Background
Non-communicable diseases (NCDs) such as cancer are a public health concern worldwide (DePinho and Hawk, Reference DePinho and Hawk2016; Chan, Reference Chan2017). In Mexico, cancer is the third leading cause of death (World Health Organization, 2018), with a high percentage of cases diagnosed at the later disease stages (Reynoso-Noverón et al., Reference Reynoso-Noverón, Meneses-García and Erazo-Valle2016).
The National Comprehensive Cancer Network (NCCN) (2018) defines distress as “unpleasant emotional experience of psychological, social, and spiritual nature that interferes with the capacity to cope with cancer diagnosis and its treatment.” The NCCN's definition is internationally recommended as a necessary standard for appropriate cancer care given its high prevalence, negative consequences on quality of life, and validity as confirmed and applied in many countries (Mansourabadi et al., Reference Mansourabadi, Moogooei and Nozari2014). During the cancer trajectory, 22% (Lloyd-Williams and Friedman, Reference Lloyd-Williams and Friedman2001) to 89.3% of cancer patients report higher levels of distress (Küttner et al., Reference Küttner, Wüller and Pastrana2017) depending on the disease stage (Moscoso, Reference Moscoso2011; Holland et al., Reference Holland, Andersen and Breitbart2013) and cancer site (Herschbach et al., Reference Herschbach, Keller and Knight2004, Reference Herschbach, Book and Brandl2008).
High levels of distress in cancer have been widely reported in association with poor therapeutic adherence and treatment withdrawal, prolonged hospitalization, poor satisfaction with medical attention (Prieto et al., Reference Prieto, Blanch and Atala2002; Kennard et al., Reference Kennard, Stewart and Olvera2004), communication problems, emotional disorders, such as anxiety or depression (Kelly et al., Reference Kelly, Ghazi and Caldwell2002; Herschbach et al., Reference Herschbach, Book and Brandl2008), lower quality of life (Zabora et al, Reference Zabora, Brintzenhofeszoc and Curbow2001), desire for an early death, fear of the future, poor control of disease-related symptoms (Brenne et al., Reference Brenne, Loge and Kaasa2013; Lee et al., Reference Lee, Wu and Chiu2015; Singh and Harding, Reference Singh and Harding2015), and disease progression (Murray et al., Reference Murray, Kendall and Boyd2010). Most frequent issues among cancer patients include financial problems, worries, nervousness, getting around, and sleep (VanHoose et al., Reference VanHoose, Black and Doty2015).
Psychological disorders are generally not assessed and treated in oncological settings (Grassi et al., Reference Grassi, Johansen and Annunziata2013; Shimizu, Reference Shimizu2013; Randazzo and Peters, Reference Randazzo and Peters2016) and distress screening recommended to provide comprehensive care. Some of the most commonly used screening instruments include the Distress Thermometer (DT; Roth et al., Reference Roth, Kornblith and Batel-Copel1998; Hamilton and Kroska, Reference Hamilton and Kroska2019), Edmonton Symptom Assessment System (ESAS; Bruera et al., Reference Bruera, Kuehn and Miller1991), Hospital Anxiety and Depression Scale (HADS; Zigmond and Snaith, Reference Zigmond and Snaith1983), and the Brief Symptom Inventory-18 (BSI-18; Franke et al., Reference Franke, Jaeger and Glaesmer2017).
Most studies on distress in advanced cancer patients were conducted in high-income countries (HIC). We identified 30 from low- and middle-income countries (LMIC). Only one study was exclusively dedicated to advanced cancer patients (Guan et al., Reference Guan, Wang and Shao2019), and four included advanced cancer patients (Iskandarsyah et al., Reference Iskandarsyah, de Klerk and Suardi2014; Dessai et al., Reference Dessai, Chakraborty and Sajeev Kumar2015; Huey et al., Reference Huey, Guan and Gill2018; Sah, Reference Sah2019). The cutoff was ≥4 (Dessai et al., Reference Dessai, Chakraborty and Sajeev Kumar2015; Huey et al., Reference Huey, Guan and Gill2018) and ≥5 (Iskandarsyah et al., Reference Iskandarsyah, de Klerk and Suardi2014; Guan et al., Reference Guan, Wang and Shao2019). Guan et al. (Reference Guan, Wang and Shao2019) reported a 70.5% prevalence of high distress scores. Dessai et al. (Reference Dessai, Chakraborty and Sajeev Kumar2015) reported an 82% prevalence in patients with advanced cancer in contrast to 41.3% in non-advanced cancer patients.
