Introduction
In many respects, Israel serves as a case study for understanding the obstacles and challenges in developing palliative care (PC). Israel's public healthcare system, despite of few evident stressors, holds a high ranking (8.8 out of 10) among the OECD countries (Hadad et al., Reference Hadad, Hadad and Simon-Tuval2013; Even, Reference Even2018). The country belongs to upper-income countries with a high living standard, access to education, and low infant mortality rates (Baider and Goldzweig, Reference Baider, Goldzweig and Silbermann2016). At the same time, the Israeli society can be described as an amalgamation of cultures, religions, and people of different origins, including Jewish immigrants from many countries, Muslim Arabs, Christian Arabs, Druze, and Bedouin many of which with traditional cultural values (Baider and Goldzweig, Reference Baider, Goldzweig and Silbermann2016). Providing and teaching PC in such cultural melting pot evidently calls for special attention to cultural safety in PC, which has also been acknowledged (Gamondi et al., Reference Gamondi, Larkin and Payne2013; Würth et al., Reference Würth, Langewitz and Reiter-Theil2018). Yet, finding the balance of power between professional caregivers and the people receiving care still needs better conceptualization (Curtis et al., Reference Curtis, Jones and Tipene-Leach2019) and improvements in PC implementation and education.
In 2009, PC was added to “the health basket,” a predefined list of health services. Accordingly, all Israeli citizens are entitled to free PC when needed (Ministry of Health, 2009; Bentur et al., Reference Bentur, Emanuel and Cherney2012). The policy stated that by 2013, all healthcare facilities have to provide PC services of the highest quality in terms of minimum standards, scope, and tasks of a PC team. The Health Maintenance Organizations were declared responsible for training the health and social care professionals (Ami and Yaffe, Reference Ami and Yaffe2015). As a result, a continuing education program INPACT was introduced (Shvartzman et al., Reference Shvartzman, Singer and Bentur2011). This program targeted existing PC teams. In 2010, pain management was officially acknowledged as a medical specialty followed by PC in 2013. Today, there are about 30 recognized PC specialists in Israel (Rosen et al., Reference Rosen, Waitzberg and Merkur2015; Arias-Casais et al., Reference Arias-Casais, Garralda and Rhee2019), and the number is growing.
The quality of PC development, however, cannot be solely assessed from a specialized provision perspective (Arias-Casais et al., Reference Arias-Casais, Garralda and Sánchez-Cárdenas2021). Despite sufficient access to pain medication, available policy, and advantages in specialist education, PC services in Israel are still mainly provided to cancer patients (Shaulov et al., Reference Shaulov, Baddarni and Cherny2019). PC integration into pediatrics, long-term care facilities, primary care, cardiology, and neurology are still to be addressed (Arias-Casais et al., Reference Arias-Casais, Garralda and Sánchez-Cárdenas2021).
For preliminary and advanced integration of PC, the existence of a recognized medical specialty in PC and the inclusion of PC education at the undergraduate level in the medicine and nursing curricula are of great importance (Baur et al., Reference Baur, Centeno and Garralda2019). To expand the provision of PC and increase the access, the core principles and the practice of PC need to be integrated in all undergraduate education and formative training programs (Paal et al., Reference Paal, Brandstötter and Lorenzl2019; Mason et al., Reference Mason, Paal and Elsner2020a; Martins Pereira et al., Reference Martins Pereira, Hernández-Marrero and Pasman2021). In the European region, the lack of basic training in PC with a particular emphasis on the absence of PC teaching at the undergraduate level is still the most frequently mentioned barrier (Centeno et al., Reference Centeno, Garralda and Carrasco2017). Hence, exploring PC education at the undergraduate level at medical schools in Israel may help to identify hindrances relevant not only at an individual country level but also worldwide. Even if the situation at Israeli medical schools is changing rapidly (Reis et al., Reference Reis, Glick and Urkin2017), some remaining obstacles need to be discussed recurrently. This article presents the findings collected from all medical schools that are under the regulation of the Israeli Council of higher education.
Aim
This qualitative study explored and described the current state of PC education at the undergraduate level at medical schools in Israel. The following questions were addressed:
• How is PC undergraduate education implemented in medical schools?
• What are the objectives, obstacles, and challenges in PC undergraduate education perceived by Israeli medical faculty?
