Introduction
During infancy and childhood, optimal eating patterns can promote healthy growth and development(1), and potentially improve school performance(Reference O’Dea and Mugridge2–Reference Nyaradi, Li and Foster4). Consuming a poor diet from a young age has been associated with an increased risk of becoming overweight or obese and the development of obesity-related conditions later in life(1). Dietary risk factors such as the consumption of sugary drinks, frequent snacking on high-energy dense foods, and consuming large portions all contribute to a positive energy balance(5,Reference Moreno and Rodríguez6) . In contrast, increased consumption of fruit and vegetables is associated with more positive health outcomes, including lower risk of cardiovascular disease and some types of cancer(7,Reference Wang, Ouyang and Liu8) . Promoting healthy eating habits among children is therefore essential, particularly as research indicates that a child’s eating behaviours and patterns might persist into adolescence and adulthood(Reference Craigie, Lake and Kelly9–Reference Nicklaus and Remy11).
Research suggests that nutrition education during childhood plays a key role in establishing healthy eating behaviours that continue as the child ages(Reference Dudley, Cotton and Peralta12). The school environment has been proposed as an ideal setting to provide education about a healthy lifestyle and healthy eating practices at an early life stage(Reference Strawser and Wachob13–Reference Lee17). Previous reviews have outlined the effectiveness of health-promoting school programmes on several outcomes such as healthy eating behaviour, nutrition knowledge and body mass index (BMI)(Reference Dudley, Cotton and Peralta12,Reference Pérez-Rodrigo and Aranceta18–Reference Wang, Cai and Wu22) . A Cochrane review reported a small, but clinically significant, BMI reduction in children aged 6–12 years receiving nutrition education in combination with physical activity interventions(Reference Waters, de Silva-Sanigorski and Burford19). Although the above shows the potential of nutrition education for supporting primary school children’s healthy lifestyle, research highlights the need for better implementation of future programmes into the regular school curriculum(Reference Strawser and Wachob13,Reference Pérez-Rodrigo and Aranceta18,Reference Waters, de Silva-Sanigorski and Burford19) .
Instead of implementing interventions that are resource and time intensive, and that lack long-term sustainability, future nutrition education interventions need to be developed such that they can be incorporated into usual teaching practices and operate within school systems and structures(Reference Pérez-Rodrigo and Aranceta18,Reference Waters, de Silva-Sanigorski and Burford19,Reference Follong, Prieto-Rodriguez and Miller23,Reference McIsaac, Spencer and Chiasson24) . Multiple studies investigating barriers to implementing nutrition lessons concluded that fitting these lessons into the school timetable is challenging(Reference Kipping, Payne and Lawlor25–Reference de Vlieger, Riley and Miller33), with core curricular subjects prioritised(Reference Hall, Chai and Albrecht26,Reference Upton, Taylor and Upton29,Reference Love, Booth and Margerison32) . This is particularly evident in primary schools where one teacher teaches several school subjects. In a survey conducted by de Vlieger et al. (2019), 80 % of participating primary school teachers indicated a lack of time as the main barrier for teaching nutrition(Reference de Vlieger, Riley and Miller33). This time constraint makes it hard to teach nutrition as a stand-alone school subject(Reference Perera, Frei and Frei30), and thus the focus should be shifted to the integration of nutrition curricula into other subjects such as mathematics, English and science(Reference Jones and Zidenberg-Cherr27,Reference Perera, Frei and Frei30,Reference Love, Booth and Margerison32) . This integrated approach would have a minimal effect on the amount of time spent on core subjects and therefore could overcome this barrier to implementing healthy eating interventions(Reference Jones and Zidenberg-Cherr27,Reference Peralta, Dudley and Cotton34) .
Although the integration of nutrition education with standard curricular subjects has been suggested in previous research, it is unclear how this approach has been used in interventions and whether it has been proven effective. To the best of the authors’ knowledge, the effectiveness of integrated nutrition education programmes has not been reviewed before. This scoping review aimed to provide an overview of the current research on teaching practices and effectiveness of primary-school-based interventions that use an integrated approach to implement nutrition education programmes into core learning areas within the curricula.
Methodology
Study design
A scoping review was determined as the most appropriate method given the broad study aim of exploring a topic that includes a range of study designs and outcome measures. Scoping reviews are commonly undertaken to examine the extent, nature and range of research activity, to summarise and disseminate research findings and to identify research gaps(Reference Arksey and O’Malley35). This type of review allows for mapping of existing literature on integrative nutrition education and provides a comprehensive picture of the research area. This scoping review followed the Joanna Briggs Institute Reviewer’s guidelines to ensure transparency in the reporting of our findings(Reference Peters, Godfrey and McInerney36). The manual is based on the methodological framework proposed by Arksey and O’Malley(Reference Arksey and O’Malley35), which was later updated by Levac, Colquhoun and O’Brien(Reference Levac, Colquhoun and O’Brien37), and further refined by Peters et al. in 2015(Reference Peters, Godfrey and Khalil38).
Search strategy
Six databases, Medline, CINAHL Complete, Embase, Scopus, EBSCO Megafile Ultimate and Eric, were searched in May 2019 using relevant search terms to identify studies integrating nutrition into the primary school curriculum (Table 1). The search was not restricted by date of publication.
Table 1. Search terms and fields used to conduct a scoping review on the integration of nutrition education into the primary school curriculum

Eligibility criteria
Types of participants
Participants included in the studies comprising this review were primary or elementary school children. As such, eligible articles needed to report on student-related outcomes. Studies conducted with children from various school levels, including primary school classes, were considered eligible. Interventions with middle-school students only were not included since the teaching structure may differ from that of primary school students. Studies specifically focusing on children with learning disabilities were excluded, as we were interested in studies representing general populations.