The prevalence and sources of distress in patients with advanced cancer stages in LMICs are largely unknown. In Mexico, the GDP per capita is low, with a low standard of living, the lowest average salaries in the world, low educational levels (8.6 degrees in urban populations and 5.7 degrees in rural populations), and high levels of poverty and inequality (OECD, 2019).
This study identified the levels of distress and associated factors in patients with advanced cancer consulting at the outpatient palliative care unit at the National Cancer Institute in Mexico City, Mexico.
Design
A retrospective study of data collected from electronic medical records of patients with advanced untreatable cancer (incurable, locally advanced, or metastatic cancers) (American Cancer Society, 2013) at the palliative care unit at the National Cancer Institute in Mexico City who were seen between June 2015 and December 2016 was conducted. Patient records with incomplete data/information were excluded. Variables were assessed during the patients’ first visit to the outpatient palliative care unit.
Instruments
The DT is a self-assessed one-item 11-point Likert scale represented on a visual graphic of a thermometer that ranges from 0 (no distress) to 10 (extreme distress), in which patients indicate their level of distress the week prior to assessment. Additionally, on a 35-item Problem List (PL), the patients identify specific problems as their sources of distress. The most recent version of the NCCN practice guidelines for the management of distress recommends that a DT score ≥4 indicates moderate to severe distress (Cutillo et al., Reference Cutillo, O'Hea and Person2017). The DT has been validated in palliative care settings (Gessler et al., Reference Gessler, Low and Daniells2008; Wüller et al., Reference Wüller, Küttner and Foldenauer2017). In Mexico, the DT (Version 1.2008) has been validated as a reliable and accepted instrument with strong clinometric parameters (Almanza-Muñoz et al., Reference Almanza-Muñoz, Juárez and Pérez2008). This version was used in this study.
The Eastern Cooperative Oncology Group (ECOG) Performance Status (Oken et al., Reference Oken, Creech and Tormey1982) describes the patient's functioning level in terms of self-care, daily activity, and physical ability (walking, working, etc.). The ECOG scale consists of five categories: 0 (fully active, able to carry on all pre-disease performance without restriction) to 5 (death).
Medical and socio-demographic variables, including age, sex, civil status, place of residence, educational level, monthly income, and diagnosis, were also collected.
Statistical analysis
Categorical variables were described with frequencies and percentages, and continuous variables were described using the median and interquartile range (IQR). A simple logistic regression analysis between DT score and socio-demographic variables, medical variables, and PL was conducted. Independent variables that influenced the DT score in the simple logistic regression (P < 0.001) were included in the multiple logistic analysis. This cutoff point was considered to avoid variables that although could be statistically relevant were not relevant in the clinical context. For the simple and multiple logistic regressions, distress was considered a binary variable depending on whether the DT score was <4 (absence of distress) or ≥4 (presence of distress). The level of significance for the multiple logistic regression analysis was P ≤ 0.05, and clinically significant variables were discussed as predictors of a DT score ≥4. IBM SPSS v.21 and StataCorp. v.12.0 (2011) were used for the statistical analysis.
The Institutional Review Board approved the use of the patients’ information in this study (Ref. INCAN/CI/864/2017).
Results
Socio-demographic and clinical characteristics
We identified 750 palliative cancer patients from June 2015 to December 2016. Patients without psychological evaluation by triage (n = 79) or with incomplete or unknown information (n = 25) were excluded. Data from 646 patients were analyzed.
Overall, 62% were women. The participants’ median age was 57 years (IQR = 46–68). Most of the participants were married (54.8%) and lived in Mexico City (38.5%). 50% had fewer than 7 academic years (in 2018, the average academic years in the 55–64-year age group was 7.4 years) (National Institute for the Evaluation of Education, 2018). The median household income was US$199 (IQR = US$125–US$314), the minimum annual wage in Mexico was US$164, and the average wage was US$580. Gastrointestinal cancer was the most frequent diagnosis at 28.6% followed by gynecologic cancer (18.7%) and breast tumors (14.7%). ECOG 1 and 2 functional performance status was 33.4% and 38.9%, respectively. The sample characteristics are summarized in Table 1.
