor solution and the presence of a single, overpowering factor suggested a one-factor solution. Despite these conflicting findings, they chose to interpret the two-factor solution which, like many other factor analysis solutions, appeared to be heavily influenced by item wording. The first factor, labeled Pessimism, contained eight negatively worded items and Factor 2, labeled Optimism, contained seven positively worded items (five items were excluded based on their poor fit with the chosen factor structure).
Tanaka et al. (1988) investigated the structure of hopelessness in a community sample of 154 Japanese adults using a Japanese translation of the HS. They extracted two factors from their principal components analysis, one corresponding to optimism and another to pessimism, although these factors bore virtually no resemblance to those derived by Marshall et al. (1992). Further, despite commonsense assumptions that these terms reflect opposite poles of the same construct, the two factors were only correlated 0.28 in their sample (after rotation).
In sum, although no clear consensus is apparent, studies of nonclinical samples have supported both one-factor and two-factor models, with little support for the three-factor models that have emerged in studies of clinical populations. Moreover, in one of the most sophisticated analyses to date, Steed (2001) suggested that the HS may simply be uninterpretable in “normal” populations. Thus, both the factor structure and utility of the HS in nonclinical populations is simply unknown.
In the context of this literature, we chose to assess the meaning and structure of hopelessness in patients with AIDS. As discussed above, hopelessness may have a unique meaning for patients with advanced medical illness. Although one might posit that medically ill individuals would interpret the Hopelessness Scale similarly to psychiatric patients (given the relatively high rate of depression and past or current substance abuse in patients with AIDS), where three-factor models have generally prevailed, other possibilities clearly exist. Because medically ill individuals do not necessarily suffer from any particular psychological symptoms (e.g., cognitive distortions) or psychiatric disorder (e.g., depression), their interpretation of the HS might more closely reflect the one- or two-factor models that have emerged from studies of nonclinical samples. Alternatively, the HS may have an altogether different structure in the context of severe medical illness, because these individuals might interpret the various HS items in a unique manner. Because our goal was to compare the adequacy of the various models previously described, we utilized a confirmatory factor analytic approach to these data, hypothesizing that the three-factor model would provide the best fit for our data set. In addition, we analyzed data from two separate samples of patients with advanced HIV/AIDS, including data collected before and after the development of highly active antiretroviral therapies (HAART) to assess the extent to which HS responses differ among samples with a somewhat different prognosis. Finally, we analyzed the correlations between the resulting factors of hopelessness and other, potentially relevant variables (e.g., depression, desire for hastened death, suicidal ideation, social support) to better understand the differences among these factors.
The data were drawn from two sources: a study of pain and psychological functioning in ambulatory patients with AIDS conducted between December 1992 and March 1995, and an ongoing study of depression and desire for hastened death among hospitalized patients with advanced AIDS (data was collected between February 1998 and February 2000).
Of 479 subjects who participated in Study 1 (described in detail in Breitbart et al., 1996), 63.9% were male, the average age was 38.8 years (range: 18–69), and they reported an average of 13.0 years of education completed. Racial breakdown of this sample was roughly evenly divided between Caucasian (38%), black (37%), and Hispanic (23%), with 2% classified as “other” (largely Asian). The majority of the sample had contracted the HIV virus through injection drug use (53%), with 28% reporting homosexual contact as the risk transmission factor and 19% reporting heterosexual contact as the source of infection. The majority of subjects studied (72%) had experienced at least one opportunistic infection and most had CD4+ cell counts below 200 (65%).
Participants in the second study (N = 198) were also predominantly male (79%), with an average age of 44.4 (range: 24–75) and an average of 12.7 years of education. This sample was predominantly of minority ethnic background, with 55% black, 19% Hispanic, 5% Asian, and 21% Caucasian. Injection drug use was again the most common form of risk transmission behavior, with 61% reporting drug use as the likely source of infection. Heterosexual contact was reported by 12% of the sample and 18% reported homosexual contact (9% reported either multiple or unknown sources of HIV infection). The majority of subjects (69%) had a history of at least one opportunistic infection and 71% had current CD4+ cell counts below 200 (41% had CD4+ cell counts below 50 at the time of study participation). Roughly one-fifth (20.2%) of the sample met criteria for a major depressive disorder based on SCID (First et al., 1994) interviews.
