Introduction
Code status among hospitalized patients is an important part of understanding patient's goals of care. Patients’ code status can be customized, with the most common including full, partial, do-not-resuscitate (DNR), and comfort care only. Full code signifies full resuscitation efforts in case of a cardiopulmonary arrest without restrictions. Partial code includes statuses such as do-not-intubate (DNI), intubate only without chest compressions, chemical code with medications only, and do-not-defibrillate (Rafiq et al., Reference Rafiq, Ullah and Naglak2019). DNR indicates declining resuscitative efforts including chest compression, defibrillation, intubation, and chemical resuscitation during a cardiopulmonary arrest. Finally, comfort care implies an impending death with avoidance of aggressive medical interventions and liberal use of analgesics or anxiolytics for comfort. In a survey of more than 200,000 adult patients in California between 2008 and 2012, full code was the most common code status with 82.5%, followed by DNR at 15.3%, partial at 1.5%, and comfort care only at 0.7% (Kim et al., Reference Kim, Escobar and Halpern2016).
Code status decisions are affected by factors such as patient preferences, medical prognosis, patients’ understanding of available interventions, as well as family dynamics or preferences of a healthcare proxy. Another potential influencer though is severe mood conditions such as major depressive disorder (MDD), an increasingly prevalent illness (Weinberger et al., Reference Weinberger, Gbedemah and Martinez2018) affecting an estimated 12% (95% confidence interval (CI): 10–15%) of general inpatient medicine and surgical patients (Walker et al., Reference Walker, Burke and Wanat2018). Because poor medical prognosis can influence both code status decisions and depression separately, the association of MDD with code status independent of prognosis is poorly understood.
While clinicians routinely encounter patients with DNR code status, the evidence is sparse on the epidemiology of those with DNR order and its association with MDD. This study aims to investigate the demographics of those with DNR, the relationship between DNR order and having MDD diagnosis, and differences in hospitalization outcomes among those with DNR with and without MDD.
Methods
Database
The Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample (NIS) database was used for years 2009–2013. As the largest publicly available inpatient healthcare database in the United States, it estimates more than 35 million hospitalizations nationally (Healthcare Cost and Utilization Project, 2021). With a 20% stratified sample of all discharges from United States community hospitals (non-governmental, but including tertiary centers), excluding rehabilitation and long-term acute care hospitals, it provides a nationally representative sample of hospitalization data. The dataset includes diagnoses and procedural codes (International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM]), demographics, and hospitalization outcomes. Our study was exempt from the Tufts University Medical Center Institutional Review Board because this research did not involve human subjects and only included de-identified administrative data.
Classification of code status and mood disorders
We identified patients with do-not-resuscitate orders using International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM] code V49.86 (Table 1). Mood disorders including MDD were categorized according to the ICD-9-CM codes in Table 1. Of note, patients with MDD in partial or full remission (ICD-9-CM codes 296.25, 296.26, 296.35, 296.36) were not considered as having MDD, as we wanted to assess the impact of active MDD on DNR status.
Table 1. ICD-9-CM diagnosis codes for identification of do-not-resuscitate, psychiatric comorbidities, and conditions affecting capacity

Inclusion and exclusion criteria
We included patients ages 18 and older who were hospitalized from January 1, 2009 to December 31, 2013. We excluded all patients with psychiatric comorbidities such as bipolar I disorder, schizophrenia, schizophreniform, schizoaffective, and other unspecified psychoses including brief psychotic disorder that may be confounders. We did not exclude patients with comorbid substance use disorders due to a significant overlap between substance use and depressive disorders (Currie et al., Reference Currie, Patten and Williams2005; Davis et al., Reference Davis, Uezato and Newell2008; Shantna et al., Reference Shantna, Chaudhury and Verma2009). We also excluded patients who may lack decision-making capacity such as those with altered mental status, dementia, and intellectual disability to minimize the effect of decision-making by healthcare proxy. We did not include patients under the age of 18 as code status in pediatric populations is much less frequently documented and its determination is much more complex with many external influences outside of the patient's individual preferences. Of note, we did include patients with suicidal ideation (ICD-9-CM code V62.84) but used it as a covariate in the multivariable logistic regression as described below.
Outcomes of interest
The first research question we wanted to answer in this study was “Does having MDD have any association with having a DNR order in the inpatient setting?” To answer this, we first analyzed demographic factors such as the absolute number and proportion of hospitalizations that had DNR orders, and how many patients with DNR status had MDD of different severities. We computed demographic figures including age, sex, race, primary insurance, and proportion having suicidal ideation among those with DNR orders, stratified by MDD presence. We determined the strength of association between varying levels of MDD severities with having a DNR order among all hospitalized patients using regression analysis.