Table 1. The participants’ socio-demographic and medical characteristics compared to their distress level on the DT

IQR, Interquartile range; USD, United States dollar; ECOG, Eastern Cooperative Oncology Group.
Prevalence of distress and problem list (PL)
The analyses of the DT scores demonstrated a median of 4 (IQR of 2–6). A total of 362 (56.0%) patients were defined as distressed with a DT score ≥4. Table 2 shows the distribution of the patients’ socio-demographic and clinical characteristics according to their DT scores.
Table 2. Frequency distribution of the participants’ problem list item checked as a source of distress
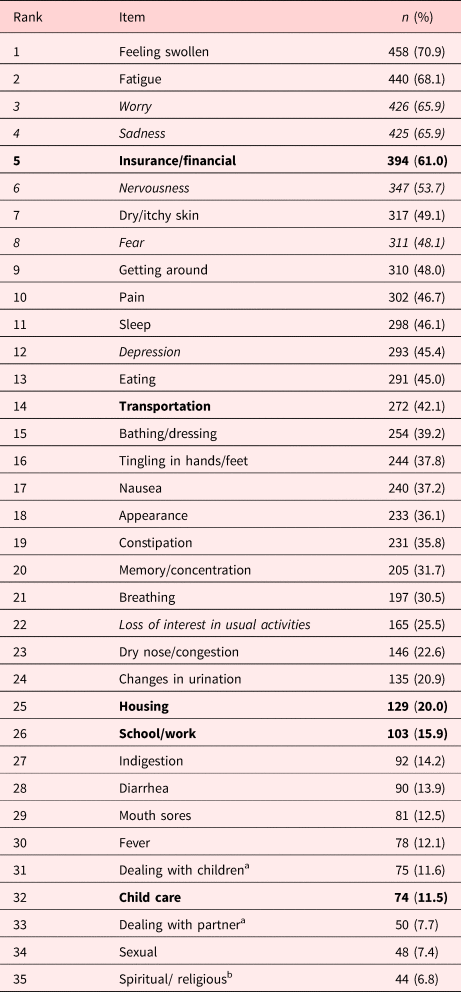
Italics represents emotional problems.
Bold represents practical problems.
a Family problems.
b Spiritual problems.
All of the items in the PL were mentioned. In the PL, the median for emotional problems was 3 of 6 items (IQR = 1–5), for physical problems was 7 of 21 items (IQR = 4–10), and for practical problems was 1 of 5 items (IQR = 1–2).
The most frequently reported problems were physical: feeling swollen (70.9%), fatigue (68.1%), dry/itchy skin (49.1%), getting around (48.0%), pain (46.7%), emotional worry (65.9%), sadness (65.8%), nervousness (53.7%), and fear (48.1%). In the practical category, financial security was mentioned by 61% of the participants, followed by challenges with transportation (42.1%). Family problems (10%) and spiritual/religious problems (6.8%) were the least mentioned categories. Table 2 compares the reported frequency of problems by the distressed and non-distressed patients.
The 10 most frequent problems reported by the distressed patients (DT score ≥4) were sadness (82.6%), feeling swollen (81.2%), worry (79.6%), fatigue (77.9%), insurance/financial (68.0%), nervousness (67.7%), fear (61.2%), depression (60.5%), getting around (58.6%), and eating (55%). The 10 main problems for patients reporting DT score <4 were feeling swollen (57.7%), fatigue (55.6%), insurance/financial (52.1%), worry (48.6%), dry/itchy skin (45.1%), sadness (44.4%), pain (38.7%), nervousness (35.9%), getting around (34.5%), and tingling in the hands/feet (33.5%) (Figure 1).

Fig. 1. Comparison of the percentages of the PL items according to the patients’ level of distress on the DT
The univariate analysis did not show associations with any of the socio-demographic variables (P < 0.001); however, the clinical relevance of age (P = 0.007) and the ECOG (P = 0.002) in the distress level were considered in the final model. The simple logistic regression analysis of the reported DT scores and independent variables are shown in Tables 3 and 4.