Concept
Programmes integrating healthy eating or nutrition education with curricular learning areas were included. Educational interventions, programmes, resources or approaches were only eligible if they included a nutrition or healthy eating component. Examples of nutrition-related topics are the intake of fruit and vegetables, sugary drinks, types of fat, portion size or nutrition labels. Studies were excluded if their focus was not on nutrition or healthy eating. General subjects such as health, home economics, life orientation, food chain or web, farming, food processing and food safety were not included as they target health- or food-related topics rather than nutrition-related topics. Furthermore, providing students with breakfast, fruit and vegetables, or other foods was not considered as nutrition education unless the intervention specifically targeted education concerning those food items. School-garden and cooking programmes were excluded if they involved hands-on gardening and food preparation tasks without a nutrition education component.
Integrated teaching was defined as an approach to teach a certain topic by embedding it across different curricular subjects and supporting the learning of all of them. Many interventions or programmes focus on multiple topics and target several health-related outcomes (e.g. physical activity). We screened for studies that target nutrition education and whether the nutrition component had been integrated or not. Studies were excluded when the healthy eating lessons had been taught parallel to the other intervention topics or when the lessons were not integrated with any other core subject.
In the current scoping review, only articles embedding nutrition content in core curricular subjects were eligible. Core curricular subjects included, but were not limited to, language arts, mathematics, literacy, science, social studies and physical education. As research shows that teachers have limited time available for subjects other than the core subjects, these will likely be prioritised over healthy eating or nutrition education(Reference Hall, Chai and Albrecht26,Reference Jones and Zidenberg-Cherr27) . Integrating lessons on healthy eating with non-core subjects would not reduce this time constraint. We therefore decided to exclude interventions that were integrated into a health-related curricular subject (e.g. home economics, life orientation, health, etc.). Other subjects which we did not consider core subjects included arts and crafts, music and theatre.
A clear distinction must be made between incidentally and explicitly integrated programmes. Teaching strategies that were incidentally connected to the learning of other subjects were those where other curricular concepts were present, but where there was no indication that the intention was for students to learn about these concepts(Reference Hickmott, Prieto-Rodriguez and Holmes39). This type of integration was not included in the current review. Solely studies in which the research team had described linking nutritional topics and the learning of other curricular subjects (explicitly integrated) were included.
Context
The nutrition education programmes had to be delivered through the primary school curriculum and involve classroom teaching or a curricular component (e.g. after-school programmes were excluded). Studies using multiple intervention components or whole school approaches were considered eligible, as long as one of the intervention components included nutrition education. This highlights the explorative nature of the current scoping review.
Types of sources
The current review screened for peer-reviewed journal articles. This ensured that we only included evidence-based literature that involved nutrition education programmes that had been rigorously evaluated. Sources such as book chapters, conference proceedings, correspondence letters, dissertations and abstracts only were excluded. Additionally, searches were limited to English text only.
Note: Eligibility criteria for study designs and type of outcome measures were not defined, as this is a scoping review and only a small number of articles were expected after screening.
Study selection
After the initial search was completed, all studies identified were uploaded to Covidence, and duplicates were removed by the lead author. Subsequently, study selection was based on meeting the inclusion criteria described above. To determine whether an article was included or excluded, all titles and abstracts were screened by two independent reviewers. When unclear as to whether an article was eligible for the review based on solely the title and abstract, the full-text article was examined. Disagreements were resolved by a third reviewer.
Full-text articles were obtained for all potentially relevant studies and then screened by the lead author and a second independent reviewer. In contrast to the title and abstract screening, conflicts resulting from the second round of screening were solved by discussion between the reviewers. Reference lists of reviews and all included articles after the initial round of full text screening were examined to identify additional relevant articles that would meet the inclusion criteria.
Data extraction
Data were extracted from the full-text papers included in the scoping review via a standardised data extraction process by the lead author. Where available, the following information was extracted and tabulated (Table 2):
-
Programme name, authors, year of publication, country of study, study design, study population (e.g. sample size, age, grade level) and intervention length
-
Lesson frequency and duration
-
Nutrition-related topics
-
Curricular integration
-
Lesson delivery and teacher training
-
Theoretical framework
Table 2. Programmes including a nutrition education component that is integrated into the primary school curriculum

QE, quasi-experimental; PS, primary school; I, intervention; C, control; NR, not reported; USA, United States of America; K, Kindergarten; TNR, teacher delivery with training not reported; CRCT, cluster randomised controlled trial; TT, teacher delivery with extensive training; NE, nutrition expert; RT, resiliency theory; SCT, social cognitive theory; UK, United Kingdom; SDT, self-determination theory; PCDT, Piaget cognitive development theory/constructivist learning theory; TRM, teacher delivery with role model training; NS, not specified; RM, repeated measures; SEM, social ecological model; TPB, theory of planned behaviour; MLM, mastery learning model.
a Programmes were described in one or multiple intervention studies. This number represents the number of studies reported per programme.
b Intervention studies were described in one of multiple papers. Each row refers to one paper.
c n is reported as number of students and represents (where possible) the number of students with pre- and post-test data, mean age reported as mean ± standard deviation (SD) in years.
d Only core subjects were included in this table.
* Number of lessons might cover multiple subjects rather than solely nutrition (e.g. a combination of physical activity and nutrition lessons, or nutrition and gardening lessons).
† Information reported on subject integration might be incomplete (e.g. only example subjects were provided).
Data on the intervention components (e.g. curriculum, parental involvement) and integration related findings were not tabulated, but summarised in text. Findings were organised and reported in multiple ways, including a descriptive numerical analysis to illustrate the extent, distribution and nature of the included studies, and a narrative summary to provide a more in-depth description.