The second research question we wanted to answer was “Among patients with DNR order, does having MDD affect mortality or hospital outcomes in any way?” For this investigation, we tested the strength of association between varying levels of MDD severities and inpatient death among those with DNR using regression analysis. We also implemented a subanalysis among those with septicemia (ICD-9 code 038*) as their principal diagnosis and having a DNR order, and assessed the impact of MDD on inpatient mortality. The purpose of the subanalysis was to assess if the multivariable regression findings hold true when applied to a specific chief concern, whereby we could control for the underlying condition as well as its presumed prognosis. Septicemia was chosen as it was the second most common cause of inpatient death in the United States in 2010 (Hall et al., Reference Hall, Levant and DeFrances2013). We also compared hospitalization outcomes such as length of stay, total charges, the proportion of patients who left against medical advice, and death among DNR patients with and without MDD.
Statistical analysis
Chi-squared tests were used to test for differences between patients with and without DNR orders in demographics and hospitalization outcomes. To understand baseline comorbidity differences among those with and without MDD, we used the 31 comorbidities that comprise the Elixhauser Comorbidity Index (ECI) and computed the ECI weighted sum for those with and without depression. Multivariable logistic regression was used to estimate the adjusted odds ratios (aORs) for comparing the likelihood of having DNR status based on varying severities of MDD among all hospitalized patients in a cross-sectional analysis. Multivariable logistic regression was also used to estimate the aORs for computing the likelihood of inpatient death based on the presence of MDD among patients with DNR. In this multivariable analysis, we included covariates such as age, sex, race, suicidal ideation, and ECI in the models to adjust for potential confounders. Suicidal ideation was included as a covariate as it can acutely affect patients’ reasoning during a suicidal crisis, but it can be difficult to clearly distinguish between the effect of suicidal ideation and depression on their thought process regarding code status. Since the ECI is effective in incorporating the influence of comorbidities in models assessing the risk of in-hospital mortality and readmissions using administrative data (Elixhauser et al., Reference Elixhauser, Steiner and Harris1998; van Walraven et al., Reference van Walraven, Austin and Jennings2009; Moore et al., Reference Moore, White and Washington2017), its integration into our models was critical and helped delineate the precise effect of MDD regardless of medical prognosis. Other hospitalization outcomes including length of stay, hospital charges, and leaving against medical advice were compared using multivariable logistic and linear regressions. Statistical significance was set at p < 0.05 (two-sided). All analyses were carried out using Stata version 15 (Stata Corp, College Station, TX, USA). To calculate national estimates and standard errors, data were analyzed using appropriate discharge and trend weights provided by the HCUP (Healthcare Cost and Utilization Project, 2015). HCUP-NIS hospital data were used to calculate appropriate standard errors when working with smaller subsets of data that may include strata with single sampling unit (Houchens and Elixhauser, Reference Houchens and Elixhauser2015a, Reference Houchens and Elixhauser2015b).
Results
Patient population
We identified 688,506 inpatient stays with DNR order from 2009 to 2013, an estimate of 3.4 million (95% CI: 3.3–3.5 million) hospitalizations nationwide. This amounted to 2.3% (95% CI: 2.2–2.4%) of all hospitalizations during that period. Among DNR patients, the median age (interquartile range) was 82 (72–89) years and 40% of the hospitalization were for male patients.
Among patients having DNR order, 1.2% had any type of active MDD. Of those with DNR order and MDD, 51.8% unspecified single episode MDD, 0.7% had mild single episode MDD, 2.0% had moderate single episode MDD, 4.7% had severe single episode MDD, 25.6% had unspecified recurrent MDD, 1.0% had mild recurrent MDD, 4.8% had moderate recurrent MDD, and 9.5% had severe recurrent MDD. Less than 1% of the patients with DNR and MDD exhibited any psychotic behavior.
Among patients with DNR orders, those with MDD were more likely to be in younger age groups such as 30–74 and less likely to be in >90 age, more likely to be female, and more likely to be white relative to those without MDD (Table 2). Those with MDD were more likely than those without MDD to have private insurance, but less likely to use self-payment or other unspecified insurance. Suicidal ideation was more common among those with MDD than those without MDD.