Methods
This is a qualitative study supported by a survey and semi-structured expert interviews. The theoretical sampling in ethnographical studies is difficult, and thus we opted for purposive expert sampling (Etikan and Bala, Reference Etikan and Bala2017). The anticipation is that experts have special knowledge and specific functions close to societal ascription (Bogner et al., Reference Bogner, Littig and Menz2009). The expert interviews are expected to provide knowledge resulting from the actions, responsibilities, and obligations of their specific role. Hence, the selected approach is helpful to explore and describe the current state of PC education at the undergraduate level at medical schools in Israel. However, the recruited experts represent a variety of standpoints depending on their role, and daily challenges as physicians or faculty members.
Before entering the field, we surveyed all five medical schools in Israel. The survey has been tested and used in the Pan-European study regarding postgraduate PC education to gain internationally comparable as well as country-specific data (Stähli et al., Reference Stähli, Stiel and Paal2020). The survey included questions on (1) background information of the respondent, (2) voluntary and obligatory courses on PC, (3) PC content in different course models, (4) teaching methods, (5) time frame, (6) content, (7) institutions involved, (8) and examinations. One key faculty member filled out the survey.
An interview guideline (Appendix) was developed and validated by conducting four test interviews. The questions were open and text-generating. It enabled an exploratory approach providing a basis for subsequent qualitative evaluation (Lamnek and Krell, Reference Lamnek and Krell2010, p. 314 ff.; Wittkowski, Reference Wittkowski2013). With permission, the interviews were audio-recorded. All interviews were conducted in English in a quiet environment from November 2017 to February 2018. The interviewer took field notes to enable better understanding and interpretation of the data. Participants could stop the interview at any time. Each interviewee received an Informed Content Sheet providing written information about the study, benefits, risks, and data protection. The ethics committee of the RWTH Aachen University approved the study (EK 182-17). All participants committed themselves to confidentiality (§40, German Federal Data Protection Act).
The interviews conducted in English were stored and evaluated anonymously with codes. We transcribed and edited the interviews using the FT4 transcript software. We followed the simple transcription system of Dresing and Pehl (Reference Dresing and Pehl2015). The statements and results based on the material were generated without defining predefined hypotheses (Kuper et al., Reference Kuper, Reeves and Levinson2008; Mayring, Reference Mayring2015). The analysis was conducted in the following substeps: (Z1) Paraphrasing; (Z2) Generalization to the level of abstraction; (Z3) First reduction by one investigator; and (Z4) Second reduction, where all authors collaborated until categories were finalized (Vaismoradi et al., Reference Vaismoradi, Turunen and Bondas2016). The main findings are presented as a synthesis of the interviewees’ thoughts and ideas with respective direct quotations or references to verbatim.
Results
Participants of the survey
One faculty member of each medical school (N = 5) filled out the survey. At the time of the interviews, they were working at the Departments of Hematooncology, Geriatrics, or Family Medicine. All respondents were in charge of teaching PC.
Results of the survey
Haifa and Tel Aviv universities have established mandatory PC courses. In Safed, PC is an integrated part of other disciplines. Medical schools in Jerusalem and Be'er Sheva do not have PC in their medical curriculum as yet. All medical schools provided contact with patients with PC needs during the rotation internships. The results are summarized in Table 1, where we have outlined the types of medical programs at each university (Reis et al., Reference Reis, Glick and Urkin2017) and listed mandatory and elective courses, indicating the extent and content of PC-related teaching.