Results
Study selection
Fig. 1 illustrates the study selection process. The initial search through all databases retrieved 4675 records. After duplicates were removed, a total of 3328 records were identified for title and abstract screening. Following title and abstract screening of the records identified, 257 full-text articles were retrieved and screened. A further 219 papers were excluded for not meeting the inclusion criteria, resulting in 39 papers being included.
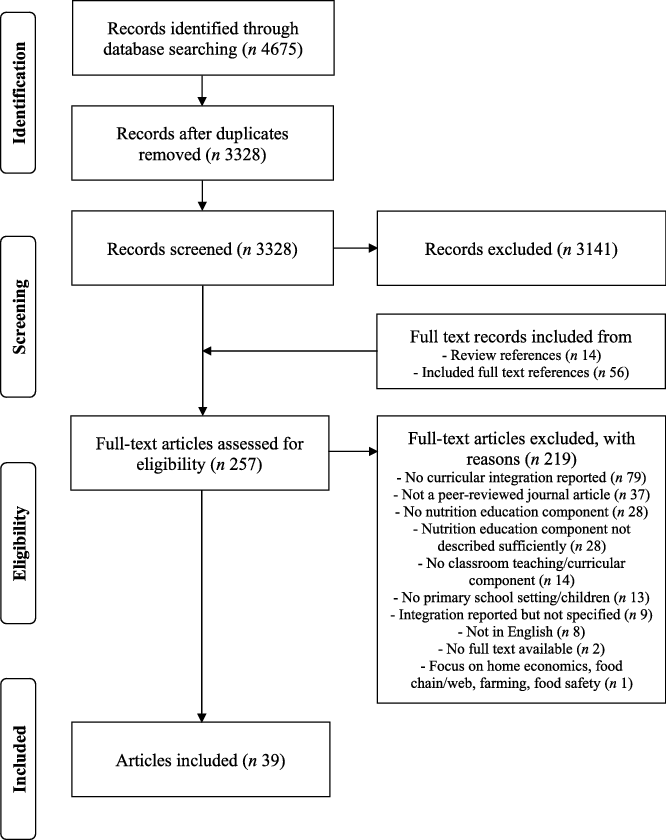
Fig. 1. PRISMA flowchart illustrating study selection for a scoping review on the integration of nutrition education into the primary school curriculum.
Duplication and inconsistencies in reporting
Several included articles were based on the same study population and/or intervention but addressed different study outcomes. Therefore, the individual articles were organised according to the intervention study and overall programme that they described to synthesise and present findings without duplication. Twenty-four individual programmes were identified, with each programme being used within one or more intervention studies that were described by at least one publication (Table 2).
Findings from multiple publications on the same trial and programme were combined to prevent duplication and to provide an overview that is as complete as possible. As such, when one article on a particular study did not report on the lesson frequency, but another article on the same study did include this information, the same lesson frequency was reported for both articles. In contrast, some papers on the same intervention provided inconsistent information on the data extracted. For instance, articles describing the same population reported a different number of included students due to these articles examining different outcomes. As a result of the inconsistent reporting of the data that were extracted for this review, discrepancies were not grouped but included separately in the table.
Programme, study and article characteristics
All thirty-nine of the included articles are presented in Table 2, and grouped by intervention programme to provide a complete overview of the literature. Table 2 provides a detailed description of the programme characteristics per study including author(s), year, country, study design, target population, intervention length, lesson frequency and duration, nutrition-related topics, curricular integration, intervention delivery, teacher training and theories used. Note that the characteristics were grouped at different levels throughout the text, including programme, study and publication level (Table 3). The final sample included eleven cluster randomised controlled trials, fifteen quasi-experimental trials and two repeated measures/pre–post trials. Papers on nutrition integration were published as early as 1974(Reference Head40). There seemed to be a publication gap between 1985 and 1998, with the topic becoming increasingly popular from 2009 until now. The nutrition programmes were conducted in eight different countries, with most being conducted in the USA (17 out of 24)(Reference Pittman, Bland and Cabrera31,Reference Head40–Reference Gortmaker, Cheung and Peterson68) . Included studies almost solely examined primary school aged children, with only one study investigating outcomes related to higher educational stages(Reference Head40). Except for the number of participating students in this study, all data were extracted from the primary school grades only. Integrative nutrition education interventions were developed for a variety of school settings such as single grades, multiple grades or whole primary or elementary schools. These programmes most often targeted fourth or fifth grade students (n = 13 and n = 12, respectively). The longest intervention length was 2 years, compared with the shortest intervention trial of 3 weeks. Additionally, twelve studies included only an education intervention component(Reference Head40,Reference Webb and Rule45,Reference Roseno, Carraway-Stage and Hoerdeman47–Reference Duffrin, Hovland and Carraway-Stage51,Reference Meyers and Jansen58,Reference Jakubowski, Perron and Farrell59,Reference Keihner, Meigs and Sugerman63,Reference Wall, Least and Gromis67,Reference Francis, Nichols and Dalrymple69–Reference Tilles-Tirkkonen, Nuutinen and Sinikallio72) , whilst sixteen studies were part of a larger intervention involving multiple components (e.g. school garden, school policies, parental involvement, school canteens)(Reference Pittman, Bland and Cabrera31,Reference Belansky, Romaniello and Morin41–Reference Auld, Romaniello and Heimendinger44,Reference Tinsley, Houtkooper and Engle46,Reference Koch, Contento and Gray52–Reference Scherr, Linnell and Dharmar57,Reference Foster, Sherman and Borradaile60–Reference Foerster, Gregson and Beall62,Reference Morris, Briggs and Zidenberg-Cherr64–Reference Morris, Koumjian and Briggs66,Reference Gortmaker, Cheung and Peterson68,Reference Taylor, McAuley and Barbezat73–Reference Fairclough, Hackett and Davies77) . Across all twenty-four programmes, half (n = 12) did not report using a theory that supported the students’ learning. Others included at least one theory such as the social cognitive theory (n = 8), Piaget cognitive development theory/constructivist learning theory (n = 4), self-determination theory (n = 2), theory of planned behaviour (n = 1), social-ecological model (n = 1), resiliency theory (n = 1), and mastery learning model (n = 1).