Table 2. Demographics of patients with do-not-resuscitate orders in the United States, stratified by major depressive disorder: 2009–2013 combined, Nationwide Inpatient Sample

* p < 0.05; all values represent proportion % (95% confidence interval) except for first indicator, total weight number of patients.
Assessment of baseline comorbidities
Baseline comorbidities were assessed using ECI for all hospitalized patients with and without MDD (Supplementary Appendix I), and for all patients with DNR order with and without MDD (Supplementary Appendix II). Among all hospitalized patients, those with MDD were less likely to have 18 of the 31 comorbidities, including congestive heart failure, cardiac arrhythmias, and metastatic cancer. Those with MDD were more likely to have 10 of the 31 comorbidities such as alcohol abuse and drug abuse. The ECI mean was higher among those with MDD than those without MDD by 0.8 index point (95% CI: 0.7–0.8). Among those with DNR order, the MDD patients were less likely to have 10 of the 31 comorbidities, and more likely to have 15 comorbidities. Among DNR patients, ECI mean was higher among those with MDD than those without MDD by 1.1 index point (95% CI: 1.0–1.3).
Association of MDD with DNR
Multivariable logistic regression showed that those with MDD of any type were less likely to have DNR status than those without MDD. More specifically, patients with moderate single episode (aOR 0.77, 95% CI: 0.63–0.94), severe single episode (aOR 0.54, 95% CI: 0.48–0.62), moderate recurrent episode (aOR 0.74, 95% CI: 0.65–0.85), and severe recurrent episode (aOR 0.42, 95% CI: 0.37–0.48) were significantly less likely to have DNR status than those without MDD (Table 3). There was an inverse relationship between severity of MDD and odds of having DNR, with the more severe MDD patients being less likely to have DNR status than those with moderate MDD. Those with milder or unspecified forms of depression did not show any difference in odds of having DNR status relative to those without MDD.
Table 3. Association of major depressive disorder with do-not-resuscitate orders, United States: 2009–2013, Nationwide Inpatient Sample

* p < 0.05; model adjusted for age, sex, race, suicidal ideation, and Elixhauser comorbidity index.
Association of MDD with mortality in patients with DNR order
Among patients with DNR order, death was significantly less likely among those with MDD than those without (Table 4). The difference was evident with >40% reduction in odds of death for all severities of MDD except for mild single episode MDD.
Table 4. Association of major depressive disorder and inpatient death among patients with do-not-resuscitate orders, United States: 2009–2013, Nationwide Inpatient Sample
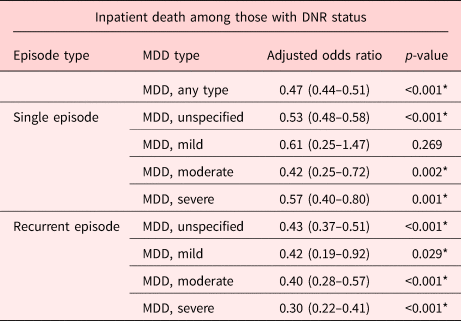
* p < 0.05; model adjusted for age, sex, race, suicidal ideation, and Elixhauser comorbidity index.
In the subanalysis, the mortality of patients with septicemia and DNR orders was analyzed. Patients with septicemia as principal diagnosis with DNR order who had any type of MDD had reduced risk of death (aOR 0.49, 95% CI: 0.42–0.57, p < 0.001) relative to those without MDD. When stratified by type of MDD, unspecified single, unspecified recurrent, and moderate recurrent MDD patients showed significant reduction in risk of death.
Differences in hospitalization outcomes by the presence of MDD in DNR patients
Among patients with DNR order, patients with MDD had longer length of stay of slightly less than one day and higher total charges by more than $4,500 relative to those without MDD (Table 5). Those with MDD had 9.9% lower inpatient mortality than those without MDD, and there was no significant difference in rates of leaving against medical advice between the two groups.
Table 5. Hospitalization outcomes among patients with DNR orders, stratified by major depressive disorder, 2009–2013; Nationwide Inpatient Sample

* p < 0.05; model adjusted for age, sex, race, suicidal ideation, and Elixhauser comorbidity index.
Discussion
Main findings
This is the first study to characterize the demographics of those with DNR code status in the inpatient setting and to determine the association between DNR status and MDD of varying severities. Having a DNR order was less likely among those with moderate or severe MDD, with an inverse association between likelihood of DNR status and severity of MDD. Those with DNR orders with MDD were significantly less likely to die during hospitalization than those without MDD. Patients with DNR order and MDD had longer length of stay, higher total hospitalization charges, and lower rate of inpatient death relative to those without MDD.
