The number of individuals providing care for a family member or a partner is steadily increasing as a large proportion of the American population reaches late adulthood (Marks, Reference Marks1996; Schulz & Beach, Reference Schulz and Beach1999). Moreover, with long-term care costs rising and the population aging, the cost benefit of home-based care provided predominantly by a primary caregiver is very substantial (Congressional Budget Office, 2007). Despite this, caregiving is not without risk; the association between caregiving and health risk has been established in regard to the care of individuals diagnosed with a range of illnesses (Schulz et al., Reference Schulz, Visintainer and Williamson1990, Reference Schulz, O'Brien and Bookwala1995; Keefe et al., Reference Keefe, Ahles and Porter2003; Vitaliano et al., Reference Vitaliano, Zhang and Scanlan2003b). In addition, caregiving has been associated with immunosupression (Kiecolt-Glaser et al., Reference Kiecolt-Glaser and Dura1991), which may account for the mechanism by which individuals become susceptible to health problems. Caregivers have also demonstrated a small but significant cognitive decline as a function of caregiver stress compared to a matched sample of noncaregivers (Vitaliano et al., Reference Vitaliano, Zhang and Scanlan2003b).
With regard to the psychological consequences of caregiving, research indicates a consistent association between caregiving and a greater risk of developing a range of negative psychosocial outcomes including depression (Vachon, Reference Vachon, Whitman, Merluzzi and White1999; Pinquart & Sorensen, Reference Pinquart and Sorensen2003; Vitaliano et al., Reference Vitaliano, Zhang and Scanlan2003b). Depressed mood in caregivers is associated with higher levels of caregiving stress; greater quantity and intensity of symptoms; and more difficulty performing tasks than those with less depressed mood (Lu & Austrom, Reference Lu and Austrom2005). Therefore, the ability of caregivers to deal with their own physical and psychological symptoms is an integral factor in overall caregiving effectiveness. Along those lines, there is evidence that enhancing self-care behaviors leads to reductions in caregiver stress (Lu & Wykle, Reference Lu and Wykle2007).
In light of these findings and the critical role that caregivers are fulfilling in the informal provision of heathcare, researchers have begun to study the factors that may be associated with the ability to cope with the demands of caregiving, in order to aid the development of effective support services. Consistent with research on coping with stress, self-efficacy expectations (Bandura, Reference Bandura1991, Reference Bandura1997) have been identified as potentially important in predicting individuals' ability to cope with the stressors of caregiving.
With regard to caregiving, self-efficacy theory posits that individuals who possess high self-efficacy for performing the tasks of caregiving would be more successful in completing those tasks, report less incidence of psychosocial distress and physical illness, be at a reduced risk of caregiver burnout, and promote greater health benefits in those being cared for than those who are low in self-efficacy (Bandura, Reference Bandura1997). In support of this theoretical underpinning, research has consistently associated a high degree of reported self-efficacy with reduced risk of caregiver burnout and psychosocial distress (van den Heuvel et al., Reference van den Heuvel, de Witte and Schure2001) and decreased negative mood and caregiver strain (Keefe et al., Reference Keefe, Ahles and Porter2003). In addition, a high level of caregiver self-efficacy has been associated with improved patient well-being (Vachon, Reference Vachon, Whitman, Merluzzi and White1999; Keefe et al., Reference Keefe, Ahles and Porter2003). Consequently, interventions have been developed and implemented that have focused on enhancing caregiver self-efficacy. These have included training and support for caregivers of children with disabilities (Cullen & Barlow, Reference Cullen and Barlow2004); relaxation training for Alzheimer caregivers (Fisher & Laschinger, Reference Fisher and Laschinger2001); home-based training (Huang et al., Reference Huang, Shyu and Chen2003); and a yoga and meditation program for dementia caregivers (Waelde et al., Reference Waelde, Thompson and Gallagher-Thompson2004). These interventions resulted in enhanced caregiver self-efficacy for the management of psychosocial issues (Cullen & Barlow, Reference Cullen and Barlow2004); enhanced self-efficacy for caring for an individual with dementia (Huang et al., Reference Huang, Shyu and Chen2003; Waelde et al., Reference Waelde, Thompson and Gallagher-Thompson2004); and improved mood and well-being (Waelde et al., Reference Waelde, Thompson and Gallagher-Thompson2004). This study reports on the development of a measure of self-efficacy for caregiving, which assesses this critical stress-reduction resource.