Table 1. PC in medical curriculum at Israeli Medical Schools
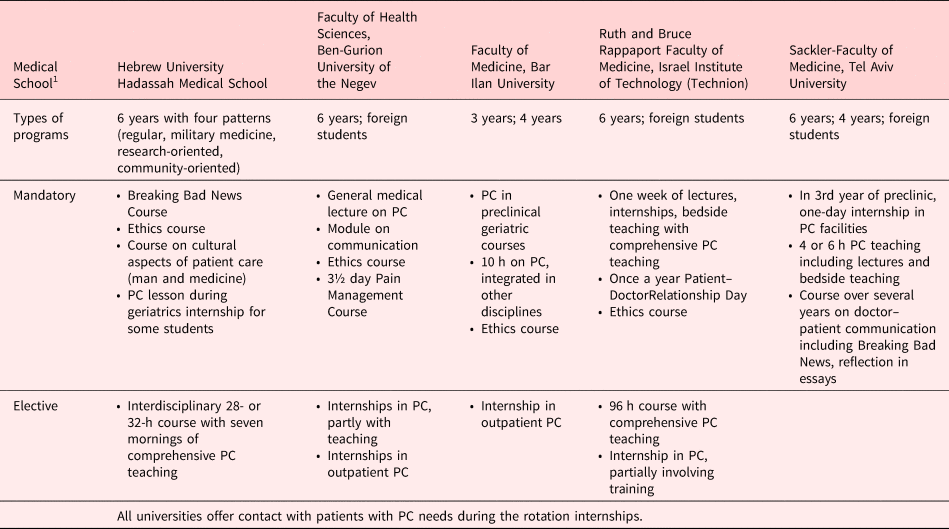
1All five medical schools have reviewed their curricula and modernized their educational frameworks; however, they have all retained an emphasis on lectures and examinations based on multiple-choice-type questions. A slow increase in small-group-based learning and an innovative approach to pedagogy and teaching have been accompanied by highly heterogeneous training in clinical skills instruction and assessment (Reis et al., Reference Reis, Glick and Urkin2017).
Semi-structured interviews: demographic data
We conducted three interviews at The Hebrew University and two at Ben-Gurion University, Bar-Ilan University, The Technion, Tel Aviv University. Eleven faculty members (ten physicians, one social worker) participated in this study. All but one participant had frequent contact with patients receiving PC. Seven worked in PC wards. There were four PC specialists among the respondents. Six had completed a fellowship or specialist training in PC abroad. All interviewed faculty members were involved in PC teaching of undergraduate medical students or PC training during clinical internships.
Results of interviews
The analysis of the interviews resulted in a coding-tree consisting of 1,838 codes. This paper focusses on three main categories relating to undergraduate teaching at medical schools: (1) PC education today; (2) obstacles related to PC education; and (3) recommendations to improve PC education. An overview of main themes and their subthemes is presented in Figure 1.
(1) PC education today

Fig. 1. Overview of the three categories and their subthemes.
PC teaching has no central organization. Palliative medicine is not a mandatory subject and not an accreditation criterion. Teaching differs greatly depending on the hospital, ward, and lecturer. Often, PC is included in internal medicine or oncology. Depending on the university, PC may be also integrated into geriatrics, ethics, family medicine, or surgery.
Timing
Since dealing with dying people requires maturity, confrontation with PC during very early stages of studies could be perilous. Hence, PC teaching has to be well timed. Some faculties introduce PC during in-home-hospice visits. At the University of Bar-Ilan, for example, PC is introduced in the geriatrics courses. At Tel Aviv, students have a one-day internship in PC called “Preclinical exposure”:
“And then we schedule them to go for a one-day-experience. Since then, they are divided. Some are going to a hospice. They spend one day in a hospice. And others are going to an in-home-hospice. We have those services in the country. (…) So, each one has to join a physician or a nurse, who is giving PC for one-day work. And if they go to the hospice, it's in groups of eight. If they go to a home, it's one. It's only one student with the team. And they have to go there. They have to interview a dying patient or the family of the patient. (Coughs) So they have to be there the whole day.” (A5T11, par. 24-26)
At all medical schools, students are exposed to PC during their clinical rotation internships. Participants assumed that students on internal medicine wards would meet dying patients. Students even have the opportunity to accompany physicians during PC consultations. Teaching activities during the visitations, however, remained unclear.
Communication
Communication, including breaking bad news, is one of the main foci of teaching. Courses on communication, in particular on breaking bad news, are included in the curricula. Students have to understand that the interpretation of what is bad news depends on the patient (A5T11, par. 10). They should also learn to ask specific questions to gain a holistic understanding of patients’ views and wishes related to treatment options (O4T10, par. 66). Competencies in dealing with conflicts should also be a focus. Students should learn strategies for how to deal with collusion, taboos, and disclosure (O5J01, par. 41).