Table 3. Simple logistic regression of the reported DT scores and socio-demographic and clinical variables

DT, Distress Thermometer; OR, odds ratio; IQR, interquartile range; USD, United States dollar; ECOG, Eastern Cooperative Oncology Group.
Bold values indicates P ≤ 0.0001.
Table 4. Simple logistic regression reported by the DT scores and Problem List
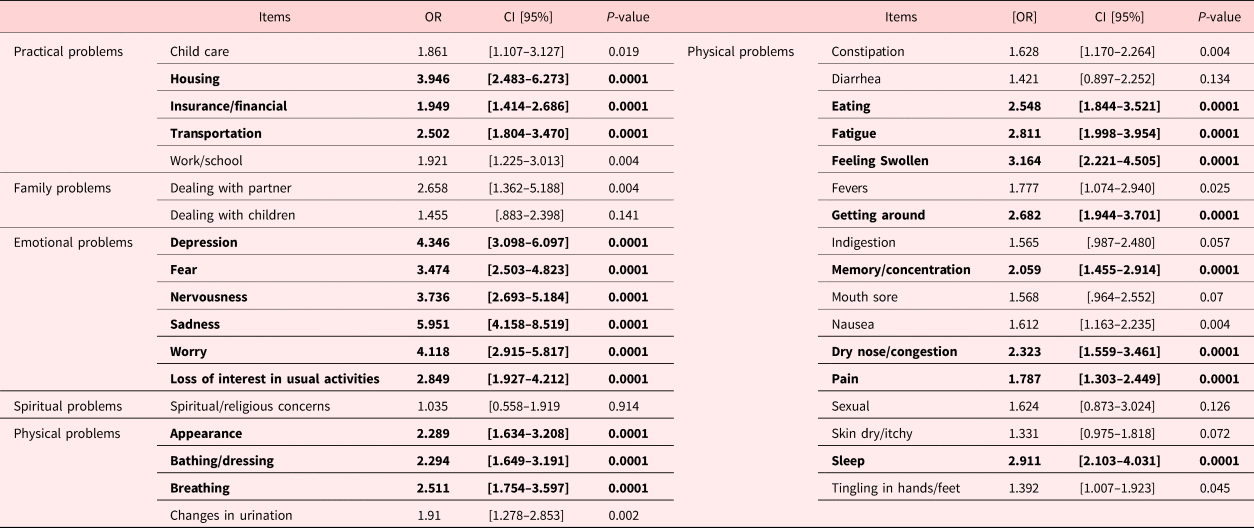
DT, Distress Thermometer; OR, Odds ratio; IQR, Interquartile range; USD, United States dollar; ECOG, Eastern Cooperative Oncology Group.
Bold values indicates P ≤ 0.0001.
Among the PL, the items that increased the odds of the presence of distress (DT score ≥4) with P < 0.001 in the emotional problems category were sadness (OR = 5.951), depression (OR = 4.346), worry (OR = 4.118), nervousness (OR = 3.736), and fear (OR = 3.474); in the practical problems category: housing (OR = 3.946), transportation (OR = 2.502), and insurance/financial (OR = 1.949); and in the physical problems category: feeling weak (OR = 3.164), sleep (OR = 2.911), fatigue (OR = 2.811), getting around (OR = 2.682), eating (OR = 2.548), breathing (OR = 2.511), dry nose/congestion (OR = 2.323), bathing/dressing (OR = 2.294), appearance (OR = 2.289), memory/concentration (OR = 2.059), and pain (OR = 1.787).
The variables that influenced the DT score in the simple logistic regression were included in the multiple logistic analysis for a final model predicting DT. In the multivariate analysis, the practical problems housing and transportation increased the adjusted odds of the presence of distress by a factor of 2.661 (95% CI = 1.538–4.602) and 1.732 (95% CI = 1.157–2.591), respectively. Emotional problems: sadness increased the adjusted odds of the presence of distress by a factor of 2.533 (95% CI = 1.615–3.973) and nervousness by 1.547 (95% CI = 1.014–2.203). Physical problems: eating and sleep increased the adjusted odds of the presence of distress by a factor of 1.626 (95% CI = 1.093–2.417) and 1.469 (95% CI = 1.980–2.203), respectively (Table 5).