Despite the importance of caregiver self-efficacy, current self-report measures suffer from a number of limitations; including: (1) disease-specific measurement; (2) lack of acknowledgement of the importance of interpersonal relationship and communication in caregiving; (3) neglect of positive aspects of caregiving; and (4) exclusion of items that deal with caregiver self-care. For example, the measures currently available focus primarily on coping with the difficult or negative aspects of caregiving (Steffen et al., Reference Steffen, McKibbin and Zeiss2002) or on problems with caregiving for persons with dementia (Fortinsky et al., Reference Fortinsky, Kercher and Burant2002). The relationship and communication with the person receiving care are inherent in the caregiving process (Vachon, Reference Vachon, Whitman, Merluzzi and White1999); therefore, its absence in current measures illustrates that the dominant focus in caregiving is on problems, tasks, and burdens to the exclusion of caregiving behaviors that are aimed at managing the relationship. Additionally, the lack of focus on self-care in existing measures also reflects a degree of oversight of what may be a critical component in preventing caregiver burnout (Vachon, Reference Vachon, Whitman, Merluzzi and White1999). For example, the ability to identify benefits of caregiving such as the discovery of personal strength and personal growth in adversity has been linked with coping and finding meaning in caregiving (Wong et al., Reference Wong, Ussher and Perz2009).
In sum, the purpose of the current study is to report the development and initial psychometric analysis of the Caregiver Inventory (CGI), a non-disease-specific measure of self-efficacy for caregiving that reflects a more comprehensive relationship orientation than currently exists in measures, and takes into account caregivers' own self-care and possible positive aspects of caregiving. The CGI was expected to have a coherent and representative factor structure, with scales that related negatively with measures of stress and burden.
METHOD
Participants
Pilot Sample
A sample of 35 caregivers was recruited from a hospice and palliative care organization and from a support center for caregivers of those with dementia. About half of the caregivers were caring for a person with cancer or other diseases (e.g., advanced chronic obstructive pulmonary disorder [COPD], chronic heart failure [CHF]) and about half were caring for a person with Alzheimer's disease (AD). All participants were primary caregivers who were caring for someone at home. Social workers in the hospice organization accrued caregivers who were receiving hospice services. The caregivers of those with AD were recruited by a staff member of the organization. The latter participants were either attending a support group for AD caregivers or were visitors to the support center. The age range for the caregivers was 56–80 years. All caregivers were compensated for their participation or chose to have their compensation donated to the organization.
Hospice/Palliative Care Sample
In another wave of accrual, caregivers from a regional hospice and palliative care agency were approached by their social worker on the second visit to the patient's home. The inclusion criteria included eligibility for hospice or palliative care and at least two social worker visits. Over a 2-year period, 183 caregivers were approached and 141 agreed to participate, and completed the study materials. In the second year of data collection several measures were added to the caregivers' and social workers' materials. Eighty-one primary caregivers completed these materials, which are described in the Measures section.
The participants had a mean age of 60.44 and were predominantly female (75.7%), Caucasian (86.3%), and married (77.3%). Participants were generally employed (26.35%) or retired (40.7%), and had a high school degree (35.85%) or some college (29.5%). About 50% had been caregivers for <15 months and 35% had been caregivers for <7 months. The most common diseases of the care recipients were cancer (52.1%), COPD (8.75%), stroke (5.95%), CHF (9.5%), and dementia (6.1%).