All participants completed the HS (Beck et al., 1974) as part of an extensive battery of self-report and clinician-rated instruments assessing potentially relevant influences such as physical symptoms, psychological well-being, and social support. The various measures included the Beck Depression Inventory (BDI; Beck et al., 1961; used in Study 1) or the Hamilton Depression Rating Scale (HDRS; Hamilton, 1960, used in Study 2), the Schedule of Attitudes Toward Hastened Death (SAHD; Rosenfeld et al., 1999, used in Study 2), the FACIT Spiritual Well-Being Scale (SWB; Brady et al., 1999, used in Study 2), the McGill Quality of Life Questionnaire (MQOL; Cohen et al., 1995; used in Study 2), the Memorial Symptom Assessment Scale (MSAS, Portenoy et al., 1994, used in Studies 1 and 2), and the Karnofsky Performance Rating Scale (KPRS; Karnofsky & Burchenal, 1949, used in Studies 1 and 2). The studies in which these data were derived were approved by the Institutional Review Boards of all participating hospitals. All subjects provided written informed consent prior to participation.
Data were analyzed using LISREL 8.30 (Jöreskog & Sörbom, 1993), comparing the model fit statistics for each of the models identified in previous research (because no clear consensus emerged in the previous research, a comparison of “nested” models appeared less informative). Model comparisons were based on several goodness-of-fit indices, including the chi-square test, the root mean square error of approximation (RMSEA), and the expected cross-validation index (ECVI). Because these indices generated largely complementary results, only RMSEA statistics are reported here. Further, because the possibility that differences in the nature of HIV/AIDS (i.e., available treatments, illness chronicity) might influence the perceived “hopelessness” of this illness, and these differences might influence the very structure of HS responses (rather than just the absolute number of items endorsed), we analyzed data from the two studies separately. Following an analysis of the data from Study 1, we examined the modification indices to determine whether, using a more exploratory approach, any alterations to the model would significantly improve the overall fit to these data. Although such an analysis is more exploratory in nature, it allows for the possibility that a model that deviates slightly from the existing models might substantially improve the overall model fit for these data. The resulting “best fit” model was then included among the model comparisons used for the confirmatory analysis of Study 2 data. Finally, because both analyses ultimately generated the same best fit model, we combined data from both studies for correlational analyses designed to help understand and characterize the resulting factor structure.
A comparison of the alternative factor analysis models demonstrated considerable superiority of the three-factor models over the one-, two-, four- and five-factor models previously published (see Table 3). The various three-factor models generated RMSEA estimates ranging from 0.052 to 0.076 (with one exception) for the first data set and 0.066 to 0.082 for the second. Of note, other fit indices yielded highly similar results but are not reported here to minimize redundancy. The one-, two-, four- and five-factor models, on the other hand, were considerably worse, all generating RMSEA statistics greater than virtually all of the three-factor models. Moreover, the 95% confidence intervals for both the RMSEA and ECVI showed little overlap with confidence intervals for the two-factor models.
Fit indices for Beck HS factor models

However, despite the apparent superiority of the three-factor models over other factor structures tested, none of these models generated an adequate fit to our data set based on accepted criteria (i.e., RMSEA below 0.05). Indeed, the best-fitting model was the three-factor model proposed by Hill et al. (1988), generating an RMSEA of 0.052 for the Study 1 data and 0.066 for Study 2 data. Because this model fit was less than ideal, we analyzed the residuals from this model in hopes of generating a somewhat better fitting model for our data set. The resulting three-factor model (referred to as the “best fit” model in Tables 2 and 3) provided an adequate fit for the data (Study 1 RMSEA = 0.048 and Study 2 RMSEA = 0.051; combined data set RMSEA = 0.046).
