Published online by Cambridge University Press: 01 May 2004
The social outcomes of pediatric traumatic brain injury (TBI) were examined in a prospective, longitudinal study that included 53 children with severe TBI, 56 with moderate TBI, and 80 with orthopedic injuries, recruited between 6 and 12 years of age. Child and family functioning were assessed at baseline, at 6- and 12-month follow-ups, and at an extended follow-up a mean of 4 years post injury. Growth curve analyses revealed that pediatric TBI yields negative social outcomes that are exacerbated by family environments characterized by lower socioeconomic status, fewer family resources, and poorer family functioning. After controlling for group membership, age, race, socioeconomic status, and IQ, path analyses indicated that long-term social outcomes were accounted for in part by specific neurocognitive skills, including executive functions and pragmatic language, and by social problem-solving. Deficits in these domains among children with TBI are likely to reflect damage to a network of brain regions that have been implicated in social cognition. (JINS, 2004, 10, 412–426.)
Traumatic brain injuries (TBI) in children result in a variety of negative sequelae. Research has shown that TBI are likely to result in cognitive deficits, behavioral problems, poor school performance, and declines in adaptive behavior, especially among children with more severe injuries (Yeates, 2000). However, surprisingly little is known regarding the impact of TBI on children's social functioning, despite the importance of social competence as a predictor of a wide variety of outcomes, including psychological adjustment, academic performance, and health status (House et al., 1988; Rubin et al., 1998). Given the developmental significance of social competence, poor social outcomes could play a major role in the reductions in quality of life reported following childhood TBI (Stancin et al., 2002).
Several different lines of research suggest that children with TBI are likely to demonstrate poor social outcomes. First, children with chronic health conditions affecting the central nervous system, such as epilepsy and cerebral palsy, are rated as less socially accepted and less socially competent than peers (Nassau & Drotar, 1997). Second, recent research regarding the neural substrates of social cognition has implicated a network of predominantly frontal and temporal brain regions (Adolphs, 2001; Grady & Keightley, 2002) that also have been shown to be especially likely to be damaged in pediatric TBI (Levin et al., 1989; Mendelsohn et al., 1992). Third, the few existing studies of social outcomes in childhood TBI have shown that children with severe TBI are rated as less socially competent and more lonely than healthy children or children with injuries not involving the brain (Andrews et al., 1998; Bohnert et al., 1997; Dennis et al., 2001; Max et al., 1998; McGuire & Rothenberg, 1986; Papero et al., 1993).
As part of a recent paper regarding the impact of pediatric TBI on behavior and academic achievement (Taylor et al., 2002), we examined a specific social outcome measure, namely the Socialization scale of the Vineland Adaptive Behavior Scales (VABS; Sparrow et al., 1984). The measure was included in a larger prospective, longitudinal study that involved children with severe TBI, moderate TBI, and orthopedic injuries not involving the head. Preinjury child and family status were assessed retrospectively shortly after the injury, and post-injury child and family functioning were measured at 6 and 12 months post injury and again at an extended follow-up on average 4 years post injury. A mixed model analysis of the VABS Socialization scale revealed a significant interaction involving Group Membership × Socioeconomic Status × Short-Term Change (i.e., from 6 to 12 months post injury). Group differences, which were minimal at the 6 month assessment, increased from the 6 to 12 month assessment, but only for children from families of lower socioeconomic status. Children from families of lower socioeconomic status showed declines in Socialization scores in the TBI groups but not in the OI group. In contrast, children from families of higher socioeconomic status showed increases in Socialization scores in all three groups. The results demonstrate the importance of studying social outcomes in a prospective, longitudinal fashion, to investigate patterns of intraindividual growth (Fletcher et al., 1995). They also indicate that the family environment is likely to play an important role in influencing social outcomes following pediatric TBI, consistent with developmental research implicating parenting and the family environment as determinants of children's social functioning (Parker et al., 1995). However, further studies are needed to determine if the findings generalize to measures of social outcomes other than the VABS Socialization scale.
Studies are also needed regarding the neuropsychological correlates of social functioning following childhood TBI. Although neuropsychological deficits have been proposed as a likely cause of social problems following TBI (McGann & Werven, 1995; McGann et al., 1997), few studies have examined the nature of the relationship between neuropsychological and social functioning in children with TBI, and the results from those studies have been inconsistent (Dennis et al., 2001; Papero et al., 1993). The limited available literature suggests that deficits in executive functions, particularly inhibitory control, and in pragmatic language and discourse skills are likely to be predictive of social outcomes following TBI (Dennis et al., 2001). However, the specificity of these relationships is unclear, because previous research has not determined whether deficits in specific neurocognitive domains account for social outcomes over and above general intellectual functioning.