Measures
Caregiver Inventory
Initially, a pool of items was developed by T.V.M. and D.O.V. after a thorough review of the literature, and through interviews with eight caregivers who were receiving supportive services from hospice/palliative care or an AD support center, and three professionals who provided direct services to caregivers. The interviews were developed to probe not only for the burdensome and stressful aspects of caregiving, but also for the positive aspects, issues of self-care, and managing communication and the relationship with the care receiver. To cull items from the larger pool of 89 items, a pilot cluster analytic study was conducted involving 35 hospice and AD caregivers (i.e., pilot sample described above) who were asked to sort the 89 items into piles in which the “items were similar to each other and different from items in other piles.” Item cluster analysis was computed using the agglomeration approach with the squared Euclidean distance (standardized) measure, and nearest-neighbor linkage method (i.e., single linkage). Based on T.V.M.'s and D.O.V.'s inspections of cluster solutions that ranged from 7 to 12, a 10-cluster solution that included all items in clusters >2 was chosen. Twenty-one items were then chosen based on (1) the representation of the items from each cluster, (2) their position relative to the center of the cluster in a plot of items in clusters, and (3) non-redundant wording of items. Those 21 items were randomly ordered and paired with the 9-point Likert scale (1 = “not at all confident” to 9 = “totally confident”) that assessed confidence in the ability to perform the caregiving behavior. In subsequent testing, the CGI was completed by the hospice/palliative care sample described above. Items that constitute the CGI are contained in Table 1.
Table 1. Means, standard deviations, and rotated factor loadings from the EFA (Model 1)
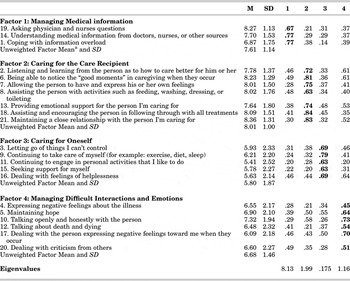
N=133, Boldface indicates highest loadings for each component.
aFactor means = sum of item scores/ number of items in the factor. This computation allowed for a direct comparison of means between factors.
Activities of Daily Living Rating (ADLR)
Caregiving is functionally tied to the care that the recipient requires. Therefore, the ADLR was adapted for the purposes of this study from two existing measures (The Index of ADL, Katz et al., Reference Katz, Ford and Moskowitz1963; and Instrumental Activities of Daily Living Scale, Lawton & Brody, Reference Lawton and Brody1969). Social workers from hospice, the staff from the AD support center, and T.V.M. and D.O.V.reviewed both measures and chose the most inclusive and critical items from Katz et al. and the Lawton and Brody measures. The result was an easily understood and easy-to-complete 10-item measure containing caregiver tasks (e.g., feeding, dressing, preparing meals, helping with walking, etc.), which caregivers rated in terms of the frequency with which they had to perform the tasks. In order to corroborate the caregivers' ratings of the ADLR, on the second home visit social workers rated the caregiving situation in 81 homes in our hospice/palliative care sample on the ADLR. The correlation between the caregivers' (ADLR-CG) and social workers' (ADLR-SW) scores was 0.63, indicating a high degree of congruence. Cronbach's α for the 10-item ADLR-CG was 0.83. Based on prior research (Fortinsky et al., Reference Fortinsky, Kercher and Burant2002), in which activities of daily living were unrelated to self-efficacy for caregiving, it was anticipated that the ADLR would be unrelated to the CGI. The ADLR-CG was completed by 81 primary caregivers in the hospice/palliative care sample and the social workers who accrued those caregivers.
Restricted Mobility
A checklist was appended to the ADLR, which contained the following items: “uses a wheelchair”; “uses a walker”; “uses a cane to walk,” “uses an oxygen tank”; and “bed-bound most of the time.” The intent of this objective measure was to assess more intense forms of caregiving that involve high levels of physical care related to the care receiver's restrictions in mobility. The caregivers checked off those items that applied to their caregiving situation. A simple sum of the checked items (range 1–5) was computed to represent restricted mobility by caregivers (RM-CG). Eighty-one participants in the hospice/palliative care sample completed this measure as did social workers (RM-SW). The correlation between the caregivers' (RM-CG) and social workers' (RM-SW) ratings of restricted mobility was 0.73 (p = 0.001), which indicated a very high degree of correspondence in the assessment of the mobility of the person receiving care.