Table 3. Intervention characteristics per programme or study

* Programme or study included multiple categories.
Integration of nutrition education
Nutrition topics
Of twenty-four intervention programmes, two did not specify the nutrition topics covered in their nutrition education programme(Reference Head40,Reference Foster, Sherman and Borradaile60) . The remaining programmes described a wide variety of nutrition topics such as fruit and vegetables, nutrients, sugary drinks, nutrition labels, snacking, energy balance, dietary guidelines, meal planning/management, portion/serve sizes and more. These topics can be clustered into nine main domains (nutrients, food groups, meal management, energy balance, nutrition labels, nutrition functions and lifestyle diseases, sugary drinks, portion/serve sizes and healthy eating choices). Several studies included more than one of these domains in their intervention. The majority of interventions focused on teaching students about food groups (n = 16), amongst which the fruit and vegetables group was most popular. In contrast, the domains on energy balance, nutrition labels, sugary drinks and portion/serve size were reported least frequently (n ≤ 4 for each domain).
Curricular integration
The included programmes reported integrating nutrition education with one or more subject areas (ranging from one to six). The dominant subjects for nutrition integration were mathematics (n = 17), science (n = 16), literacy (n = 16) and social studies (n = 6). A detailed description of the learning outcomes for each subject area or the integrative approach was frequently missing. Ten out of thirty-nine papers defined how the nutrition content and core curricular subjects were integrated(Reference Belansky, Romaniello and Morin41,Reference Webb and Rule45,Reference Roseno, Carraway-Stage and Hoerdeman47,Reference Hovland, Carraway-Stage and Cela49,Reference Carraway-Stage, Hovland and Showers50,Reference Jakubowski, Perron and Farrell59,Reference Johnston, Moreno and El-Mubasher61,Reference Keihner, Meigs and Sugerman63,Reference Wall, Least and Gromis67,Reference Francis, Nichols and Dalrymple69) . For example, one of the articles on the FoodMASTER initiative outlined the specific nutrition-related topics and curricular integration with the science standards for each lesson using an overview table(Reference Carraway-Stage, Hovland and Showers50). Another study by Jakubowski et al. (2018) described an example lesson illustrating its integration of nutrition and physical education to improve students’ dribbling skills and knowledge on proteins(Reference Jakubowski, Perron and Farrell59). In terms of reasoning for using an integrative approach, slightly under half of the articles justified the curricular integration of nutrition and other subjects(Reference Pittman, Bland and Cabrera31,Reference Belansky, Romaniello and Morin41,Reference Auld, Romaniello and Heimendinger43–Reference Webb and Rule45,Reference Roseno, Carraway-Stage and Hoerdeman47–Reference Koch, Contento and Gray52,Reference Johnston, Moreno and El-Mubasher61,Reference Morris, Briggs and Zidenberg-Cherr64,Reference Francis, Nichols and Dalrymple69,Reference Tilles-Tirkkonen, Nuutinen and Sinikallio72,Reference Angelopoulos, Milionis and Grammatikaki76) . Frequently used explanations included nutrition topics providing a relevant context for the students to learn about core subjects(Reference Auld, Romaniello and Heimendinger43,Reference Auld, Romaniello and Heimendinger44,Reference Roseno, Carraway-Stage and Hoerdeman47–Reference Koch, Contento and Gray52) , improving outcomes related to both nutrition and academic standards(Reference Pittman, Bland and Cabrera31,Reference Belansky, Romaniello and Morin41,Reference Webb and Rule45,Reference Carraway-Stage, Kolasa and Díaz48,Reference Carraway-Stage, Hovland and Showers50,Reference Morris, Briggs and Zidenberg-Cherr64) , and the lessons being appealing to teachers(Reference Belansky, Romaniello and Morin41,Reference Auld, Romaniello and Heimendinger43,Reference Auld, Romaniello and Heimendinger44,Reference Carraway-Stage, Kolasa and Díaz48,Reference Morris, Briggs and Zidenberg-Cherr64) by limiting time demands(Reference Pittman, Bland and Cabrera31,Reference Johnston, Moreno and El-Mubasher61,Reference Morris, Briggs and Zidenberg-Cherr64,Reference Angelopoulos, Milionis and Grammatikaki76) and not competing with core subjects(Reference Auld, Romaniello and Heimendinger43,Reference Webb and Rule45,Reference Hovland, Carraway-Stage and Cela49,Reference Johnston, Moreno and El-Mubasher61,Reference Francis, Nichols and Dalrymple69,Reference Tilles-Tirkkonen, Nuutinen and Sinikallio72) .
Lesson frequency and duration
The lesson frequency and duration between the interventions differed greatly. The number of lessons provided to students varied from four to fifty lessons across varying intervention lengths. However, some studies did not specify the lesson frequency and/or duration. Due to the lack of detail on the lesson frequency and duration, no estimation on the average lesson frequency and exposure to nutrition education for all the included studies can be obtained. For the ten interventions that did report on the number and duration of the nutrition lessons, the estimated hours that the students were exposed to nutrition education was on average approximately 24 h (range 2·7–100 h).