The inconsistent findings regarding the relationship between neuropsychological functioning and social outcomes following TBI may stem from a failure to consider the mechanism by which neurocognitive abilities affect social behavior. One possibility is that the influence of neuropsychological functioning on social outcomes is mediated by children's social problem-solving skills. Previous research has shown that children with TBI display deficits in social information-processing that predict their social and academic outcomes (Janusz et al., 2002; Warschausky et al., 1997). Moreover, social problem-solving has been shown to predict social outcomes in children with TBI even when controlling for general intellectual functioning (Janusz et al., 2002). Recent models of social competence suggest that social problem-solving is a proximal determinant of social behavior that is influenced by core neurocognitive abilities, such as executive functions and pragmatic language (Dodge et al., 2002; Guralnick, 1999; Lemerise & Arsenio, 2000). However, the validity of these models has not been tested in children with TBI.
The major goal of the current study, therefore, was to investigate social outcomes following childhood TBI. We used data collected during our prospective study, which included children with moderate to severe TBI and children with orthopedic injuries not involving the brain, as well as their families (Taylor et al., 1995). Our first specific aim was to determine the relationship of TBI severity and the family environment to short- and long-term changes in children's social functioning, using measures of social outcomes not examined by us previously (Taylor et al., 2002). We hypothesized that children with TBI would show poorer social outcomes than children with injuries not involving the brain. We expected that the magnitude of social deficits would vary as a function of the severity of TBI, with more pronounced deficits in children with severe as compared to moderate TBI or orthopedic injuries. We also expected that the family environment would moderate the impact of injury severity, such that family dysfunction would exacerbate the impact of TBI on children's social functioning.
Our second specific aim was to determine the concurrent relationship of cognitive and social–cognitive skills to long-term social outcomes. Specifically, we wanted to examine the contribution of both cognitive skills and social problem-solving to the prediction of social functioning. We focused on executive function and pragmatic language as specific cognitive skills based on previous evidence linking them to social problem-solving and social functioning (Dennis et al., 2001; Dodge et al., 2002; Guralnick, 1999; Lemerise & Arsenio, 2000). We hypothesized that measures of the three domains would jointly account for significant variance in social outcomes, even after controlling for group membership, age, race, socioeconomic status, and overall cognitive ability. We also predicted that social problem-solving would mediate the influence of executive function and pragmatic language on social outcomes, consistent with recent models of social competence (Dodge et al., 2002; Guralnick, 1999; Lemerise & Arsenio, 2000).
The study used a concurrent cohort, prospective design. Children with moderate to severe TBI or orthopedic injuries (OI) not involving brain insult were recruited at the time of hospitalization for their injuries. Children and their families were invited to participate only after the children were medically stable and parents gave informed consent. The OI group was included to allow comparison of the consequences of TBI to the consequences of traumatic injuries more generally. Comparison with the OI group also controlled for preinjury factors related to the likelihood of accidental injury and for the experience of hospitalization.
Children and their parents were assessed shortly after hospitalization (baseline), 6 and 12 months post-injury, and at an extended follow-up that occurred on average 4.10 years post injury (range 2.37–5.84 years, SD = 0.91). Measures of the family environment and of children's social outcomes were completed by the child's primary caregiver, usually the mother. At the baseline assessment, caregivers rated children's social functioning retrospectively, to assess premorbid status. At the extended follow-up, children completed measures of overall cognitive ability, executive function, pragmatic language, and social problem-solving.
The original study sample included 189 children recruited from four hospitals in northern and central Ohio, including 53 with severe TBI, 56 with moderate TBI, and 80 with OI only. Recruitment criteria included: (1) hospitalization for at least one night for moderate to severe TBI, with or without OI, or for OI only; (2) age at injury from 6 to 12 years; (3) no indications of previous neurological disorder or child abuse; and (3) residence in an English-speaking household. Children were not excluded for premorbid learning disabilities, attention problems, or behavior disorders, because one of the primary goals of the original project was to examine how non-injury related factors, including children's preinjury functioning, affect the outcomes of pediatric TBI (Taylor et al., 1995).
Consistent with previous reports (Taylor et al., 2002; Yeates et al., 2002), severe TBI was defined by the lowest post-resuscitation Glasgow Coma Scale (GCS; Teasdale & Jennett, 1974) score of 8 or less. Moderate TBI was defined as a GCS score of 9 to 12, or a score of 13 to 15 accompanied by skull fracture, intracranial lesion, or diffuse cerebral swelling on routine clinical neuroimaging; posttraumatic neurologic abnormality; or loss of consciousness greater than 15 min. In the final sample, all children with TBI had a GCS of 12 or less, intracranial abnormalities on neuroimaging, or a sustained loss of consciousness. Only children with injuries resulting from blunt head trauma were included in the sample. Many children with TBI also had orthopedic injuries; however, children were excluded from the OI group if they demonstrated evidence of possible brain injury (e.g., symptoms of concussion, severe facial trauma).
Table 1 summarizes group characteristics at the baseline assessment. The groups were similar in terms of age at injury. The OI group had proportionally fewer White children than the TBI groups. The racial imbalance may have reflected differences in emergency transport patterns in the cities where the study occurred. The groups did not differ in socioeconomic status. As expected, the two TBI groups differed markedly in injury severity. The OI group had longer hospitalizations and more severe injuries to body regions other than the head than the moderate TBI group. Length of hospitalization and severity of non-head injuries were similar in the severe TBI and OI groups.
Sample characteristics at the baseline assessment (total sample recruited)