Caregiver Burden Inventory (CBI)
The CBI (Novak & Guest, Reference Novak and Guest1989) is a commonly used measure of the impact of the burdens of caregiving on the caregiver. The CBI includes 24 items that are rated on a 5-point scale (“not at all” to “very applicable”). Responses to items such as, “My care receiver needs my help to perform many daily tasks” and “My care receiver is dependent on me” were summed to form a single burden score with higher scores indicating more burden from the tasks of caregiving. The internal consistency of the CBI for this study was .88 and was completed by 81 participants in the hospice/ palliative care sample.
Perceived Stress Scale (PSS)
The PSS (Cohen et al., Reference Cohen, Karmarck and Mermelstein1983) is a 10-item measure of the degree to which situations in one's life are appraised as stressful. The PSS has been used extensively in health research; for example, higher PSS scores are associated with failure to quit smoking, greater vulnerability to depression, and more colds (Cohen, Reference Cohen1986). The PSS has been endorsed as a psychometrically sound measure with “a respectable record of validity studies (including noteworthy biological correlates)” (Monroe, Reference Monroe2008; p. 10.11). The α for the PSS in the current study was .86 and was completed by 81 participants in the hospice/palliative care sample.
Demographic and Medical Information
All participants completed a demographic and medical information form. These data are reported in the participants section.
Procedure
In all data collection, every attempt was made to reduce participant burden. Therefore, at the behest of the social workers, who were responsible for accruing participants, the number of measures was restricted to those that were essential to meet the research goals of the study.
Caregivers who were involved in the hospice and palliative care home-based program were approached and asked for consent by a hospice social worker on the second visit to the caregiver's home. Because the hospice program only accepted patients who were receiving hospice or palliative care, the inclusion criteria were: (1) eligibility for hospice care and (2) having at least two social worker home visits. The two-visit criterion insured that caregiving was a critical continuing role for the person who completed the materials for this study. Nevertheless, this criterion also limited the number of caregivers that could be approached, because the majority of new intakes to hospice were imminent end-stage cases, which meant that for most of the hospice clientele only one social work visit was possible. The CGI and a demographics questionnaire were completed by all caregivers. In addition, 81 caregivers from this sample completed the ADLR-CG, RM-CG, PSS, and the CBI. After completing the materials (15–45 minutes), the caregiver placed the packet in a sealed envelope, which was given to the social worker, who delivered those materials to the research team, unopened. The social workers also completed the ADLR-SW and the RM-SW for each of the 81 caregivers, after the visit and away from the caregivers' homes.
Overview of Structural Model
In this study, Exploratory Factor Analysis (EFA) was used to investigate the factor structure of the CGI in the hospice/palliative care sample (N = 141). The goal was to produce a clinical and research tool that would be a valid measure of caregiver self-efficacy.
For the EFA (Table 1), a Maximum-Likelihood (ML) method of estimation was used; assumptions for using this method were met, including approximate normal distribution of the data for items. All analyses were conducted using M + , version 5.1. The default list-wise deletion option was used to handle missing data. Missing values in the data sets appeared to be randomly and evenly distributed, and there was a large enough sample size in the data set to offset the loss of eight caregivers, whose materials were not complete. Notably, the analyses yielded virtually identical results to a similar analysis that utilized mean substitution.
Criteria used to assess model fit included the χ2/df ratio and the Root Mean Square Error of Approximation (RMSEA). A well-fitted model would ideally have a χ2/df ratio between two and five with lower values indicating better fit (Marsh & Hocevar, Reference Marsh and Hocevar1985). In addition, adequate fit is indicated by a RMSEA index of < .08, representing reasonable errors of approximation (Browne & Cudeck, Reference Browne, Cudeck, Bollen and Long1993). Finally, improvement in model fit would be indicated by a reduction in residual error for the optimal model compared to other solutions with more or fewer factors included.
RESULTS
Reliability of the CGI
The internal consistency (Cronbach's α) of the 21-item CGI was 0.91. Item statistics (i.e., item-to-total-score correlations and α-if-item-deleted) indicated that no items performed poorly, and that all should be retained for inclusion in analysis examining the structure of the CGI.