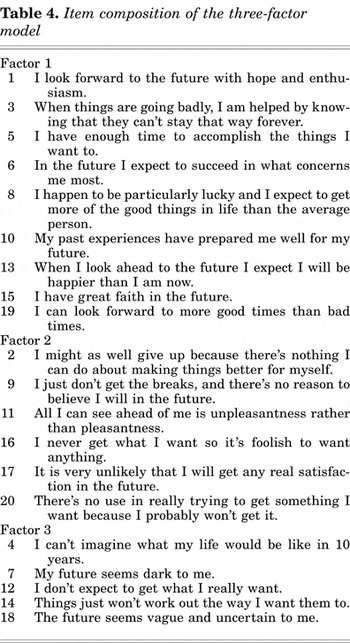
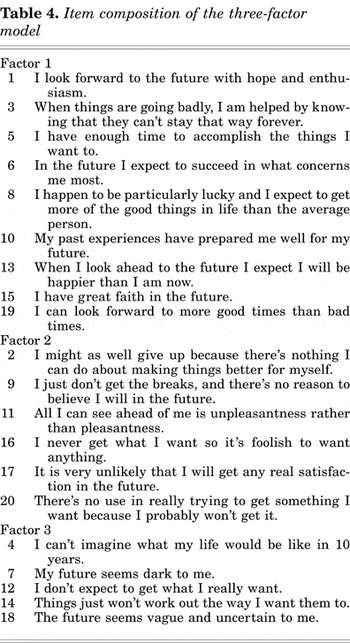
The “best fit” three-factor model incorporated the core elements of each of the three-factor models previously published, but with minor modifications (see Table 4). As with most previous studies identifying a three-factor model, the first factor was comprised of items 1, 6, 13, 15, and 19, as well as items 5, 8, and 10 (all of which have been included in this factor in at least some of the previous studies). Factor 2 also contained a core of items that have been identified in previous research, specifically items 2, 9, 16, 17, and 20. The third factor contained items 4, 7, 11, 12, 14, and 18, again reflecting a core of items that have been identified in several studies (e.g., items 4, 7, 12, 14, and 18) although the composition of this factor has been somewhat less stable in the studies reviewed.
Item composition of the three-factor model
Correlational analyses were used to analyze the pattern of correlations between the three factors of the HS (the number of items endorsed in the “critical direction” on each factor) and the various other measures administered concurrently. Not surprisingly, measures of depression (the BDI and HDRS), spiritual well-being (the FACIT), and suicidal ideation/desire for hastened death were the strongest correlates of all three HS factors (see Table 5). However, several noteworthy discrepancies emerged within the pattern of correlations. For example, gender and race were both significantly associated with Factor 1 scores (with men and non-Whites obtaining lower scores on this factor) but were not related to Factors 2 or 3. Number of physical symptoms was also strongly associated with Factor 1 scores, but much less so with Factors 2 and 3, whereas pain intensity was more highly correlated with Factor 2 (although this correlation was quite modest).
Correlations with the HS factors

An analysis of the correlations within each factor revealed that spiritual well-being was the strongest correlate of Factor 1 scores (r = −0.56) and this correlation was substantially larger than with Factors 2 or 3 (r = −0.35 and −0.47, respectively). Factor 3, on the other hand, was most strongly associated with scores on the Beck Depression Inventory (r = 0.61) and the Schedule of Attitudes Toward Hastened Death (r = 0.59; a measure of desire for hastened death), and these correlations were somewhat higher with Factor 3 than the other two factors (although scores on the BDI and SAHD were also the strongest correlates of Factor 2 scores). Thus, although one might be tempted to conclude that Factors 2 and 3 are largely similar, inspection of Table 5 reveals that the distress-related variables were much more strongly associated with Factor 3.
Understanding the construct of hopelessness is complicated considerably by the presence of a severe or terminal medical illness. We sought to study the structure of hopelessness, using the Beck Hopelessness Scale, in two samples of patients with advanced HIV/AIDS, one recruited prior to the emergence of the “newer” antiviral combination therapies and a second recruited more recently. Using a confirmatory factor analytic method to compare alternative models, data from these two samples strongly supported the same three-factor model that has been commonly observed in clinical/psychiatric samples. This three-factor model of hopelessness has significant implications for understanding the attitudes and perceptions of individuals with advanced or terminal illness.
The first and strongest factor observed in our sample (and previous studies of the Hopelessness Scale) contained all nine of the positively worded items. These items reflect a positive future orientation (e.g., “I look forward to the future with hope and enthusiasm”), and has been given labels such as “expectations for success,” “hopefulness about the future,” “feelings about the future,” and simply “optimism” in the various published studies. The second factor, which contained 6 of the 11 negatively worded items, reflects the tendency to not attempt to change one's situation (“I might as well give up because I can't make things better for myself”). This factor, which has been described as the “motivational” factor by Beck, has also been labeled “giving up” and “expectations of failure” among others. The third factor, which contained the remaining five negatively worded items, reflects a generally pessimistic outlook on the future (e.g., “All I can see ahead of me is unpleasantness rather than pleasantness”). This factor has been labeled “future expectations,” “future uncertainty,” and “future anticipation” in various published studies.