Table 2 presents information on group composition and attrition at each of the follow-ups. The groups did not differ in the average time elapsed between baseline and follow-up assessments. Attrition occurred primarily because of family moves, unwillingness to continue with the study, and multiple missed appointments. Children participating in the extended follow-up did not differ from those who had dropped out in age at injury, sex or ethnic distribution, measures of premorbid child and family functioning, or post-injury neuropsychological test results obtained at baseline. However, attrition was higher in the OI group, and dropouts in all groups had lower family socioeconomic status than children who remained in the study. Similar differences were found when comparing children who dropped out at the 6- or 12-month assessments to children who remained in the study at those times.
Sample composition, child ages, and baseline to follow-up intervals at each follow-up

Social functioning was assessed using the Social Competence and Social Problems subscales from the Child Behavior Checklist (CBCL; Achenbach, 1991) and the Socialization scale from the Vineland Adaptive Behavior Scales (VABS; Sparrow et al., 1984). The CBCL and VABS are widely used, standardized instruments that have demonstrated satisfactory reliability and validity (Bérubé & Achenbach, 2003; Kamphaus, 1987). Both measures were completed by parents. The Social Competence subscale from the CBCL assesses children's participation in peer-group activities, number of friends and frequency of contact with them, and ability to get along with siblings, other children, and parents. Higher scores represent better functioning. The CBCL Social Problem subscale assesses a variety of difficulties that children may encounter in their relationships with peers and adults, including psychological distress arising from those relationships. Higher scores represent poorer functioning. The VABS Socialization scale focuses on the quality of children's interpersonal relationships, participation in play and leisure activities, and compliance with social conventions. Higher scores represent better functioning.
The Socioeconomic Composite Index (SCI) provided a distal measure of the family environment. It was computed by averaging sample z scores for the Duncan Occupational Status Index (Stevens & Featherman, 1981), annual family income as coded on the Life Stressors and Social Resources Inventory–Adult Form (LISRES–A; Moos & Moos, 1994), and years of maternal education. Higher scores reflected higher socioeconomic status.
The LISRES–A was completed by parents. Scales assessing family stressors and resources provided measures of the proximal family environment. The Family Stressors score was defined as the mean of the T scores for five Stressors scales (Health, Work, Spouse, Extended Family, and Friends). The Family Resources score was computed as the mean of the T scores for four Resources scales (Work, Spouse, Extended Family, and Friends). Scores for single-parent families or for families in which parents did not work were based only on the relevant scales.
Parents also completed the Family Assessment Device (FAD; Byles et al., 1988; Miller et al., 1985) to assess overall family functioning. The FAD is a 60-item rating scale that has shown satisfactory reliability and validity in previous research. The 12-item General Functioning (FAD–GF) scale was used to provide an overall measure of family functioning, with higher scores representing greater dysfunction.
Children were administered a short form of the Wechsler Intelligence Scale for Children–Third Edition (WISC–III; Wechsler, 1991) to assess overall cognitive ability. The short form consisted of the Vocabulary, Similarities, Block Design, and Object Assembly subtests. Following procedures described by Sattler (1992), a prorated Full Scale IQ score was computed. The validity coefficient for the prorated IQ score is .94 (Sattler, 1992).
Executive function was assessed using the Contingency Naming Test (CNT; Anderson et al., 2000). The CNT is a speeded naming task that assesses verbal rule learning, working memory, inhibitory control, and cognitive flexibility. The CNT was selected from the larger battery of neuropsychological tests administered to the children because it provided the best measure of working memory and inhibition. Performance was assessed using a measure of efficiency that reflects the ratio of speed to accuracy of performance (Anderson et al., 2000). We have reported previously that the severe TBI group performs more poorly than the moderate TBI and OI groups on the CNT (Yeates et al., 2002).
Pragmatic language was assessed using the screening composite of the Test of Language Competence–Expanded Edition (TOLC; Wiig & Secord, 1989). The screening composite consists of the Oral Expression: Recreating Speech Acts and Figurative Language subtests. The Oral Expression: Recreating Speech Acts subtest assesses the ability to produce a contextually appropriate utterance using two or three key words, given a picture representing the participants and setting. The Figurative Language subtest measures the ability to interpret idioms and metaphors within a given situation, both orally and by selecting the correct meaning from among four-picture displays. Performance on the TOLC has been shown to be sensitive to the effects of childhood TBI (Dennis & Barnes, 1990).
The Interpersonal Negotiation Strategies (INS) interview (Yeates et al., 1990) was administered to assess social problem-solving. Children were presented with two hypothetical interpersonal dilemmas involving social conflicts (one with a peer, one with a parent) and asked a series of standard questions and follow-up probes to assess four social problem-solving steps (i.e., defining the problem, generating alternative strategies, selecting and implementing a specific strategy, and evaluating outcome). Interviews were audiotaped and transcribed verbatim. Answers to the interview questions were scored according to which of four developmental levels a response reflected (Schultz et al., 1988). A total score was calculated by averaging scores derived for each problem-solving step across the two stories. The interview has demonstrated satisfactory reliability and validity in previous research (Yeates et al., 1990, 1991), and the total score has been shown to be sensitive to TBI in the current sample of participants (Janusz et al., 2002).
We used general linear mixed model analysis, also referred to as hierarchical linear or growth modeling, to examine hypotheses concerning group differences in social outcomes across the four assessment occasions and their moderation by injury severity and the family environment (Burchinal et al., 1994; Jennrich & Schluchter, 1986). SAS Proc Mixed (SAS Institute, 1990) was used for data analysis. Unstructured covariance matrices were employed, allowing variances and covariances to vary across time points rather than to conform to a priori constraints. Group (severe TBI, moderate TBI, OI), sex, and race were included in the models as discrete predictors. Age, age2 (to account for nonlinear age effects), and the family variables (SCI, LISRES–A Family Stressors and Resources scales, FAD General Functioning scale) served as time-varying covariates. Because the mixed model approach is designed to assess intraindividual change or growth over time, raw scores for the social outcome measures were treated as dependent variables. Analyses were conducted only for the CBC Social Competence and Social Problems subscales, because we have presented results for the VABS Socialization scale in a previous paper (Taylor et al., 2002).
Post-injury changes in outcomes were modeled as piecewise linear splines between successive follow-ups, to represent growth over the total follow-up interval. Short-term changes were defined by splines between the 6- and 12-month follow-ups, and long-term changes by splines between the 12-month and extended follow-ups. Baseline measures of children's premorbid social functioning were included as covariates in the models. Group differences in growth were examined by testing for Group × Spline interactions. To investigate the moderating influences of family factors on group differences in change, triple interactions of group, each spline, and each family factor (SES, LSSRI stressors, LSSRI resources, FAD) were also included in the models. Models were trimmed by eliminating first higher- and then lower-level interaction terms that were not significant.
To preserve statistical power, the SCI was the only family factor included in initial models. Once models involving the SCI had been trimmed, Family Stressors and interactions of this factor with group and the splines were added to examine their effects. Models involving Family Stressors, in turn, were trimmed. Next, Family Resources were examined in a similar manner, and finally the FAD was considered. Main effects for SCI were included in all models, but main effects for Family Stressors, Family Resources, and the FAD were retained only if they or their interactions predicted outcomes independently of the SCI.
Path analyses were used to test hypotheses regarding the contributions of cognitive and social-cognitive skills to each of the social outcomes. The analyses were restricted to the extended follow-up because it was the only occasion at which the measures of pragmatic language and social problem-solving were administered. The relationships of interest are summarized in the path model depicted in Figure 1. According to this model, both cognitive and social problem-solving skills contribute to social functioning, with social problem-solving acting as a mediator. Confirmation of the model requires each of the following hypotheses to be tested (Baron & Kenny, 1986): (1) executive function and pragmatic language predict social problem-solving; (2) executive function and pragmatic language predict social outcomes; (3) social problem-solving predicts social outcomes; and (4) the association of executive function and pragmatic language with social outcomes is weaker after controlling for social problem-solving.