Structure of the CGI
EFA was conducted in order to determine the smallest number of meaningful factors underlying the items in the CGI. A seven-factor extraction was carried out using PROMAX oblique rotation method. First, eigenvalues were examined using the eigen-criterion of >1.0; according to this rule, factors with eigenvalues >1.0 are good indicators of latent factors. A four-factor solution was the appropriate model based upon eigenvalues for the first four factors in the model. Eigenvalues for the first five factors were 8.13, 1.99, 1.75, 1.16, and 0.98, respectively.
The χ2/df values for factor solutions three through five were 1.61, 1.39, and 1.29, respectively, suggesting that these models provided a relatively good fit to the data according to criteria. Further indication that the four-factor model, in particular, was an optimal fit was indicated by improvement of RMSEA from 0.05 for the three factor solution to 0.04 for the four-factor solution. Another indication of the adequacy of the four-factor solution was the reduction in residual error over the three-factor solution, whereas the five-factor solution showed only slight improvement in residual error variances. Therefore, the four-factor solution appeared optimal.
Finally, the factor loadings were examined. The factor loadings in the four-factor PROMAX rotated solution provided some indication that a model with simple structure was adequate for these data. Factor loadings for the four factor model ranged from 0.45 to 0.84. The five factor solution was eliminated because of parsimony in that the factor structure was less clear, and there were multiple cross-loadings of items on the factors. For three factors, the structure was less clear in that several items did not load highly on any factor; this solution also suggested evidence of cross-loadings.
In the four-factor structure, items 1, 14, and 19 loaded highly on factor 1, with loadings ranging from 0.67 to 0.77; this factor reflected “Managing Medical Information.” Items 2, 6, 7, 8, 13, 18, and 21 loaded on factor 2 (loadings ranging from 0.72 to 0.84); this factor represented “Caring for the Care Recipient.” Items 3, 9, 11, 15, and 16 loaded highly on factor 3 with factor loadings ranging from 0.63 to 0.79; this factor reflected “Caring for Oneself.” Finally, items 4, 5, 10, 12, 17, and 20 loaded highly on factor 4 with loadings ranging from 0.45 to 0.73. This factor represented “Managing Difficult Interactions and Emotion.” In terms of item variance, the range of estimated residual variances was from 0.26 to0 .77. Overall, the analyses suggest that a four-factor solution provided the best fit for the data (Table 1).
Correlational Analyses
Preliminary analyses indicated that, with one exception, the critical variables in the study were not correlated with the caregivers' income, education, and time spent in the caregiver role. The one exception was that social workers' ratings of the tasks of the caregiving (ADLR-SW) were correlated with income (r = 0.40; p < 0.01) and education (r = 0.39; p < 0.01). Despite this, a comparison of partial (controlling for income and education) and zero order correlations of social workers ADLR-SW with other critical study variables revealed negligible differences. Also, the social worker ADLR-SW ratings were primarily used to corroborate the caregivers' ADLR-CG ratings. Therefore, all analyses were conducted using zero order correlations.
Correlational analysis revealed several relationships between the caregivers' and social workers' evaluation of caregiving tasks. A highly significant correlation was established between social workers' assessment of a caregivers' tasks (ADLR-SW) and the caregivers' (ADLR-CG) own assessment (r = 0.63, p < 0.01). Similarly, evidence that caregivers and social workers shared perceptions of the caregiving situation was also reinforced by the correlation between caregivers' (RM-CG) and social workers' (RM-SW) restricted mobility checklists (r = 0.73; p < 0.01). These correlations suggest that the caregivers' perception of the tasks of caregiving were accurate in the sense that they are validated or verified by the professional social workers' ratings of the caregiving situation. Therefore, any correlations of the CGI and the tasks of caregiving (ADLR-CG) by the caregiver are based on an objective (i.e., verified by the social workers) assessment of the caregiving needs in the home as opposed to some idiosyncratic perception by the caregiver.