Intervention delivery and teacher training
Interventions were delivered by the classroom teacher (n = 17 studies), nutrition expert (n = 6 studies), or both classroom teacher and nutrition expert (n = 4 studies), or intervention delivery was not reported (n = 1 study)(Reference Taylor, McAuley and Barbezat73–Reference Taylor, McAuley and Williams75). When both classroom teacher and nutrition expert were involved, this meant that they either provided the lessons together, alternated the lesson delivery, or the classroom teacher and nutrition expert were compared between study arms. Except for two studies(Reference Pittman, Bland and Cabrera31,Reference Webb and Rule45) , classroom teachers were provided with training to implement the nutrition lessons. Professional development workshops or training sessions were often scheduled prior to implementing the lessons with several studies also supporting the teachers throughout the implementation phase. The observed intensity of these workshops was mixed, with the duration ranging from 1 h to multiple days.
Integration-related outcomes
Both qualitative and quantitative data were obtained from fifteen articles(Reference Head40,Reference Belansky, Romaniello and Morin41,Reference Auld, Romaniello and Heimendinger43,Reference Auld, Romaniello and Heimendinger44,Reference Roseno, Carraway-Stage and Hoerdeman47–Reference Duffrin, Hovland and Carraway-Stage51,Reference Jakubowski, Perron and Farrell59,Reference Gortmaker, Cheung and Peterson68–Reference Devadas, Chandrasekhar and Vasanthamani70,Reference Tilles-Tirkkonen, Nuutinen and Sinikallio72,Reference Fairclough, Hackett and Davies77) . Programme evaluations with teachers confirmed that the content was integrated with curricular standards as intended(Reference Belansky, Romaniello and Morin41,Reference Auld, Romaniello and Heimendinger43,Reference Auld, Romaniello and Heimendinger44,Reference Duffrin, Hovland and Carraway-Stage51,Reference Gortmaker, Cheung and Peterson68,Reference Tilles-Tirkkonen, Nuutinen and Sinikallio72) . The majority of the teachers who were asked about the integration perceived this strategy as valuable(Reference Auld, Romaniello and Heimendinger43), easy to implement(Reference Francis, Nichols and Dalrymple69) or feasible(Reference Gortmaker, Cheung and Peterson68,Reference Fairclough, Hackett and Davies77) , with others commenting they noticed a positive impact on their teaching time(Reference Hovland, Carraway-Stage and Cela49,Reference Francis, Nichols and Dalrymple69) . Several papers reported that the curricular activities were liked by the teachers and/or students(Reference Roseno, Carraway-Stage and Hoerdeman47,Reference Gortmaker, Cheung and Peterson68,Reference Francis, Nichols and Dalrymple69) . However, two articles stated that teachers expressed the need for a more explicit connection between nutrition and core subjects(Reference Duffrin, Hovland and Carraway-Stage51,Reference Tilles-Tirkkonen, Nuutinen and Sinikallio72) . Where studies compared the integrated approach without implementing other intervention components to usual teaching practices, some observed positive effects on nutrition-related outcomes such as nutrition knowledge(Reference Head40,Reference Carraway-Stage, Hovland and Showers50,Reference Devadas, Chandrasekhar and Vasanthamani70) or healthy food choices(Reference Jakubowski, Perron and Farrell59). Furthermore, multiple papers on the FoodMASTER programme provided evidence for the improvement of academic outcomes including mathematics and science knowledge as a result of the integration(Reference Roseno, Carraway-Stage and Hoerdeman47–Reference Hovland, Carraway-Stage and Cela49).
Discussion
This scoping review aimed to summarise peer-reviewed programmes or interventions that were designed to integrate nutrition content with core subjects of the primary school curriculum. Findings highlight that the included studies are heterogeneous in terms of nutrition topics covered, subject integration, programme delivery, intervention components and level of detail provided in the programme description. The majority of studies implemented an educational programme on fruit and vegetables (food groups) and researchers primarily integrated nutrition with mathematics, science and literacy. Overall, the effectiveness of an integrative approach to teach nutrition in primary schools remains unclear.
Nutrition topics
Out of nine nutrition-related domains, teaching about food groups, and fruit and vegetables specifically, was observed as the most popular topic. This is not surprising as many national nutrition guidelines state the importance of eating a variety of foods from different food groups, with an emphasis on the consumption of fruit and vegetables(78). A large proportion of children and adolescents worldwide do not meet fruit and vegetable intake recommendations(Reference Mihrshahi, Myton and Partridge79–Reference Albani, Butler and Traill83), and low intake of fruit and vegetables is associated with a high risk of mortality and chronic diseases(Reference Wang, Ouyang and Liu8). It is therefore essential to continue promoting the consumption and knowledge of the health effects of fruit and vegetables through nutrition education interventions.
In line with our findings, teachers identified food groups as a commonly taught nutrition topic in the classroom(Reference Murimi, Sample and Guthrie84). This is considered developmentally appropriate and easy to understand for primary-school-aged children(Reference Eliassen and Wilson85). Similar to our observations that some nutrition topics are less frequently used in nutrition education interventions, results from an online survey by de Vlieger et al. (2019) show that teachers themselves spent less time on topics such as energy balance, lifestyle diseases, fast food, salt intake, sugar intake and fat intake(Reference de Vlieger, Riley and Miller33). Early primary school children may not be able to comprehend abstract concepts like energy, vitamins or protein(Reference Eliassen and Wilson85). Nevertheless, nutrition topics other than food groups may be just as important given that large amounts of sugar-sweetened beverages, high-fat foods, fast food, frequent snacking and large portion sizes are related to obesity or chronic diseases(5,Reference Moreno and Rodríguez6,Reference Sahoo, Sahoo and Choudhury86–Reference Swinburn, Caterson and Seidell88) . Future studies may need to provide education on a broad scope of nutrition topics supporting all dietary guidelines and that are age appropriate for the target population to improve overall healthy eating habits.