Teaching methods
Lectures and presentations were considered a common PC teaching method, which some of the interviewees did not consider particularly effective (O6B06, par. 39). They described seminars and small group learning much more useful (D3J02, par. 136). Lecturers from Tel Aviv reported a big interactivity in small groups (A5T11, par. 26). Students were required to write reports on their impressions of the clinic, which were later discussed in the group. Case studies were also presented and discussed (A5T11, par. 35). Students were allowed to choose discussion topics to process what was bothering them. The elective course in Jerusalem also provides many small group activities (O5J01, par. 37). There, the inter-professional exchange with nursing and social work participants is both, method and learning objective. Furthermore, it was often emphasized that the students’ encounter with patients, families, and caregivers was an important form of learning (O5J01, par. 47).
Written assignments and interactive online modules were considered methods to enable learning about PC outside clinical environments and universities (O5J01, par. 39). Reading literature about end-of-life and in-depth analysis of short stories constituted theoretical forms of learning (O5J01, par. 41).
At universities, physicians typically provide the PC lectures. However, other professionals, such as psychologists, social workers, nurses, chaplains, lawyers, politicians, and even writers or poets, take part in the teaching (E4H09, par. 19).
Content
Lecturers from various universities emphasized the importance of teaching students at least basic PC concepts:
“What is PC, what are the goals, and what are the services in this country?” (A5T11, par. 12)
Students should recognize the role of the family as caregivers as well as people in need (A5S04, par. 30).
Another very important topic in teaching is the quality of life regarding the symptom and pain management (O4T10, par. 10). Practical skills, such as physical examination, medical history, and profound knowledge about complex and chronic illnesses, are considered paramount (O4T10, par. 10). Specific learning contents, such as nutrition at the end of life, were also mentioned (I5H08, par. 22).
Furthermore, medical students should know about the history and the current state of PC in Israel and worldwide (O4T10, par. 10). They are taught about legislation, especially the Dying Patient Law (accepted in 2005), living wills, and advance care planning (M5S05, par. 10). Ethics was mentioned as a curricular issue (M5S05, par. 10). Students have to understand and respect cultural and religious traditions regarding the end of life (O5J01, par. 29). They should also understand that spirituality means more than religion. For example, literature or art may serve as a form of spiritual expression for some patients (O5J01, par. 45).
Personal contact with dying people is an important aspect of the training of young doctors. Respect and professionalism were keywords mentioned to characterize this (D3J02, par. 134). They should understand the importance of reflecting on their feelings throughout their professional and personal lives (O5J01, par. 154).
Student's preparedness
Interviewees agree that medical students should obtain PC competencies since they will treat patients in need of PC. Often, students experience death and dying during military service or within the family (A5S04, par. 36). Some, however, would have their first encounter with death during studies. The introduction to the end of life and dying needs to be gradual (A5T11, par. 28). Finding a way into PC philosophy and thinking takes time.
The lecturers were ambivalent when asked to evaluate the effectiveness of PC teaching. Medical students seem familiar with basic concepts of PC, but their preparedness to deal with terminally ill patients is limited.
“They know what PC is all about. Can they provide it by themselves? I'm not so sure.” (M5S05, par. 12)
Medical students understand the importance of PC, know that PC teams are established on the wards, and know where to get professional support. They can manage pain. Then again, some interviewees suggested that students were not well prepared as becoming a good PC physician would require years of experience:
“Well prepared is not the right word. It's (..) something that you need in the years of experience, okay? (.) It's not something that right away. And your position in life is matter in PC.” (I5H08, par. 26)
Hence, medical students should have more opportunities to accompany their patients at the end of life in order to develop an experience-based attitude towards PC.
Requirements to PC teachers
A teacher needs to have a good relationship with students requiring respect and demonstrating attention to their needs. Discussion and communication are of the essence. A good teacher–student relationship may motivate teachers in their work. One lecturer noted that the relationship with the student changes with increasing age from friendly discussions to ones filled with respect (O5J01, par. 152). The teacher's main task is to convey enthusiasm for PC. Focusing on relevant topics and teaching attitude and practical skills are priority tasks to make good people, rather than just good doctors (M5S05, par. 76).
Gaining practical experiences
Most PC training for physicians is postgraduate training. There are courses for specialist PC physicians and various specialist training programs.