In general, caregivers did not perceive a relationship between their daily tasks (ADLR-CG) and their self-efficacy expectations for caregiving (Table 2); the only significant relationship between ADLR-CG and any of the four factors of the CGI was for “Managing Medical Information.” This modest relationship indicated that the higher the level of ADLR-CG (i.e., a greater level of caregiver tasks required), the greater the efficacy for managing medical information such as asking questions, understanding medical information, and dealing with information overload. Similarly, social worker ratings of caregiver tasks (ADLR-SW) were only correlated with the caregivers' “Managing Medical Information” scores. Therefore, it is apparent that greater requirements for caregiving are accompanied by higher levels of self-perceived competence to handle the interface with medical professionals and medical information. Also, whereas there were no differences in the ratings of restricted mobility between caregivers and social workers, there was a modest correlation between the caregivers' ratings of restricted mobility (RM-CG) and the second factor of the CGI, “Care of the Care Recipient,” indicating that higher levels of restricted mobility were moderately associated with higher levels of efficacy for caring for the care recipient.
Table 2. Correlations of caregiver CGI scales with other measures

CGI = Caregiver Inventory; PSS = Perceived Stress Scale; CBI = Caregiver Burden Inventory; ADLR-CG = Activities of Daily Living Rating – Caregiver Rating; ADLR-SW = Activities of Daily Living Rating – Social Worker Rating; RM-CG = Restricted Mobility ratings by the caregiver; RM-SW = Restricted Mobility ratings by the social workers.
* p<.05.
** p < .01.
Each factor of the CGI was significantly correlated with the PSS (Table 2), indicating that perceived stress was highly related to caregivers' estimates of their self-efficacy in all aspects of caregiving. Therefore, high stress is related to low caregiver efficacy and, except for “Managing Medical Information,” is unrelated to the actual demands of caregiving.
The CGI was similarly related to caregiver burden (CBI) with significant correlations for factors 2, 3 and 4 of the CGI (i.e., “Care of the Care Recipient,” “Care of Oneself,” and “Managing Difficult Interaction and Emotions”). These relationships were slightly weaker than those of the factors of the CGI with PSS. It is also noteworthy that the CBI was related to the demands of caregiving (ADLR-CG). This relationship is clearly reflected in the items of the CBI, which correspond to the needs of the persons for whom care is being provided.
The strongest correlations for both the PSS and the CBI were with factors 3 and 4 of the CGI, “Care of Oneself” and “Managing Difficult Interactions and Emotions” (Table 2). Using Fisher's z to compare correlations, the relationships of the PSS with factor 3 (Caring for Self) and factor 4 (Managing Difficult Interactions and Emotions) were significantly stronger than for those of the PSS with factor 1 (Managing Medical Information) and factor 2 (Caring for the Care Recipient). These results suggest that these two dimensions, “Care of Oneself” and “Managing Difficult Interactions and Emotions,” which were heretofore neglected in caregiver research, are critical factors in caregiver stress and burden and add a new perspective the assessment of the caregiving situation.
Relative Importance Analyses
Relative importance analysis (Johnson, Reference Johnson2000; Feldman, Reference Feldman2005) involves the use of regression analysis to establish the relative importance of variables in the prediction of the criterion variable, particularly in situations in which the predictor variables are correlated. Dominant variables retain their predictive efficiency (i.e., variance accounted for) regardless of the interdependence of the variables. The results of the correlational analysis would suggest that all factors of the CGI would be predictive of stress and burden; however, given that “Care of Oneself” and “Managing Difficult Interactions and Emotions” were more highly correlated with stress and burden, they might emerge as the best predictors. Moreover, the interdependence of these factors could be parsed by relative importance analysis. Therefore, regression analyses were conducted on all of the CGI factors in order to narrow the relative analysis to only the significant predictors of stress and burden.