Hypothesized path model of relationships among executive function, pragmatic language, and social problem-solving as predictors of social outcomes.
Based on the recommendations of Holmbeck (1997), the path analyses consisted of a series of three hierarchical regression analyses conducted for each dependent variable. Group membership (coded as two dummy variables), age, race, and SCI were entered into the regression analyses first to control for demographic factors and injury severity. Then, to determine whether executive function and pragmatic language predicted social problem-solving, the INS interview total score was treated as the dependent variable, and the CNT and TOLC measures were entered as predictors in a second step. Next, to assess whether executive function and pragmatic language predicted social outcomes, analyses were conducted using each of the social outcome measures as dependent variables, and the CNT and TOLC were entered as predictors in a second step. The third set of analyses included all three cognitive and social–cognitive measures (i.e., CNT, TOLC, INS Interview) as predictors in the second step, both to assess the relationship of social-problem solving to the outcomes and to determine whether the association of executive function and pragmatic language with the outcomes was reduced after controlling for social problem-solving. We used the Sobel test to determine whether the mediational effect was significant (Holmbeck, 2002; Sobel, 1988). As a final step, we added estimated IQ as a predictor, to determine whether the cognitive and social–cognitive measures continued to account for significant variance after controlling for overall cognitive ability.
The mixed-model approach permits the inclusion of data even for participants not seen on all occasions. Therefore, growth curve analyses concerned with patterns of change in children's social outcomes included all children for whom at least one assessment was completed. However, the path analyses involved only children who had complete data available at the extended follow-up. Of the 134 children who participated in the extended follow-up, 13 were missing one or more of the requisite measures. Thus, the sample available for the path analyses consisted of 121 children, including 35 with severe TBI, 40 with moderate TBI, and 46 with OI. The groups did not differ significantly in gender, race, age at injury, age at testing, time post injury, or socioeconomic status.
The analysis of the CBCL Social Competence scale revealed a significant Group × FAD interaction [F(2,163) = 6.14, p < .01]. The severe TBI group consistently had lower scores on the Social Competence scale than the OI group, but group differences were larger in the presence of higher FAD scores. Thus, children with severe TBI had poorer social competence than children with OI, especially when their families demonstrated higher levels of dysfunction.
Some evidence for group differences in short-term change (i.e., from 6 to 12 months post injury) in social competence was found in significant interactions involving Group × Short-Term Change [F(2,163) = 3.11, p < .05] and Group × FAD × Short-Term Change [F(2,163) = 3.75, p < .05]. As shown in Figure 2, the interactions reflected an increase in the magnitude of group differences on the Social Competence scale, which occurred because the severe TBI group showed a short-term decline in their scores while the OI group showed relatively stable scores. The moderate TBI group showed a mixed pattern of change. Children from families with higher FAD scores (i.e., poorer functioning) showed short-term declines in their scores, whereas children from families with lower FAD scores showed short-term increases.