The observation that, in the context of a life-threatening illness, the negatively worded items form two distinct factors, as has been observed in most clinical samples (to a greater or lesser extent), suggests that “pessimism” may become a multidimensional construct for some populations. Although similar findings have been observed in samples of depressed and suicidal individuals, separating one's expectation that the future will hold nothing but unpleasantness from the sense that one has no control over the future may be a particularly important distinction for medically and terminally ill individuals, as these different aspects of one's future orientation may lead to different perceptions, attitudes, and decisions. For example, it may be possible to maintain a positive outlook on life (e.g., the Factor 1 items) while nevertheless accepting one's inability to control his or her destiny (i.e., Factor 2). Such distinctions may lead to different beliefs, attitudes, and treatment decisions in medically ill individuals, such as decisions to forgo life-sustaining interventions or seek a hastened death. Particularly given the growing focus on hopelessness as an integral component to end-of-life decision making, attention to the various aspects of hopelessness may yield important information for these crucial policy questions.
However, the similarities between our “best fit” model and the previous factor models derived from clinical samples begs the question as to whether patients with HIV/AIDS, because of the high rate of depression, substance abuse, and suicidal ideation, are not simply another “clinical” sample. Although no clear answer exists to this question, the frequency of major depressive disorders (roughly 20%) in the second data set suggests that a characterization of this sample as “depressed” is probably not warranted. On the other hand, more than half of our samples (from both data sets) had either a history of or active substance abuse disorders, making them much more comparable to the sample described by Steer et al. (1994). Hence, the extent to which our findings reflect the influence of advanced illness rather than comorbid psychiatric disorders is unclear. However, the similarity of the factor structure for both data sets (before and after the emergence of multidrug regimens) suggests that responses to the HS may not have been primarily responsive to the individual's actual prognosis.
It should be noted that this confirmatory factor analysis was intended to assess the structure of hopelessness in the context of severe medical illness rather than provide a “definitive” analysis of hopelessness more generally. We cannot ascertain whether these findings would generalize to other populations or even other samples of medically or terminally ill individuals (e.g., patients with cancer, diabetes, or other terminal illnesses). In response to an earlier review, Steed (2001) concluded that HS may be uninterpretable in “normals” but acknowledged that three-factor models have been the norm in clinical samples. Our findings support the latter conclusion. But given that the construct of hopelessness is particularly relevant in the context of both psychiatric and medical illness, the absence of a clear (or even valid) interpretation of HS scores in college students or other healthy populations is not necessarily troubling. Instead, researchers using the HS in clinical samples should attend to the different elements of hopelessness that have consistently emerged in this and previous factor analytic studies.
The evidence suggesting that the third factor, tapping a generally pessimistic outlook toward the future, was the most highly associated with desire for hastened death and depression was unexpected. We anticipated, based on both the results of Hill et al. (1988) as well as item content, that Factor 2 (“feelings of giving up”) would be the strongest correlate of suicidal ideation and desire for hastened death in our study. Although this factor might intuitively seem to be the most salient element in driving a patient's desire to die, we found that a more general “pessimism” factor was a stronger predictor. In fact, this finding is consistent with the results of a study of “trait” versus “state” pessimism, with the former being significantly associated with suicidal ideation whereas the latter was not (Young et al., 1996). Hence, it may be that decisions to hastened death or contemplate suicide in the context of a terminal illness are rooted in a more chronic type of “hopelessness” analogous to general pessimism rather than a more transient or situational form of hopelessness. Of course, any conclusions based upon the pattern of correlations should be considered tentative, as the magnitude of the differences across the three factors was usually quite modest and may have, at times, reflected chance variation.
Regardless of whether our findings would be replicable in other terminally ill samples, or reflect a finding unique to patients with HIV/AIDS, these data have important ramifications for the study of patients with a terminal illness. The possibility that hopelessness might require a more detailed analysis than has typically occurred, where simple summary scores have been the norm, is clear. Studies of end-of-life issues might achieve their aims using an abbreviated hopelessness scale, perhaps assessing only the most relevant portions (e.g., one factor) of this multidimensional construct. Alternatively, understanding the complex end-of-life issues might benefit from exploring the different elements of hopelessness and their unique correlates among different patient populations (e.g., patients with cancer, amyotrophic lateral sclerosis). Although this study represents the first step in developing a more thorough understanding of the interaction between hopelessness and terminal illness, further research will no doubt help to elucidate these complex relationships.
This research was supported by grants from The American Foundation for Suicide Prevention (B. Rosenfeld, P.I.), and The National Institute of Mental Health Grant #RO1MH 57629 (W. Breitbart, P.I.).

Factor analytic studies of the Beck Hopelessness Scale

Item composition of factor analysis models

Fit indices for Beck HS factor models
Item composition of the three-factor model

Correlations with the HS factors