“And it's not incidental that all over the world is a fellowship, it's not a residency. You have to be either an internal medicine doctor or paediatric or family medicine doctor. You have to have the basic of something. (…) So, and I think that it also tells you something about the right time to give education. I think that in professions that you cannot require the profession before you're a resident. It's too early to teach you (.) that profession (…) while you are like in medical school.” (A5T11, par. 51)
Support for students
Potential support offers to students and residents in coping with death and dying vary. According to lecturers, mutual support in the team and among students is highly important. Even if the awareness of difficulties in dealing with dying people is growing, the lack of support was acknowledged. Whereas, some interviewees indicated the lack of opportunities for discussing these sensitive topics (O5J01, par. 158), others justified it by emphasizing the lack of patient contacts. One respondent argued that students are less exposed and have less responsibility, and therefore, their need for support is reduced compared to the attending physician (D3J02, par. 150).
Interviewees from the Tel Aviv University repeatedly said that students would know how to get help (A5T11, par. 121). An attempt to create a network of support among students is ongoing (A5T11, par. 117). Tutors are available for personal discussions. If necessary, the tutors would ask PC lecturers, psychologists, or Balint groups for further help (O4T10, par. 38).
Within the hospital PC team, its members often support themselves, which is part of PC philosophy. Mutual support, however, varies from hospital to hospital. Some PC units have discussion and self-reflection opportunities for all employees. At Jerusalem and Be'er Sheva, there are regular meetings with debriefings (O6B06, par. 143-145). Students on the ward are also encouraged to participate and talk about their thoughts and feelings.
-
(2) Obstacles related to PC education
Identifying the obstacles to PC education helps to identify areas for improvement. The most commonly cited barrier to good PC teaching is the missing mandatory status of PC. Organizational structures at medical schools would make it difficult to establish a new subject. Additionally, there is a lack of time and human resources.
Missing mandatory status of PC
Since PC is not mandatory, teaching depends on the personal interest of lecturers.
“There all is, it is inconsistent. You know, because there is not a national curriculum. It is not considered a core element of medical education. So, it's not an accreditation criterion for the medical schools.” (A5J03, par. 29)
Teaching varies greatly between medical schools, and not all students can learn about PC. PC is not an independent mandatory subject. As a result, PC teaching suffers (A5J03, par. 17).
Difficult to establish a new subject
To introduce a new content at medical school, existing curriculum has to be amended. Establishing new courses at universities is challenging (O6B06, par. 39). Organizational and academic efforts to offer new mandatory internships are high (A5T11, par. 47). Furthermore, medical students already feel overwhelmed by information overload (A5T11, par. 51).
Lack of resources and personnel
Lack of time, personnel, and suitable training wards were mentioned as further obstacles to expand PC teaching. Lecturers expected to teach do not have enough time at hand. One lecturer described it as follows:
“So, it's kind of hard to have learners come in, when I don't have the time or the ability to take them around.” (D3J02, par. 26)
Another problem is the lack of lecturers with sufficient experience in PC. The “manpower infrastructure” (A5J03 par. 116), in particular, has to be improved and a sufficient number of lecturers with good PC skills is needed.
Some physicians working at medical schools are described as poor role models by suppressing the topic of death and dying. Interviewees mentioned that young doctors who had studied outside Israel have been rarely taught to communication skills. Students from Eastern European universities have rarely learned to deliver bad news (A5S04, par. 72-78). Young doctors from universities in the surrounding Arab countries, on the other hand, are often less aware of patient rights and not used to listening to patients (A5S04, par. 80).
-
(3) Recommendations to improve PC education
Medical schools should cooperate to learn from each other. Ideally, similar teaching should take place in all medical schools and teaching hospitals. A formation of expertise exchange across medical schools would automatically lead to more courses, jobs, grants, and research. In any case, decisions on the further development of teaching need to be enforced at the national level:
“I think that we need to change things nationally.” (O4T10, par. 132)
Make elective PC courses mandatory
To improve PC teaching, PC has to become a mandatory subject. All medical schools should include PC in their curricula, communicate PC values, and foster a holistic approach to all future physicians. Additionally, longitudinal curricular integration of PC would be desirable (O6B06, par. 37-39). It would be beneficial to include PC aspects to all disease-specific teachings (M5S05, par. 88). PC should be recognized as an independent subject with an equal academic and educational status to other medical subjects (O4T10, par. 44).