Model estimates of group means on CBCL Social Competence scale raw scores, at the 6-month, 12-month, and extended follow-ups for children with (a) high and (b) low levels of family dysfunction (i.e., those from poorer vs. better functioning families) as defined by values 1 standard deviation above and 1 standard deviation below the sample mean on the FAD General Functioning scale. The plots show an increase in the magnitude of group differences from 6 to 12 months, as well as more pronounced group differences among children from families with high levels of family dysfunction.
Scores on the CBCL Social Competence scale also were related significantly to race [F(1,163) = 5.11, p < .05], the SCI [F(1,163) = 8.13, p < .01], and the baseline rating on the Social Competence scale, which reflected premorbid functioning [F(1,163) = 89.67, p < .001]. Scores on the Social Competence scale were lower among children who were non-White, of lower socioeconomic status, and had poorer premorbid functioning.
For the CBCL Social Problems scale, the group main effect was significant [F(2,166) = 10.52, p < .001], as was the Group × Family Resources interaction [F(2,166) = 3.99, p < .05]. As Figure 3 shows, the severe TBI group had higher scores than the moderate TBI and OI groups, and group differences were larger among families with lower scores on the LISRES–A Family Resources scale. Thus, children with TBI displayed more social problems than children with OI, especially when their families had fewer social resources. No interactions involving short- or long-term change were significant. Other variables that were significant predictors of the CBCL Social Problems scale were the SCI [F(1,163) = 12.42, p < .01] and the baseline Social Problems scale rating of premorbid functioning [F(1,163) = 161.57, p < .001]. Scores were higher among children of lower socioeconomic status and those with poorer premorbid functioning.

Model estimates of group means on CBCL Social Problem scale raw scores, at the 6-month, 12-month, and extended follow-ups for children with (a) high and (b) low family resources (i.e., those from families with more or fewer resources) as defined by values one standard deviation above and one standard deviation below the sample mean on the LISRES–A Family Resources scale. The plots show greater social problems among children with severe TBI than among children with OI, with more pronounced group differences among children from families with fewer resources.
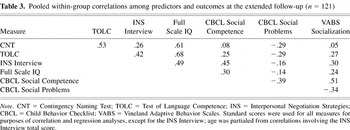
Table 3 presents the pooled within-group correlations among the measures of cognitive and social-cognitive functioning and of social outcomes at the extended follow-up. The measures of cognitive and social–cognitive skills displayed medium to large intercorrelations, as did the measures of social outcomes. The correlations between the cognitive and social-cognitive measures and the measures of social outcomes ranged from small and non-significant to medium in size.
Pooled within-group correlations among predictors and outcomes at the extended follow-up (n = 121)
Path analyses were conducted to test the model represented in Figure 1. In the first step, regression analyses were conducted using the INS interview total score as the dependent variable, with the CNT and TOLC entered as predictors in a second step, to determine whether executive function (i.e., CNT) and pragmatic language (i.e., TOLC) predicted social problem-solving (i.e., INS interview) after controlling for demographics and injury severity (see Table 4). Collectively, the two variables did not account for significant variance in the INS interview total score [F(2,112) = 2.29, p > .10], after controlling for group membership, race, SCI, and age. However, examination of the beta weights for each predictor showed that the TOLC did account for significant unique variance in the INS interview total score (t = 2.06, p < .05).
Summary of hierarchical regression analysis with CNT and TOLC as predictors of INS interview