Curricular integration
Our findings suggest that nutrition, science, mathematics and literacy subjects are commonly used for multidisciplinary teaching. The potential for integrating nutrition into the mathematics and science syllabus due to a coherent link between these subjects has been discussed regularly(Reference Follong, Prieto-Rodriguez and Miller23,Reference Perera, Frei and Frei30,Reference Carraway-Stage, Kolasa and Díaz48,Reference Eliassen and Wilson85,Reference Coulson, Eiser and Eiser89–Reference Miller92) . In 1998, James and Adams highlighted that an integrative nutrition and mathematics curriculum could contribute to a child’s problem solving, reasoning, mathematical connections, and procedural and conceptual mathematics knowledge. At the same time, it may improve knowledge and skills related to nutrition and healthy eating(Reference James and Adams90). Nutrition concepts can easily be used to contextualise mathematics and science content, as it provides real-life examples that students can relate to(Reference Roseno, Carraway-Stage and Hoerdeman47,Reference Carraway-Stage, Kolasa and Díaz48,Reference Miller92–Reference Duffrin, Cuson and Phillips95) . Findings from the FoodMASTER initiative provide evidence for the positive association between nutrition, mathematics and science knowledge(Reference Carraway-Stage, Kolasa and Díaz48). Since academic achievement tests in mathematics, literacy and science are often mandatory, instruction time on these core subjects is prioritised(Reference Hall, Chai and Albrecht26,Reference Perera, Frei and Frei30,Reference Smith and Kovacs96) . Teachers may benefit from efficient use of class time and being able to meet curricular standards(Reference Carraway-Stage, Kolasa and Díaz48). Teaching nutrition through mathematics, literacy and science might therefore have the greatest potential of reducing the pressure on teachers to choose between academic success and the importance of nutrition education.
Although the results seem to point to one direction, extracting the data in regard to nutrition integration was challenging for a number of reasons. All twenty-eight studies included information on the curricular subject integration of the nutrition programmes; however, the level of detail varied considerably. The majority of included papers only provide a limited description of the approach and do not specify what is considered an integrative teaching strategy. Curriculum descriptions typically include the objectives, main topics, frequency and duration of activities, and behaviour theories used(Reference Waters, de Silva-Sanigorski and Burford19,Reference Linnell, Zidenberg-Cherr and Briggs97) . Development processes and the use of specific approaches are often minimally discussed(Reference Linnell, Zidenberg-Cherr and Briggs97). This might have resulted in missing or incomplete data extraction from the included publications or potentially excluding relevant articles. To minimise the exclusion of relevant articles, we identified related sources such as programme webpages or protocol papers to complement the data extraction. No additional sources were found for several papers on nutrition integration that did not specify the curricular subjects. These studies generally stated integrating the nutrition content within the primary school curriculum or education standards. Although acknowledging the fact that these studies used an integrative approach, they were excluded from the review(Reference Llargues, Franco and Recasens98–Reference Ekwaru, Ohinmaa and Tran106). Not only does a limited programme description affect the selection process or data extraction, comparison and replication of these nutrition curricula also becomes extremely difficult. Notably, this shows the importance of defining the concept of integration or cross-curriculum when developing and reporting on such an approach. To avoid misinterpretation and to prevent these issues from occurring in the future, authors should consider clearly defining their integrative approach and including detailed information on the curricular practices.
Integration-related outcomes
Although the integration has been intentional and explicitly mentioned within the included studies, the research aim might not have been to investigate outcomes related to the integration itself. Additionally, the numerous multicomponent interventions included still does not allow for a conclusion on the effectiveness of the integrative approach, but rather on the overall effect of the intervention. This might explain why most study outcomes were not related to the integration, but more so to the overall effectiveness of the intervention. Therefore, only limited data could be extracted on the integration-related outcomes, and no conclusions on a potential causal relation could be drawn.
Several studies collected data through interviews and questionnaires to examine teachers’ and/or students’ perspectives on an integrative approach and how this affected their teaching practices and/or learning experiences(Reference Auld, Romaniello and Heimendinger43,Reference Roseno, Carraway-Stage and Hoerdeman47,Reference Duffrin, Hovland and Carraway-Stage51,Reference Gortmaker, Cheung and Peterson68,Reference Francis, Nichols and Dalrymple69,Reference Tilles-Tirkkonen, Nuutinen and Sinikallio72,Reference Fairclough, Hackett and Davies77) . In general, the integration of nutrition into the curriculum was positively received by both the teachers and students. However, some teachers still highlighted that the activities needed a stronger connection to the school curriculum(Reference Duffrin, Hovland and Carraway-Stage51,Reference Tilles-Tirkkonen, Nuutinen and Sinikallio72) . As the description of the integration is often lacking, it is hard to determine to what extent the programme was integrated and, therefore, the degree to which this influenced the teacher’s time constraints or students’ learning. Furthermore, only one programme discussed the outcomes related to academic performance of the core subjects(Reference Roseno, Carraway-Stage and Hoerdeman47–Reference Hovland, Carraway-Stage and Cela49). When using an integrative approach, it is important to take into account both nutrition- and academic-related outcomes(Reference Shilts, Lamp and Horowitz107,Reference Campbell, Rawlins and Wells108) . Multiple papers on the FoodMASTER initiative suggest that a food-based science curriculum could improve students’ nutrition knowledge, science knowledge and mathematics achievements. Their findings provide evidence for the effectiveness of integrative teaching on students’ academic performances. In addition, all programmes, except for one(Reference Jakubowski, Perron and Farrell59), reported a positive impact of integrative nutrition education on children’s nutrition knowledge(Reference Head40,Reference Carraway-Stage, Hovland and Showers50,Reference Devadas, Chandrasekhar and Vasanthamani70) . Despite these promising findings, the programmes had large methodological differences, which prevents comparison and limits interpretation of the effectiveness in regard to nutrition knowledge. Other nutrition-related outcomes such as dietary intakes or food purchases and long-term effects relating to health and wellbeing remain unexplored.