Because of the high correlation of stress (PSS) and burden (CBI) these variables were aggregated to form a composite Stress/Burden variable. In addition, the ADLR and RM ratings by the caregiver were aggregated to form a composite variable that reflected the tasks that were required in the caregiving situation. In the initial regression analysis (Table 3) the ADLR/RM variable was entered in the first step and the four factor scores of the CGI were entered in the second step. The ADLR/RM variable was a modest yet significant predictor of Stress/Burden (β = 0.08, p = 0.001) as were factor 3 (Care of Oneself, β = −0.30) and factor 4 (Managing Difficult Interactions and Emotions, β = −0.33). Relative importance analysis (Table 3) established that after taking into account the interdependence of the variable, they retained their predictive power, and whereas “Caring for Oneself” emerged as having the highest relative weight, there were no differences among the variables on relative weight based on the examination of 95% confidence intervals. Therefore, in terms of critical variables in the caregiving situation, caring for oneself, dealing with difficult interactions and affect, and the demands of the caregiving situation are all significantly associated with burden and stress, the former two in an inverse relationship and the latter in a positive relationship. However, examination of the standardized regression coefficients indicated that the prediction of burden-stress is marginally enhanced by the inclusion of the tasks of caregiving (ADLR-CG/RM-CG) relative to the more substantial contribution of the factors of the CGI that represent “Caring for Oneself” and “Managing Difficult Interactions and Emotions.”
Table 3. Relative importance analysis of the factors of the CGI with stress-burden as the criterion

CGI = Caregiver Inventory; ADLR-CG = Activities of Daily Living Rating – Caregiver Rating; RM-CG = Restricted Mobility ratings by the caregiver; Burden-Stress = Perceived Stress Scale +Caregiver Burden Inventory.
Finally, it is important to note that the mean item score (i.e., sum of factor item scores/number of items in the factor) for the factors (Table 2) reflected that fact that caregivers reported the lowest level of self-efficacy for “Caring for Oneself” (M = 5.80), followed by “Managing Difficult Interactions and Emotions” (M = 6.68), then “Managing Medical Information” (M = 7.61) and “Caring for the Care Recipient” (M = 8.01). These data suggest that the most difficult caregiving tasks are also the most important in terms of their relationship to burden and stress.
DISCUSSION
The results of the EFA establish the structure of the CGI, and identified self-care and dealing with difficult interactions and emotions as critical aspects of the caregiving process. Factor 3 (Care of Oneself) represents a new dimension in the assessment of caregiving self-efficacy and reflects a growing trend in caregiving in which self-care is viewed as important in the prevention of burnout (Vachon, Reference Vachon, Whitman, Merluzzi and White1999; Lu & Wykle, Reference Lu and Wykle2007). This dimension is more highly related to stress and burden than factor 2 (Care of the Care Recipient) and factor 3 (Managing Medical Information). Therefore, the confidence that caregivers have in their ability to successfully engage in self-care is highly related to their level of perceived stress and perception of burden, and presumably, depressive symptoms. Self-care practices can include maintaining one's health and well-being, actively seeking support, and maintaining some activity apart from the caregiving situation. It also includes dealing with helplessness and “letting go” in the sense of recognizing the limits of personal control. Therefore, an important aspect of self-care is the ability to identify and effectively manage the limits of control in the caregiving situation. This process often involves recognizing those situations in which attempting to invoke a high level of control, sometimes referred to as primary control, would be personally costly in terms of stress and burden, whereas letting go or accepting things as they are (secondary control) would be more adaptive and less stressful (Skinner, Reference Skinner1996). As a result, for an individual caregiver, adjustment may be optimized through discerning when problem-solving coping (i.e., primary control) is most effective versus when acceptance and emotion-focused coping is most effective. Although the current study was unable to further explore this process of discernment, it is an important direction for future research, especially in light of the fact that of all the factors, caregivers reported (on-the-average) the lowest ratings of self-efficacy for the items related to “Caring for Oneself.” Therefore, caregivers may need more help with self-care aspects of caregiving than with other areas where self-efficacy is greater (e.g., Caring for the Care Recipient). Finally, the regression analysis clearly identifies self-care as one of the dominant factors in the association between self-efficacy for caregiving and stress-burden. Therefore, interventions that do not acknowledge the role of self-care may be missing a critical variable in ameliorating stress and burden for those involved in the important work of caregiving.