Table 5. Multiple logistic regression of the predictive variables
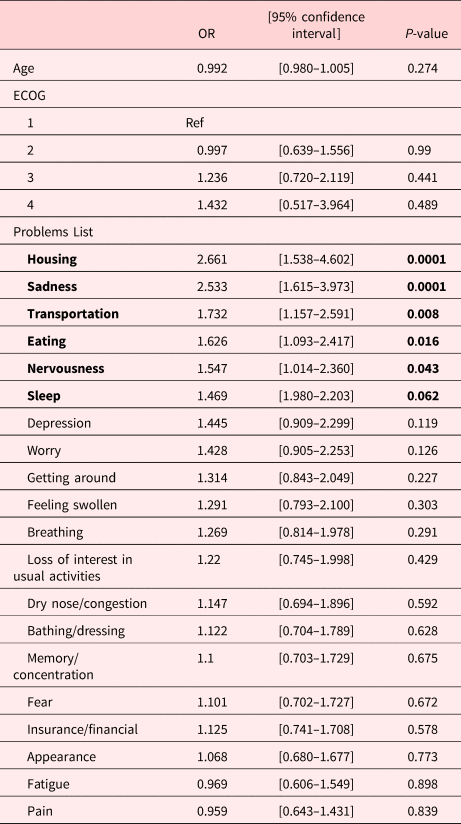
OR, Odds ratio.
Discussion
Advanced cancer patients in Mexico with palliative care requirements treated at the INCAN were mostly women. Half were younger than 57 years old. Their average educational level and income were below the average wage in Mexico. Overall, 56% of the patients reported high levels of psychosocial distress (DT score ≥4) with a median score of 4. This prevalence was lower than reported by advanced cancer patients in China (70.5%) (Guan et al., Reference Guan, Wang and Shao2019) and Nepal (81.7%) (Sah, Reference Sah2019). In HIC, the prevalence of palliative care needs in cancer patients who were cared for at home by a domiciliary palliative care service reported a high level of distress of 89.3% in Germany (Küttner et al., Reference Küttner, Wüller and Pastrana2017), and only 14% in Iceland reported that they had not experienced any distress (Gunnarsdottir et al., Reference Gunnarsdottir, Thorvaldsdottir and Fridriksdottir2012). In Middle Europe (Austria) and two southern European countries (Italy and Spain), cancer patients reported a 60% prevalence of distress (Meggiolaro et al., Reference Meggiolaro, Berardi and Andritsch2016). In Ireland, patients with medical oncology, hematology, and palliative care services reported a 53.6% prevalence of distress (Ryan et al., Reference Ryan, Gallagher and Wright2012). Akizuki et al. (Reference Akizuki, Yamawaki and Akechi2005) and Meggiolaro et al. (Reference Meggiolaro, Berardi and Andritsch2016) stated that factors such as economic, social, and cultural differences as well as medical conditions (for example, cancer type) might influence the evaluation of distress.
Socio-demographic characteristics were not associated with self-reported DT scores (Jacobsen et al., Reference Jacobsen, Donovan and Trask2005; Snowden et al., Reference Snowden, White and Christie2011). Previous studies reported gender differences. Various studies showed that women were more likely to experience and report distress than men (Snowden et al., Reference Snowden, White and Christie2011), but this was not significant in our sample. In addition to the ECOG 2, medical conditions such as the cancer site did not influence the DT scores as reported by Zabora et al. (Reference Zabora, Brintzenhofeszoc and Curbow2001).
Based on our model, the high distress score in the palliative care patients was associated with a young age and degree of dysfunctionality (ECOG 3 confined to bed or chair for more than 50% of waking hours) as reported by Goulia et al. (Reference Goulia, Papadimitriou and Machado2012), Waller et al. (Reference Waller, Williams and Groff2013), and Cormio et al. (Reference Cormio, Caporale and Spatuzzi2019). Similarly, Guan et al. (Reference Guan, Wang and Shao2019) reported that the poorer the Karnofsky Performance Status as influencing factor, the higher the DT score.