A previous systematic review exploring teaching strategies to educate primary school children on healthy eating included multiple papers that implemented a cross-curricular approach (i.e. ‘nutrition education programs that were delivered across two or more traditional primary school subjects’)(Reference Dudley, Cotton and Peralta12). Some of these articles met all our inclusion criteria, except for having the nutrition education component integrated. Only articles that explicitly integrated nutrition within the curriculum and that reported on the curricular subjects were included in our review, which might explain the discrepancy in included publications and subsequently the conclusions on the effectiveness of this approach. According to Dudley et al. (2015), embedding this teaching strategy within healthy eating interventions could improve primary-school-aged children’s fruit and vegetable consumption or preference, and it might reduce their consumption of sugar-sweetened drinks or fruit juice(Reference Dudley, Cotton and Peralta12). However, the calculated effect size of these nutrition-related outcomes was based on interventions that included multiple strategies. These effect sizes might therefore not reflect the effectiveness of the nutrition integration alone. Hence, more research is needed on the effectiveness of nutrition integration within core subjects. Future studies are recommended that report on outcomes related to health and nutrition, academic achievements, teacher and student perspectives in terms of the whole intervention and integration, and its effect on teachers’ time constraints using both quantitative and qualitative methods.
Intervention length, lesson frequency and duration
Similar to other data extracted, issues arose when analysing our findings on intervention length, lesson frequency and duration. The information obtained was not well described and extremely heterogeneous. For behaviour change to occur, a minimum intervention length of 6 months is suggested(Reference Sharma109–Reference Murimi, Moyeda-Carabaza and Nguyen111). Half of the studies within this review were conducted over at least 6 months, including multiple interventions that ran for 1 or 2 academic years. Although these interventions were implemented for a sufficient amount of time, their lesson intensity (frequency and duration) may have not met the suggested 50 h of nutrition education to achieve better dietary patterns(Reference Connell, Turner and Mason112). With, on average, 24 h of nutrition education, students appear to not receive the intensity needed. Only Foster et al. (2008) were able to provide the recommended intensity, with 100 h across 2 academic years(Reference Foster, Sherman and Borradaile60). Considering all the above, it is fundamental to report on both the lesson duration and frequency to determine how this might impact the intervention effectiveness.
Intervention delivery and teacher training
The included nutrition interventions were delivered mainly in classroom settings by the teacher. A previous Cochrane review found that approximately as many interventions were delivered by a nutrition expert as compared with the classroom teacher(Reference Waters, de Silva-Sanigorski and Burford19). This difference in findings might indicate that, when an integrative approach is used, classroom teachers are preferred over nutrition experts. Three of the studies included in this review compared the implementation of nutrition education between the classroom teacher and nutrition expert(Reference Belansky, Romaniello and Morin41,Reference Devadas, Chandrasekhar and Vasanthamani70,Reference Panunzio, Antoniciello and Pisano71) . Results from these studies on the delivery of integrative nutrition lessons were inconclusive.
Although the implementation through resource teachers or nutrition experts may be beneficial for certain aspects of teaching, it also means that this person enters and leaves the room within a nutrition context and integration does not occur in a pure form(Reference Auld, Romaniello and Heimendinger43). In comparison, classroom teachers have the opportunity to integrate nutrition concepts through all their lessons and activities(Reference Panunzio, Antoniciello and Pisano71), they are able to tailor the content to their students’ needs and abilities(Reference Hall, Chai and Albrecht26), and they might act as greater role models than an outside teacher(Reference Perikkou, Kokkinou and Panagiotakos113). Another key role the classroom teacher could play is in developing the teaching unit. Research highlights that collaborating with teachers to develop educational resources could improve credibility, feasibility, promotion and uptake(Reference Love, Booth and Margerison32). Thus, previous research and our findings highlight the significance of teacher involvement in the development and implementation of integrated nutrition lessons. To draw firm conclusions on the best type of delivery for integrative teaching practices, future research is needed to compare the effectiveness of classroom and resource teachers.
When primary school teachers implement the intervention, it is essential that they are supported or trained to feel competent and confident to teach nutrition content(Reference Peralta, Dudley and Cotton34,Reference Dunn, Burgermaster and Adams114) . Multiple studies reported that teacher training could significantly improve teachers’ self-efficacy towards teaching nutrition(Reference Carraway-Stage, Roseno and Hodges115,Reference Fahlman, McCaughtry and Martin116) . Subsequently, possessing high levels of self-efficacy has been associated with more time spent teaching nutrition(Reference Carraway-Stage, Roseno and Hodges115,Reference Britten and Lai117,Reference Metos, Sarnoff and Jordan118) , delivery of effective nutrition education(Reference Carraway-Stage, Roseno and Hodges115) and enhanced programme implementation(Reference Fahlman, McCaughtry and Martin116). The level of support or training in the included studies ranged from 1-h sessions to extensive professional development courses over several weeks. In line with a recent review on the content analysis of classroom teacher professional development for nutrition education interventions, few studies described strategies used in these workshops and reported only on elements like the duration of the training and follow-up sessions throughout or after the programme(Reference Dunn, Burgermaster and Adams114). Due to inconsistencies and lack of detail in the reporting of teacher support or training, and the heterogeneity of the programmes in general, a conclusion cannot be drawn on the appropriate level of support or training to deliver high-quality nutrition education. Although teacher training and support has been identified as important(Reference Wang and Stewart20,Reference Sadegholvad, Yeatman and Parrish119,Reference Nanayakkara, Margerison and Worsley120) , more research is needed on the level of support or training required to teach nutrition using integrative strategies(Reference de Vlieger, Riley and Miller33,Reference Peralta, Dudley and Cotton34,Reference Dunn, Burgermaster and Adams114) .