Internships and hybrid courses
Structured internships, as well as hybrid courses, are seen as trend-setting (E6B07, par. 18). Hybrid courses combine modules at the university with online modules. Suitable video clips have been recorded in Jerusalem and made available on an interactive learning platform (O5J01, par. 55).
Integration of PC across the healthcare-related education
All other professions in healthcare should also be required to integrate PC teaching into their curricula:
“It should be an integral part of ANY health care education, whether it's physicians, nurses, social workers, psychologists, (.) whatever.” (M5S05, par. 86)
All specialist training courses should include further PC training for physicians who are already licensed, especially general practitioners working closely with outpatient PC services. The expansion of further training program for PC physicians should also be considered.
Discussion
PC education in Israel is shifting. There are several factors, which suggest a positive development in the future. Throughout Europe, PC is introduced to undergraduate medical education (Arias-Casais et al., Reference Arias-Casais, Garralda and Rhee2019). The medical faculty described how the number of PC specialists in Israel is increasing and how teaching PC for medical student is improving. A clear change regarding PC education can be observed. The increasing acceptance of PC education is reflected in the students’ feedback (Bar-Sela et al., Reference Bar-Sela, Mitnik and Zalman2017). In general, there is a new generation of students who are more open to PC philosophy and reflection. Hence, students call for the expansion of the range of courses. The situation is similar in European countries where students claim to benefit from PC education as the content of PC education meets their needs and is essential for their personal development toward becoming a good doctor (Anneser et al., Reference Anneser, Kunath and Krautheim2014; Carrasco et al., Reference Carrasco, Lynch and Garralda2015; Mason et al., Reference Mason, Paal and Elsner2020a). To enable personal and professional growth, the role of senior physicians as role models is of utmost importance, yet the personal resources to enable such growth at medical schools remain limited.
The information regarding teaching PC to undergraduate medical students in Israel has been controversial. A publication from 2015 indicated that PC is mandatory at all medical schools in Israel (Carrasco et al., Reference Carrasco, Lynch and Garralda2015). According to the European Atlas of Palliative Care, PC is not mandatory at any of the medical schools (Arias-Casais et al., Reference Arias-Casais, Garralda and Rhee2019). According to our survey conducted in late 2017, PC was mandatory at two medical schools in Israel. Developing and improving PC education is a global effort, but the collection of country-level information is highly dependent on the interests and knowledge of people identified as key informants. As the collaboration between Israeli medical schools in terms of PC undergraduate teaching has been described as infrequent, it can be estimated that the information about what is going on may be inaccurate.
In Israel, medical students are expected to understand and respect cultural and religious traditions regarding the end of life. Particular importance should be paid to the cultural safety of patients and their caregivers by cultivating humanness and cultural competencies in PC education (Shaulov et al., Reference Shaulov, Baddarni and Cherny2019). Already in 2013, the Council of Europe highlighted the need for structured programs of PC education incorporated into the training of all concerned healthcare professionals in member states. It stressed the necessity for all health and social care professionals and workers involved in providing PC to be trained appropriately for their tasks in a concrete, insightful, and culturally safe way (Council of Europe, 2013; Gamondi et al., Reference Gamondi, Larkin and Payne2013). In the survey, only Hadassah Medical School reported providing course on cultural aspects of patient care. During the interviews, it became evident that spiritual care (Best et al., Reference Best, Leget and Goodhead2020), which according to the participants encompasses more than religion, was integrated into the PC curriculum. Issues concerning methods of how to teach the broader understanding of spiritual care (Jones et al., Reference Jones, Paal and Symons2021) or cultural safety (Curtis et al., Reference Curtis, Jones and Tipene-Leach2019) in PC were not raised or discussed.
In the expert interviews, many ideas for the future developments of PC in Israel were presented. Concerning undergraduate medical education, the following three main goals can be outlined:
1. PC needs to become a mandatory subject for students: It is considered essential that PC physicians, universities, and the government work together to make PC a mandatory subject at medical schools. This step is the key to improving PC education to a high-level nationwide. A national level of decision-making is crucial even if universities are responsible for implementing the recommendations. At best, a PC formative circle should be initiated in which the lecturers from all teaching hospitals of all universities could gather to decide on a mutual goal. In this context, it is also important to allow the lecturers sufficient time for good teaching in addition to their clinical work. For sufficient importance and attention, PC needs to be established as an independent teaching and examination subject. Parallel to educational models, support for students who struggle with topics such as grief, death, and dying should be put in place. All recent curriculum-related recommendations of the European Association for Palliative Care (Paal et al., Reference Paal, Brandstötter and Lorenzl2019; Best et al., Reference Best, Leget and Goodhead2020; Mason et al., Reference Mason, Ling and Stanciulescu2020b) contain besides medical competencies and skills, strategies for self-care and self-reflection, compassionate communication, and whole-person care.