Association of MDD and DNR
Patients with moderate or severe MDD were less likely to have a DNR order than those without MDD. This may be surprising since the ECI was higher for depressed patients and ECI has been used in administrative data as a predictor of inpatient mortality (Elixhauser et al., Reference Elixhauser, Steiner and Harris1998; van Walraven et al., Reference van Walraven, Austin and Jennings2009; Moore et al., Reference Moore, White and Washington2017), suggesting that some external factor specific to depressed patients affected their reduced likelihood of having DNR status. One potential explanation is that clinicians are appropriately considering and assessing capacity in patients with MDD. Many clinicians may have concluded that moderately and severely depressed patients lacked medical decision-making capacity due to their depression. This is also consistent with the inverse relationship between the severity of MDD and the odds of having DNR status. Another possibility is that depressed patients with MDD may have different goals of care than those without MDD. A study of patients with advanced cancer found that patients who most highly valued cure and fighting cancer had significantly more depressive symptoms than those who had other goals of care (Rand et al., Reference Rand, Banno and Shea2016). Patients who value cure mostly and therefore would not opt for a DNR order may experience more depressive symptoms, while those who value goals other than cure may be at peace with their prognosis, choose DNR status, and experience less depression. Finally, it is also possible that depressed patients simply have not established their true values and goals of care, thereby establishing full code as the default code status in the hospital setting. One of the key clinical features of clinical depression includes lack of concentration and clear thought process which can impair genuine contemplation. Additionally, patients with depression can alienate both loved ones and clinicians by engaging in excessive reassurance-seeking behaviors (Coyne, Reference Coyne1976a, Reference Coyne1976b). Without the opportunity to thoroughly reflect on one's own values internally or discuss and express these values to others externally, coming to such a complex decision may be more difficult. Although a more detailed qualitative study is needed to explain these findings, the results suggest that with current clinical practice depressed patients ultimately do not have DNR orders more frequently than those without MDD and prematurely forego resuscitation because of their depression; rather, the exact opposite is true in the hospital setting.
MDD and risk of inpatient death in DNR patients
If the patient was moderately or severely depressed and chose DNR status, they were at least 40% less likely to die during inpatient hospitalization. One potential explanation could be that depressed patients obtained DNR status not solely based on medical prognosis but with the influence of their mood. The subanalysis for a cohort with chief concern of high mortality such as septicemia bolsters these findings. Even for the same diagnosis of septicemia with presumably similar risk profile for death regardless of depression, DNR patients with MDD were about half as likely to die as those without MDD. Patients with septicemia and MDD who decided to have DNR status may have been healthier than those without MDD, and may have opted to have DNR partially due to mood, and not solely prognosis. More insight could be gained from further research examining DNR patients and their differences in cause of death between those with and without MDD.
Lower mortality among patients with MDD relative to those without may seem contrary to published literature showing poorer outcomes among those with MDD, studied in patients with specific underlying conditions such as congestive heart failure, atrial fibrillation, and asthma (Jiang et al., Reference Jiang, Alexander and Christopher2001; Eisner et al., Reference Eisner, Katz and Lactao2005; Frasure-Smith et al., Reference Frasure-Smith, Lespérance and Habra2009; Kato et al., Reference Kato, Kinugawa and Yao2009; Prina et al., Reference Prina, Deeg and Brayne2012; Hare et al., Reference Hare, Toukhsati and Johansson2013). However, many of these studies show long-term outcomes such as 1- to 2-year mortality or rehospitalization rates. In the acute inpatient setting, depressed patients with DNR order appear to have a much lower risk of individual hospitalization death relative to DNR patients without depression.
Hospitalization outcomes
Apart from mortality, other inpatient hospitalization outcomes such as longer length of stay and higher total charges among DNR patients with MDD relative to those without MDD were consistent with previous findings (Hosaka et al., Reference Hosaka, Aoki and Watanabe1999; Frasure-Smith et al., Reference Frasure-Smith, Lespérance and Gravel2000; Prina et al., Reference Prina, Deeg and Brayne2012). These findings reinforce the need for early involvement of consultation-liaison psychiatry in the inpatient setting to reduce length of stay and hospitalization costs (Strain et al., Reference Strain, Lyons and Hammer1991).