Theoretical framework
Of the included programmes that involved a theoretical framework, many based their intervention content or strategies on the social cognitive theory. This is in line with other reviews identifying that this theory has been most widely used in nutrition education interventions to improve individuals’ health-related behaviour(Reference Dudley, Cotton and Peralta12,Reference Sharma109,Reference Contento, Balch and Bronner121,Reference Hoelscher, Evans and Parcel122) . The development and implementation of nutrition interventions using a theoretical foundation has been shown to increase intervention effectiveness(Reference Sharma110,Reference Contento, Balch and Bronner121–Reference Baranowski, Cullen and Nicklas123) . With half of the programmes not reporting the use of a theoretical framework, researchers should be encouraged to design theory-based nutrition education interventions in the future.
Population and age
Although this review primarily includes studies in primary schools, the results show that the interventions have been conducted particularly with grade 4 or 5 students. Kropski et al. (2008) observed a similar age distribution, with most interventions targeting children between 7 and 10 years old(Reference Kropski, Keckley and Jensen124). Children between 8 and 12 years of age start to develop food preferences and dietary habits that become more resistant to change when entering middle school(Reference Winter, Stanton and Boushey125,Reference Kelder, Perry and Klepp126) . In this age range, children are also able to understand the health benefits of foods because of their cognitive development(Reference Zeinstra, Koelen and Kok127). Furthermore, research indicates that persistent obesity is established before the age of 11 years and that preventative measures should therefore target children in their early years(Reference Wardle, Brodersen and Cole128). Although the middle-to-upper primary school years have been determined as the appropriate target age for school-based nutrition education, interventions ideally should target all children using sequential Kindergarten-to-grade-6 nutrition education programmes that include different activities for each grade level(Reference Sharma109,Reference Murimi, Moyeda-Carabaza and Nguyen111) .
Strengths and limitations
There are multiple strengths of this scoping review. To the best of our knowledge, this is the first study to explore evidence-based nutrition integration programmes in primary schools. Given this review included many different forms of interventions and outcomes, a comprehensive overview of the current available literature has been presented. Furthermore, over-representation of our findings was prevented by taking into account the fact that articles might be linked at the intervention and programme level.
This scoping review has several limitations that need to be addressed. This type of review provides a less in-depth evaluation of the literature compared with a systematic review. Furthermore, the methodological quality and risk of bias were not assessed. Despite the fact that these critical aspects were not taken into account, this review provides insights into the breadth of current evidence on nutrition integration in primary schools. Critical research gaps and methodological issues have been identified and can inform future interventions. Of note is that data extraction was based solely on what was described in the article, related protocol papers or online sources, and was not verified with the authors. It is possible that excluded articles might have used an integrative approach which could not be identified from the text or these other sources. The review therefore strictly included papers that explicitly reported on the integration of nutrition in the school curriculum. Additionally, the heterogeneity of primary-school-based nutrition interventions is large. This resulted in a limited ability to compare studies and to examine the effectiveness of integrative teaching in nutrition programmes. This is not surprising given the exploratory nature of this scoping review. Allowing the inclusion of multicomponent school interventions, results might not reflect the impact of solely the integrative approach but rather a combination of intervention components. Although most papers described each component separately in their method section, not all data extracted could be exclusively linked to the curricular component.
Conclusions
Nutrition education programmes integrated into a variety of core subjects of the primary school curriculum have been widely implemented. Although integrating nutrition into the curriculum has been proposed as a way to address teachers’ time constraints, to date, evidence available to support this claim is scarce. Only limited research suggests that students’ academic performances or healthy eating knowledge could be improved. Hence, more research is needed to provide evidence on the effectiveness of integrative nutrition curricula with regard to nutrition or health-related outcomes, academic achievement and teachers’ time barriers. Furthermore, comprehensive programme evaluations including both teachers’ and students’ perceptions are needed. Future interventions should consider embedding a variety of age-appropriate nutrition subjects, defining and outlining the integrative approach, designing the curriculum based on a theoretical framework, offering teacher support and training, and implementation by teachers. Each of these elements should be described sufficiently to allow for the comparison and replication of effective interventions. Additionally, the current review provides initial support for exploring the use of more standardised approaches and/or policies related to teaching nutrition in the curriculum. This could assist in helping to reduce heterogeneity and, therefore, limitations encountered when evaluating effectiveness of classroom nutrition interventions. While research progresses to identify best practice in using this promising teaching strategy, high-quality interventions are needed before conclusions can be made as to whether implementing integrative nutrition education programmes in primary schools is a successful strategy.
Acknowledgements
We would like to acknowledge Debbie Booth (The University of Newcastle’s Librarian) for her support with creating the search terms and conducting the database searches.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflict of Interest
None.
Authorship
B.M.F., E.P., A.M., C.E.C. and T.B. conceived the study aim and design. B.M.F. designed the search strategy and conducted the database searches. B.M.F., A.V., E.P., A.M., C.E.C. and T.B. screened records. Data were extracted and analysed by B.M.F. B.M.F. drafted the manuscript, and all authors contributed to processes related to reviewing and editing the final manuscript. The final version of the paper has been approved by all authors.