The presence of higher distress in younger patients (DT score ≥4) coincided with findings reported in the literature (Van Scheppingen et al., Reference van Scheppingen, Schroevers and Smink2011; Goulia et al., Reference Goulia, Papadimitriou and Machado2012; Kim et al., Reference Kim, Shin and Kim2013; Haynes-Lewis et al., Reference Haynes-Lewis, Clayton and Viswanathan2018). In a study of adolescents and young adults in China (15–39 years), Xie et al. (Reference Xie, Ding and He2017) reported a prevalence of 89.1% of DT score ≥4. Age and level of functionality are relevant in the clinical setting since patients with less functionality and adolescents and young adults (AYA) represent a greater challenge in oncological palliative care.
The participants reported physical and emotional problems more frequently. Sadness, worries, and nervousness were among the most frequent problems mentioned regardless of the DT score. Sadness and nervousness are predictive factors for increased distress, so psychological attention is required to prevent an adaptive or mood disorder. Emotional symptoms occur very frequently in the majority of cancer patients and may be part of the adaptive or maladaptive response to the disease depending on the coping strategies and resources of each individual patient. Although worries were the strongest single item associated with high distress scores as stated by VanHoose et al. (Reference VanHoose, Black and Doty2015), Skaczkowski et al. (Reference Skaczkowski, Sanderson and Shand2018), and Sah (Reference Sah2019), in our sample, this was not a predictor. In Ireland, the most commons problems were fatigue (66.8%), pain (52.2%), worry (45.4%), sadness (38.0%), and fear (37.1%). Overall, 13.7% endorsed the depression item, and 22.4% loss of interest (Ryan et al., Reference Ryan, Gallagher and Wright2012). Similar findings were reported in Iceland, where distressed patients indicated a higher number of emotional (depression, fear, and nervousness) and physical problems (Gunnarsdottir et al., Reference Gunnarsdottir, Thorvaldsdottir and Fridriksdottir2012).
Frequent physical symptoms of cancer were fatigue as reported by Teunissen et al. (Reference Teunissen, Wesker and Kruitwagen2007) in a systematic review of 44 studies (25,074 patients). Numerous studies described the relationship between cancer pain and psychological distress. Unrelieved pain increases the risk of psychological distress. Psychological factors influence both the experience of pain and the response to pain treatment in cancer patients (Zaza and Baine, Reference Zaza and Baine2002; Syrjala et al., Reference Syrjala, Jensen and Mendoza2014). According to a meta-analysis, 66.4% of advanced cancer patients experience pain (van den Beuken-Van et al., Reference Van den Beuken-Van, Hochstenbach and Joosten2016). However, in our study, pain was mentioned by 46.1% of the participants and was associated with a high distress score.
The most commonly mentioned practical problems by patients regardless of their DT score were financial problems. The patients’ income was higher than the minimum wage, but below the average wage in Mexico. The economic impact/financial burden of living with a chronic illness such as cancer is well-known (Essue and Essue et al., Reference Essue, Essue, Jamison, Gelband, Horton, Jha, Laxminarayan, Mock and Nugent2017; Dean et al., Reference Dean, Moss and Ransome2019) such as additional costs through transportation, since more than 60% of the patients were from other cities. Practical problems such as housing and transportation were a predictive factor for a DT score >4. Transportation was a source of distress in our population, probably due to the physical discomfort as well as time consumption and costs associated with it, as Mexico City and the metropolitan area have serious transit problems. Skaczkowski et al. (Reference Skaczkowski, Sanderson and Shand2018) reported that the most frequently identified problem in the practical domain was transportation. The association between distress and housing may be due to payments, family dynamics, responsibilities, roles, and proper functioning of their home while managing the limitations and symptoms of advanced disease.
Sleep problems were associated with DT scores ≥4. In general, sleep problems are common in patients with advanced cancer and are strongly associated with symptoms of pain, dyspnea, lower performance status, and distress (Palesh et al., Reference Palesh, Roscoe and Mustian2010; Sharma et al., Reference Sharma, Holm and O´Connor2012). Psychological distress influences sleep quality and sleep disorders and may induce or aggravate symptoms such as depression, anxiety, pain, fatigue, and deterioration of quality of life (Nishiura et al., Reference Nishiura, Tamura and Nagai2015). Therefore, it is important to identify distress in palliative care patients to improve their quality of life.