The next set of regression analyses used each of the social outcome measures as dependent variables, and entered the CNT and TOLC as predictors, to assess whether executive function and pragmatic language predicted social outcomes (see Table 5). After controlling for demographics and injury severity, the CNT and TOLC collectively did not account for significant incremental variance in the CBCL Social Competence scale [F(2,111) = 1.18, p > .10] and neither variable accounted for unique variance. In contrast, the analysis with the CBCL Social Problems scale showed that the CNT and TOLC collectively accounted for significant incremental variance [F(2,111) = 3.72, p < .05]. Neither variable accounted for unique variance, although there was a trend for higher scores on the CNT to predict fewer social problems (t = −1.87, p < .07). For the VABS Socialization scale, the CNT and TOLC again accounted for significant incremental variance [F(2,112) = 4.95, p < .01], and the TOLC explained significant unique variance (t = 3.05, p < .01), with higher scores predicting better social functioning.
Summary of hierarchical regression analyses with CNT and TOLC as predictors of social outcomes

The third set of analyses included all three cognitive and social–cognitive measures (i.e., CNT, TOLC, INS Interview) as predictors, both to assess the relationship of social problem-solving to the outcomes and to determine whether the association of executive function and pragmatic language with the outcomes was reduced after controlling for social problem-solving (see Table 6). The INS Interview total score was a significant predictor of the CBCL Social Competence scale (t = 3.58, p < .001) but not of the CBCL Social Problems scale or the VABS Socialization scale. The CNT and TOLC continued to collectively explain significant variance in the CBCL Social Problems scale after taking the INS interview total score into account [F(2,110) = 3.35, p < .05], as well as in the VABS Socialization scale [F(2,111) = 4.09, p < .05]. In both cases, the proportion of variance for which they accounted was slightly smaller after controlling for social problem-solving (i.e., 5% vs. 6% for the CBCL Social Problems scale; 5% vs. 7% for the VABS Socialization scale). However, Sobel tests indicated that the reduction in the individual beta weights was not significant for either the CNT or the TOLC.
Summary of hierarchical regression analyses with CNT, TOLC, and INS Interview as predictors of social outcomes (Step 2 only)

As a final step, we added estimated IQ to analyses that also included the CNT, TOLC, and INS interview as predictors. The goal was to determine whether cognitive and social-cognitive measures continued to account for social outcomes after controlling for overall cognitive ability, as well as for group membership and demographics. The results of the analyses were essentially unchanged when compared to the analyses that did not include IQ as a predictor. The only change was that the CNT accounted for unique variance in the CBCL Social Problems scale after taking IQ into account (t = −2.15, p < .05). Notably, estimated IQ was not a significant predictor of any of the social outcome measures when the other cognitive and social-cognitive measures were taken into consideration.
Figure 4 summarizes the results of the path analyses in terms of the model in Figure 1. As it shows, pragmatic language was predictive of social problem-solving, but executive function was not. Pragmatic language and executive function were significant predictors of two of the three measures of social outcomes (i.e., CBCL Social Problems, VABS Socialization). Social problem-solving was a significant predictor of only one of the measures of social outcomes (i.e., CBCL Social Competence), which was not predicted by either executive function or pragmatic language. After taking social problem-solving into account, pragmatic language and executive function had a slightly weaker association with social outcomes, but the reduction in the magnitude of the relationships was not significant in either case. Thus, the findings provided little support for the hypothesis that social problem-solving mediates the effects of neuropsychological functioning on social outcomes. The analyses of the CBCL Social Competence subscale provided evidence for an indirect effect of language pragmatics on social outcomes; pragmatic language was a predictor of social problem-solving, which in turn was a predictor of the Social Competence scale. However, the indirect effect must be interpreted cautiously, and does not provide evidence of mediation because of the lack of a significant path between language pragmatics and the Social Competence scale (Holmbeck, 1997).