Implications for practice
Given the cross-sectional nature of this study, the associations elucidated above cannot be extrapolated to causality, and without knowing the exact mechanism of the findings no definitive policy implications can be made. What the data does show is that depressed patients are less likely to have DNR status with current clinical practice, and among DNR patients those with depression are less likely to die while hospitalized. One may argue depressed patients are more likely to prematurely forego resuscitative efforts and experience higher inpatient mortality because of their mood despite a reasonable chance at meaningful recovery, but the data above refutes this possibility. Although grossly this may hold true, without more in-depth qualitative studies investigating how depressed patients process code status decisions and any differences in the cause of death between those with and without MDD, it is difficult to draw definitive mechanisms of these associations and further policy implications. Code status discussion is unique and nuanced to each patient and one's clinical status, and the different mechanisms proposed above that may contribute to these findings can be further explored through future studies.
As the findings show mood can be associated with different code status assignments during hospitalizations, and thoughtful clinicians should be aware of how mood is affecting patients’ thought process, including around decisions regarding code status. Regardless of the code status of a single hospitalization, given the poorer long-term outcomes of depressed patients it is essential for clinicians to utilize each inpatient stay as an opportunity to intervene if longitudinal care for the patients’ MDD is lacking with early involvement of psychiatry consultations.
In addition to ensuring adequate longitudinal treatment for MDD, another potential implication is ensuring more frequent and in-depth goals of care discussions between clinicians and patients who are experiencing MDD. Given that patients with depression tend to alienate others and may suffer from impaired concentration and thought process, genuine contemplation of one's own values and goals of care especially in a busy hospital setting can be difficult. For a more authentic and consistent understanding of patients’ preferences, clinicians need to engage in frequent, longitudinal follow-up and adequately document their wishes in order to avoid confusion regarding goals during an acute hospitalization.
Strengths and limitations
The strengths of this study include the use of a large-scale, nationally representative database including multi-year trends. The use of ECI in the multivariable regression models also delineate the specific effect of MDD on code status by controlling for medical prognosis, which is often one of the most important determinants of code status.
The findings here are limited in that this was a cross-sectional study, and although several hypotheses that may explain the above associations have been suggested, they could not be verified without qualitative interviews in a prospective cohort. In addition, the findings are based on each inpatient encounter, which does not translate directly to patient-level data, as one patient could have had multiple inpatient encounters during the study period. Within the data source, the categorization of MDD had a significant proportion as being unspecified, which is nonspecific. Psychiatrists in the inpatient setting often defer specifying MDD severity given their brief, limited interaction or the patients have comorbid psychiatric conditions such as polysubstance abuse that obfuscate the definitive diagnosis. This may limit some of the specific findings regarding clinical outcomes and varying severity levels, but the association between MDD overall and DNR status or mortality are unlikely to change. The findings here also may be limited by incomplete documentation of DNR status, as only 2.3% of hospitalizations were DNR, a figure much lower than previously reported ones (Kim et al., Reference Kim, Escobar and Halpern2016). It was also not possible to assess whether code status decisions were made by healthcare proxies or by the patient, though this effect was minimized by excluding patients with dementia, intellectual disability, and altered mental status. Depressed patients with psychotic behavior were included in the study which could have affected their capacity, though less than 1% of DNR patients with MDD actually exhibited any psychotic behavior. Finally, though the data are >5 years old, the large sample size and multiyear analysis make the findings generalizable and applicable to current practice.
Future research
Further research in the form of chart review, surveys, and qualitative studies can provide insights into patients’ thought process and the reasons why those with depression are less likely to have DNR status. It can also investigate the difference in cause of death between DNR patients with and without MDD to provide more precise insights into depressed patients’ lower mortality rates. Finally, it can show the impact of healthcare proxies on code status decision-making for depressed patients.
Conclusion
Determining appropriate code status is a standard of care for all hospitalized patients. It can help clinicians to be aware of factors that can be associated with code status decision-making, including mood disorders. Depressed patients are less likely to have DNR status, and even with DNR status are less likely to die in the hospital relative to those without depression. Further research is needed to elucidate the exact mechanism of these findings. Clinicians can advocate for patients with MDD by ensuring longitudinal follow-up with psychiatry and primary providers for mental health and ongoing goals of care discussions.
Supplementary material
The supplementary material for this article can be found at https://doi.org/10.1017/S1478951522000463.
Acknowledgments
We thank Tufts University Department of Orthopaedics for making the Nationwide Inpatient Sample available for this study.
Funding
This research received no specific grant from any funding agency, commercial, or not-for-profit sectors.
Conflict of interest
The authors declare no potential conflicts of interest with respect to research, authorship, or publication of this article.