The relationship between DT scores and palliative care needs, especially emotional and practical needs, was demonstrated (Milne et al., Reference Milne, Aranda and Jefford2013). The most prevalent unmet needs were in the physical and daily living domain and the emotional domain (McDowell et al., Reference McDowell, Occhipinti and Ferguson2010). This reinforces Abraham Maslow's Theory of Human Motivation, which proposes a hierarchy of needs and factors that motivate people, identifying five categories of needs (physiological, security, love and belonging, esteem, and self-fulfillment), and constructed considering an ascending hierarchical order according to its importance for survival and motivational capacity (Angarita, Reference Angarita2007). We demonstrated this population's need for psychosocial support.
Latin American culture is characterized by spirituality and religiousness (Cruz-Oliver et al., Reference Cruz-Oliver, Talamantes and Sanchez-Reilly2014); however, spiritual issues were a problem in only a few cases, contrary to a study by Sah (Reference Sah2019) in Nepal, in which more than 50% of patients reported experiencing spiritual or religious concerns that were associated with high DT scores. It is possible that the DT was unable to detect all of the problems, and other specific tools may be necessary.
Limitations
This study had several limitations. First, the generalization of the results can be challenged since the patients were a heterogeneous sample with primary tumor sites and stages. It was a single-institution study, although it is the largest service provider in Mexico and is considered a typical oncological hospital functioning as a regional cancer center. However, we think that the results are applicable to other institutions.
Our study shares the limitations of retrospective studies. More data are necessary regarding protective and predictive factors behind the PL.
Although spiritual needs were frequently mentioned, in this study, it was not possible to detect them. The DT was insufficient for detecting and assessing spiritual problems, which can be important for treatment strategies (Gielen et al., Reference Gielen, Bhatnagar and Chaturvedi2017). Addressing spirituality can be necessary at the end of life as a coping resource to improve well-being in advanced disease stages and for its relationship in the relief of physical and emotional symptoms such as chronic pain, anxiety, and depression, which are recurrent in palliative care patients (Evangelista et al., Reference Evangelista, Lopes and Costa2016; Rudilla et al., Reference Rudilla, Soto and Pérez2018). In clinical practice, we consider applying some complementary assessment tools such as the Spiritual GES or FACIT-S.
Conclusion
In this study, more than half of the advanced cancer patients reported high distress levels. The routine/systematic use of the DT allows clinicians to identify patients with certain characteristics that may increase the risk of developing psychosocial distress and identify those who could benefit from additional resources. The screening also normalizes emotional status and explores different needs (Blais et al., Reference Blais, St-Hilaire and Fillion2014).
Our findings show that the presence of problems such as housing, transportation, sadness, nervousness, eating, sleep, and ECOG predict the level of distress in advanced cancer patients in palliative care in Mexico. The principal factors related to the level of distress were problems related to housing, transportation, and emotional problems such as sadness and nervousness.
In general, we consider the PL a good instrument to detect the needs of palliative and end-of-life cancer patients. Nevertheless, it must be complemented with different diagnostic instruments that will allow clinicians to further define patients’ needs including spiritual distress.
The psychosocial care of cancer patients is considered an essential component of the quality of cancer care. Detecting distress experienced by advanced cancer patients is particularly important for identifying the main needs of care to offer the best comprehensive treatment to patients and guarantee appropriate treatment in palliative care.
These findings contribute to understanding distress in Latin American cancer patients and confirm the importance of addressing psychological factors. We highlight the importance of our study as reports from limited-resource centers and LMICs remain scarce in the international literature.
Acknowledgments
The authors thank MD. Liliana De Lima, Msc., and Adriana Peña Nieves for their invaluable contributions to the data analysis. We also thank the following university students: Cassandra Pineda, Leonor Pérez, Daniela Ramírez, Elizabeth Alvarado, Andrea Hernández, Alberto Flores, Astrid Darani Bonora, and Alejandra Gutierrez
Conflicts of Interest
The authors declare no conflicts of interest.