Path diagrams depicting the relationships among the Contingency Naming Test (CNT), Test of Language Competence (TOLC), and INS Interview as predictors of three social outcomes: (a) CBCL Social Competence; (b) CBCL Social Problems; and (c) VABS Socialization. Curved, double-arrow lines represent correlations. Single-arrow lines from variable to variable are labeled with standardized regression coefficients. Single-arrow lines to the right of the social outcome variables represent residual variances (i.e., 1 − total R2). Group membership, age, race, and SCI were treated as covariates in the path analyses. *p < .05.
As predicted, children who sustained a TBI between the ages of 6 and 12 years of age demonstrated poorer social outcomes than children with OI not involving the brain. The magnitude of group differences was a function of the severity of injury, with severe TBI leading to more negative sequelae than moderate TBI. Group differences also were exacerbated by family environments characterized by fewer family resources and poorer family functioning. The latter findings are consistent with the previous report from our group showing that socioeconomic status moderated the effect of TBI on the VABS Socialization scale (Taylor et al., 2002), and add to a growing literature indicating that the family environment moderates outcomes after childhood TBI (Chadwick et al., 1981; Gerring et al., 1998; Kinsella et al., 1999; Max et al., 1998; Rivara et al., 1993, 1994; Taylor et al., 1999, 2001, 2002; Yeates et al., 1997).
The findings do not reflect substantial recovery in social functioning over time, and in some cases reflect a worsening of outcomes. The moderating influence of the family environment affected developmental change in outcomes largely over the short term, from 6 to 12 months post injury. Group differences actually tended to widen during this time, particularly among families with poorer family functioning. Group differences stabilized after the 1st year post injury, with little evidence of any differential change (i.e., recovery) after that time. We have also found relatively little evidence of long-term recovery of cognitive or behavioral outcomes in previous reports based on our larger prospective study (Taylor et al., 2002; Yeates et al., 2002), and the current findings suggest that poor social outcomes are similarly persistent after childhood TBI.
Our results additionally indicate that the stable long-term social outcomes that occur following childhood TBI are predicted by neuropsychological abilities and social information-processing. Measures of executive function, pragmatic language, and social problem-solving made both collective and independent contributions to the prediction of social outcomes. Notably, the contributions were independent of intellectual ability, which itself did not explain variation in social outcomes after neuropsychological abilities and social information-processing were taken into account. Moreover, because cognitive skills and social problem-solving were assessed directly with the children, whereas social outcomes were assessed using parent interviews and ratings, the predictors and outcomes were not contaminated by shared method variance, so the findings are likely to be robust. The independent contributions of executive function, pragmatic language, and social problem-solving to social outcomes are consistent with recent neuroscience models of social cognition and behavior (Adolphs, 2001; Grady & Keightley, 2002). According to these models, social cognition is mediated by a distributed network of interdependent brain regions subserving discrete cognitive and affective processes that are integrated during the course of social behavior.
Contrary to our expectation, the results do not provide much evidence that social problem-solving mediates the influence of cognitive and social–cognitive abilities on social outcomes. Pragmatic language and executive function predicted a different set of social outcomes than did social problem-solving, and the strength of their association with social outcomes was not significantly weaker after taking social problem-solving into account. The lack of support for the mediation hypothesis does not invalidate recent models of social competence, which include both indirect and direct effects of core neurocognitive abilities on social outcomes (Dodge et al., 2002; Guralnick, 1999; Lemerise & Arsenio, 2000). Moreover, the substantial residual variance in the three social outcome measures signifies the need to include additional predictors in the causal model. Stronger evidence for the mediating effects of social problem-solving might be found using measures of other relevant abilities that we did not assess, such as the appreciation of intentionality or the recognition of emotional states, which may have a more direct bearing on social information-processing than executive function or pragmatic language (Dennis & Barnes, 1990; Dennis et al., 2001).
The current study was characterized by several methodological limitations. One is that a substantial number of children dropped out by the time of the extended follow-up, with disproportional attrition of children of lower socioeconomic status and those from the OI group. Attrition bias must be considered when interpreting results from longitudinal studies (Cicchetti & Nelson, 1994; Francis et al., 1994). Although attrition bias seems unlikely to have produced spurious findings in this study, the findings may not generalize to the entire population of children with TBI or accurately reflect the magnitude of environmental influences on social outcomes for the most disadvantaged families.
Other limitations involve measurement issues. The measures of the family environment used in the study are distal in nature and do not shed much light on the mechanism by which the family environment moderates social outcomes after childhood TBI (Kolb et al., 2003). Measures of more proximal aspects of the family environment, such as parenting practices and parent–child interaction (Parker et al., 1995), may provide a better understanding of how the family environment affects recovery from TBI. The use of single measures for the constructs of executive function, pragmatic language, and social problem-solving is also problematic. The constructs would be more reliably measured using multiple indicators, which could be incorporated into latent variables using structural equation modeling techniques. In turn, structural equation modeling could be used to provide a more robust test of the mediation hypothesis (Klem, 2000). Lastly, although we used multiple measures of social outcomes, all assessments were based on parent report, which are subject to bias and provide only an indirect index of social functioning. Measures of social functioning derived from parent rating scales may not be especially sensitive to the effects of TBI or other insults to the central nervous system (Drotar et al., 1995; Nassau & Drotar, 1997). A more sensitive and thorough assessment would include direct measures of social outcomes, such as peer interactions, social networks, social acceptance, behavioral reputation, and reciprocal friendships (Gest et al., 2001; Rubin et al., 1998).
A final methodological limitation is that the assessment of language pragmatics and social problem-solving was completed only once, as part of an extended follow-up on average 4 years post injury. Thus, the path analyses that examined the relationships between neuropsychological abilities, social information-processing, and social outcomes were restricted to only a single occasion. We do not know if the contributions of neuropsychological abilities and social information-processing vary as a function of the time post-injury, or if assessment of these constructs completed shortly after TBI is prognostic of longer-term social outcomes.
Despite these limitations, the current study is the first to our knowledge that examines both short- and long-term social outcomes following childhood TBI and relates social outcomes to neuropsychological abilities and social information-processing. The results demonstrate that childhood TBI lead to persistent problems in social functioning that are accounted for by multiple factors, including injury severity, specific neuropsychological and social information-processing abilities known to be vulnerable to TBI, and the family environment. One important implication of our findings is the need to consider each of these factors in evaluating risks for poor social outcomes and in understanding how social problems become entrenched following TBI. To the extent the current findings provide a better understanding of the child and family factors that predict social outcomes following TBI, they also may provide the basis for more effective intervention. Unfortunately, interventions designed to promote social competence in children with other disabilities have not been very successful (Gresham et al., 2001), and few attempts have been made to evaluate programs designed to promote the social relationships of children with TBI (Glang et al., 1997).
Future studies are needed to examine social outcomes of childhood TBI in a more comprehensive fashion, drawing on conceptual models and research methods from social neuroscience (Cacioppo et al., 2000), developmental psychology (Rubin et al., 1998), and developmental psychopathology (Masten, 2001; Parker et al., 1995; Rutter, 1999). Neuroimaging studies are needed to determine whether the damage to frontotemporal brain regions that occurs in childhood TBI helps to explain core deficits in neuropsychological abilities implicated in social cognition, including behavioral inhibition, working memory, emotion perception and regulation, and theory of mind (Adolphs, 2001; Grady & Keightley, 2002). Knowledge will also be advanced by future studies of causal models linking these core deficits in neuropsychological abilities to social problem-solving, and in turn to a broader range of social outcomes. Finally, further research is required to identify other child or family variables that act as risk or resilience factors by either impeding or promoting social adjustment after childhood TBI.
The research presented here was supported by Grant MCJ 390611 (H. Gerry Taylor) from the Maternal and Child Health Research Bureau (Title V, Social Security Act), Health Resources and Services Administration, Department of Health and Human Services, and by Grant 5 RO1 NS36335 (H. Gerry Taylor) from the National Institute of Neurological Disorders and Stroke. The authors wish to acknowledge the contributions of Matt Diamond, Marla Kemmerer, Madeline Polonia, Barbara Shapero, Elizabeth Shaver, and Nichole Wood. Special thanks also are due to the Rainbow Pediatric Trauma Center at Rainbow Babies and Children's Hospital, the Trauma Program at Children's Hospital of Columbus, and the Trauma Center at MetroHealth Medical Center. We also wish to acknowledge the participation of the Children's Hospital Medical Center of Akron and the collaboration of George Thompson and G. Dean Timmons. A preliminary version of this paper was presented at the annual meeting of the American Psychological Association in Toronto, Canada, August 2003.