The fourth factor, “Managing Difficult Interactions and Emotions,” was the factor with the second lowest efficacy ratings by the caregivers, indicating that the most critical dimensions of caregiving, “Caring for Oneself” and “Managing Difficult Interactions and Emotions,” are also the ones about which the caregivers felt the least confident in terms of their ability to perform those behaviors. “Managing Difficult Interactions and Emotions” includes talking about death and dying, dealing with negative feelings from the person for whom they are giving care, being able to express negative feelings, and dealing with criticism. These are all difficult tasks in the context of the demands of the caregiving situation, and self-efficacy for managing these difficult tasks is highly inversely correlated with burden-stress. This dimension should be an essential aspect of caregiver training and on equal footing with “Caring for Oneself.”
The second factor of the CGI, “Care of the Care Recipient,” focuses on those aspects of caregiving that are typically found in caregiver measures and includes tasks such as feeding, bathing, toileting, and adhering to treatments. This factor also includes aspects of caregiving that focus on the relationship with the care receiver and the positive aspects of caregiving, making it more comprehensive than scales in existing measures. This factor includes the caregivers' expectations regarding their ability to provide support in the context of a close relationship, establish open communication, and enable care receivers to express themselves. The items in this factor also identify positive aspects, or “good moments,” in their role as caregiver. In terms of the overall level of efficacy, caregivers were most efficacious in this domain compared to the other dimensions of caregiving that were represented in the CGI.
The first factor, “Managing Medical Information,” predominantly focuses on the interface with the medical community and obtaining and understanding information related to care. Typically, in addition to physical and emotional care, the caregiver is responsible for managing the patient's medical regimen and communication with healthcare providers. For some caregivers this responsibility may add stress to an already overwhelming situation. It is interesting to note that the caregivers' report of their self-efficacy in managing information is the only factor related to the actual caregiver tasks that are necessary (ADLR-CG) and is independent of caregiver-reported burden (CBI). Self-efficacy for managing information, however, is related to stress; the greater the efficacy for managing information the less the perceived stress. Given the bidirectional nature of this finding, it would be important to look at this relationship over time to establish the causal link between self-efficacy in managing information and caregiver stress. Also, these findings would suggest that yet another way to reduce caregiver stress would be to provide more training and support for caregivers to bolster their efficacy in managing medical information and communicating with the medical community.
For the most part, and in line with previous studies, there was no relationship between the objective tasks of caregiving and self-efficacy for caregiving (Fortinsky et al., Reference Fortinsky, Kercher and Burant2002; Gilliam & Steffen, Reference Gilliam and Steffen2006) with the exception of the relationship between “Managing Medical Information” and the tasks of caregiving (ADLR-CG). Therefore, the general findings support the notion that many aspects of caregiver efficacy are not determined by the demands of the caregiving situation. In other words, no matter how burdensome the caregiving, the most critical aspects of caregiving efficacy (i.e., “Caring for Oneself” and “Managing Difficult Interactions and Emotions”) remain independent of required tasks. Therefore, the actual demands of caregiving may be less of an issue in caregivers' burden and stress than their own expectations of their adequacy to take care of themselves and to deal with very difficult interpersonal interactions that are charged with negative emotion.
As noted, because these data are cross-sectional and the variables described are bi-directional, caution must be taken in interpreting the results; the relationship between self-efficacy, stress, and burden needs to be investigated further in longitudinal studies. In addition, because the data collection was conducted within the normal operations of the organizations involved, it was not possible to administer a broad scope of measures, such as the assessment of physical outcomes or more elaborate psychosocial measures. Despite these limitations, the CGI appears to be a structurally sound, reliable, and valid measure of self-efficacy for caregiving. In addition, the results of the current study support the argument that improving self-care self-efficacy would lessen stress and burden and certainly provide fertile ground for future research in this area. Finally, this research focused primarily on caregivers of hospice/palliative care cancer patients, whose caregivers were mostly Caucasian, married women. It would be important to investigate the external validity of these findings with respect to men, ethnic minorities, and caregivers' of people who have illnesses other than cancer.