2. Improving teaching methods for PC: While practical training on patients and seminars in small groups are known to be particularly effective teaching methods, a large part of teaching is still done in lecture format. Therefore, to teach communication and other practical skills, interactive teaching strategies need to be developed. An international review committee made the same demand on Israeli universities as early as 2014 and advocated introducing simulation in teaching. In this regard, the medical universities are expected to cooperate nationwide (Committee for the Evaluation of Medical Study Programs, 2014; Reis et al., Reference Reis, Glick and Urkin2017).
3. Increased cooperation of PC experts in teaching: Establishing PC in medical curricula has been described as “a complex process in which enthusiastic leadership is of great importance” (Gibbins et al., Reference Gibbins, McCoubrie and Maher2009). In Israel, teaching would benefit from a nationwide exchange between universities and university clinics. The collaboration would empower leading PC professionals in their tasks could also be seen as more goal-oriented in terms of developing common strategies. Cooperation is useful for concrete projects, such as developing the online modules for hybrid courses. All medical schools would benefit from online modules embedded in their curriculum in a customized way.
“The education is a mirror of where PC stands in Israel today.” (D3J02, par. 24)
This quote from an interview partner underlines the importance of teaching in PC. This statement points out how undergraduate education mirrors the field and vice versa. This finding is relevant not for Israeli medical schools but should serve as a central measure of PC status worldwide. The study demonstrates that not only medical undergraduate education would benefit from the implementation of the addressed goals. Improving the teaching situation would automatically lead to a better practical implementation of PC. Optimizing PC education for medical students as well as for other healthcare professionals is desirable at under- and postgraduate levels for the benefit of people.
Limitations
All interviews were conducted in English, which was not the native language of either the interviewer or the interviewees. Conducting interviews in a participants' own language may have enabled them to better articulate their thoughts, avoiding possible semantic inaccuracies. Although the number of participants (n = 11) is low, according to the literature, Israel has around 30 PC specialists. We were able to recruit six of them. Involving one social worker as well as one participant with almost no contact with patients receiving PC may be seen as a limitation, but both of them played a relevant role in PC organization and/or implementation processes. The interviews were conducted between November 2017 and February 2018; we acknowledge that the situation has changed since then. Whereas the Covid-19 pandemic has likely enhanced online learning, access to bedside practice was further reduced. To successfully implement the global PC strategy and make it viable against various current and future challenges, structural change toward mandatory and well-designed PC education at medical schools is a must.
Conclusions
Regarding the teaching of PC at Israeli medical schools, it can be concluded that PC is not a mandatory subject, and therefore, the training of undergraduate medical students varies widely across the country. At only two out of the five universities, PC is taught as an independent subject. Overall, students are believed to understand the basic idea behind PC after completing their studies but are not well equipped to use PC in practice. To standardize and improve the situation nationwide, PC should be established as a mandatory subject in the curricula. Furthermore, the predominant lecture format of teaching should be supplemented by more interactive practical exercises and seminars. Enhanced cooperation between experts would also be beneficial in terms of teaching. Developing methods and strategies to teach culturally safe care and communication would seem worthwhile, considering the high prevalence of different cultures, especially in the Israeli health care system. Overall, not only future physicians as well as the entire healthcare system, and thereafter, the Israeli population would benefit from an improved PC education.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951521001450.
Acknowledgments
We like to thank all teaching faculty who generously shared their time and experience for this study. This paper would not have been possible without the exceptional support and dedication of Judith Rosenberg, M.A. Her expertise and precision helped us to improve this paper in innumerable ways. We sincerely thank three anonymous reviewers and the managing editor for their time and constructive feedback.
Competing interests
The authors declare that they have no competing interests.