Sample characteristics at the baseline assessment (total sample recruited)

Sample composition, child ages, and baseline to follow-up intervals at each follow-up

Hypothesized path model of relationships among executive function, pragmatic language, and social problem-solving as predictors of social outcomes.

Model estimates of group means on CBCL Social Competence scale raw scores, at the 6-month, 12-month, and extended follow-ups for children with (a) high and (b) low levels of family dysfunction (i.e., those from poorer vs. better functioning families) as defined by values 1 standard deviation above and 1 standard deviation below the sample mean on the FAD General Functioning scale. The plots show an increase in the magnitude of group differences from 6 to 12 months, as well as more pronounced group differences among children from families with high levels of family dysfunction.

Model estimates of group means on CBCL Social Problem scale raw scores, at the 6-month, 12-month, and extended follow-ups for children with (a) high and (b) low family resources (i.e., those from families with more or fewer resources) as defined by values one standard deviation above and one standard deviation below the sample mean on the LISRES–A Family Resources scale. The plots show greater social problems among children with severe TBI than among children with OI, with more pronounced group differences among children from families with fewer resources.

Pooled within-group correlations among predictors and outcomes at the extended follow-up (n = 121)

Summary of hierarchical regression analysis with CNT and TOLC as predictors of INS interview

Summary of hierarchical regression analyses with CNT and TOLC as predictors of social outcomes

Summary of hierarchical regression analyses with CNT, TOLC, and INS Interview as predictors of social outcomes (Step 2 only)

Path diagrams depicting the relationships among the Contingency Naming Test (CNT), Test of Language Competence (TOLC), and INS Interview as predictors of three social outcomes: (a) CBCL Social Competence; (b) CBCL Social Problems; and (c) VABS Socialization. Curved, double-arrow lines represent correlations. Single-arrow lines from variable to variable are labeled with standardized regression coefficients. Single-arrow lines to the right of the social outcome variables represent residual variances (i.e., 1 − total R2). Group membership, age, race, and SCI were treated as covariates in the path analyses. *p < .05.