Traumatic brain injury (TBI) is common during childhood, with mild TBIs (mTBIs) representing 80–90% of these injuries (Crowe, Babl, Anderson, & Catroppa, Reference Crowe, Babl, Anderson and Catroppa2009; Koepsell et al., Reference Koepsell, Rivara, Vavilala, Wang, Temkin, Jaffe and Durbin2011; McKinlay et al., Reference McKinlay, Grace, Horwood, Fergusson, Ridder and MacFarlane2008). The most common cause of mTBI in children below age 14 is falls (67%), followed by sport-related injuries, assaults, and motor vehicle accidents in adolescence and early adulthood (Crowe et al., Reference Crowe, Babl, Anderson and Catroppa2009; McKinlay et al., Reference McKinlay, Grace, Horwood, Fergusson, Ridder and MacFarlane2008). Epidemiological studies across Australia, New Zealand, and the United States reveal a bimodal distribution in mTBI incidence, with peaks around 0–5 years and 15–17 years of age (Barlow et al., Reference Barlow, Crawford, Stevenson, Sandhu, Belanger and Dewey2010; Koepsell et al., Reference Koepsell, Rivara, Vavilala, Wang, Temkin, Jaffe and Durbin2011; McKinlay et al., Reference McKinlay, Grace, Horwood, Fergusson, Ridder and MacFarlane2008; Russo, Rice, Chern, & Raftos, Reference Russo, Rice, Chern and Raftos2012). The larger US hospital-based study reported rates of 412 per 100,000 in children aged 0–4, and 316 per 100,000 in older adolescents (Koepsell et al., Reference Koepsell, Rivara, Vavilala, Wang, Temkin, Jaffe and Durbin2011). These figures may be an underestimation given that many mTBI cases are not treated in hospitals (McKinlay et al., Reference McKinlay, Grace, Horwood, Fergusson, Ridder and MacFarlane2008). Therefore, if only a small proportion of children experience negative outcomes following mTBI, this remains a serious public health problem.
There is substantial variation in outcomes for children following mTBI, even when injuries appear similar. Most studies have utilised cognitive assessment measures and/or behavioural rating scales to measure outcomes following mTBI. Fewer studies have focused on postconcussive symptoms (PCS) (Yeates, Reference Yeates2010). PCS refer to a set of symptoms that commonly occur following mTBI but are not unique to this population. Symptoms are typically categorised into somatic, cognitive, sleep, behavioural, and affective/mood subcategories. While PCS typically resolve over days to weeks following injury, a recent review suggested that 14–29% of children experience persistent or recurrent PCS for 3 months or longer after mTBI (Barlow, Reference Barlow2016). Only a few well-controlled longitudinal studies have examined PCS outcomes up to 12-month postinjury or beyond, and these have focused on children above the age of six or eight (Barlow et al., Reference Barlow, Crawford, Stevenson, Sandhu, Belanger and Dewey2010; McNally et al., Reference McNally, Bangert, Dietrich, Nuss, Rusin, Wright, Taylor and Yeates2013; Olsson et al., Reference Olsson, Lloyd, LeBrocque, McKinlay, Anderson and Kenardy2013; Yeates et al., Reference Yeates, Taylor, Rusin, Bangert, Dietrich, Nuss, Wright, Nagin and Jones2009). These studies have typically shown further decline in PCS rates from 3- to 12-months postinjury, with the larger of these studies reporting persistent or recurrent symptoms in 2.3% of children with mTBI compared with 0.01% of children with extracranial injury (Barlow et al., Reference Barlow, Crawford, Stevenson, Sandhu, Belanger and Dewey2010). There remains a paucity of research involving preschool and school-aged children, which examines the predictors of long-term outcomes (Kirkwood et al., Reference Kirkwood, Yeates, Taylor, Randolph, McCrea and Anderson2008; Zemek, Farion, Sampson, & McGahern, Reference Zemek, Farion, Sampson and McGahern2013).
Predictors of Persistent or Recurrent Symptoms
Both injury and noninjury-related factors have been shown to contribute to persistent or recurrent PCS following mTBI (Carroll, Cassidy, Peloso et al., Reference Carroll, Cassidy, Peloso, Borg, von Holst, Holm, Paniak and Pepin2004; McKinlay, Reference McKinlay2009; Satz et al., Reference Satz, Zaucha, McCleary, Light, Asarnow and Becker1997). Meta-analytic reviews have shown how both injury-related and pre-existing child, environmental, and family factors may differentially impact symptoms reporting across the acute and subacute postinjury period after mTBI (Satz et al., Reference Satz, Zaucha, McCleary, Light, Asarnow and Becker1997; Zemek et al., Reference Zemek, Farion, Sampson and McGahern2013). Injury severity factors such as Glasgow Coma Score (GCS), length of posttraumatic amnesia (PTA), or whether the child lost consciousness have shown some predictive association with acute symptoms, but this weakens over time, with the few completed studies showing poor predictive utility beyond 3-month postinjury (Bernard, Ponsford, McKinlay, McKenzie, & Krieser, Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2016; McNally et al., Reference McNally, Bangert, Dietrich, Nuss, Rusin, Wright, Taylor and Yeates2013; Olsson et al., Reference Olsson, Lloyd, LeBrocque, McKinlay, Anderson and Kenardy2013; Yeates et al., Reference Yeates, Taylor, Rusin, Bangert, Dietrich, Nuss, Wright, Nagin and Jones2009). Examination of these associations is challenging, however, given that the vast majority of children with mTBI score at ceiling on the GCS (15/15) do not lose consciousness and do not undergo PTA screening (Melo et al., Reference Melo, Lemos-Junior, Reis, Araujo, Menezes, Santos, Barreto, Menezes and Oliveira-Filho2010; Thomas, Reference Thomas, Apps and Walter2012). By 3-month postinjury, preexisting child and family factors reportedly become the stronger predictors of persistent or recurrent PCS (McNally et al., Reference McNally, Bangert, Dietrich, Nuss, Rusin, Wright, Taylor and Yeates2013; Yeates et al., Reference Yeates, Taylor, Rusin, Bangert, Dietrich, Nuss, Wright, Nagin and Jones2009).
Age at injury has received significant attention, and debate continues as to whether there are “critical” periods of development when children are more vulnerable to residual deficits following TBI (Anderson, Godfrey, Rosenfeld, & Catroppa, Reference Anderson, Godfrey, Rosenfeld and Catroppa2012; Anderson & Moore, Reference Anderson and Moore1995; Crowe, Catroppa, Babl, Rosenfeld, & Anderson, Reference Crowe, Catroppa, Babl, Rosenfeld and Anderson2012; Kolb, Reference Kolb1999; Risen, Reesman, Yenokyan, Slomine, & Suskauer, Reference Risen, Reesman, Yenokyan, Slomine and Suskauer2017; Zemek et al., Reference Zemek, Barrowman, Freedman, Gravel, Gagnon, McGahern, Aglipay, Sangha, Boutis, Beer, Craig, Burns, Farion, Mikrogianakis, Barlow, Dubrovsky, Meeuwisse, Gioia, Meehan, Beauchamp, Kamil, Grool, Hoshizaki, Anderson, Brooks, Yeates, Vassilyadi, Klassen, Keightley, Richer, DeMatteo and Osmond2016). A recent systematic review suggested that children older than 13 were at increased risk of PCS persisting beyond 1-month postinjury (Zemek et al., Reference Zemek, Barrowman, Freedman, Gravel, Gagnon, McGahern, Aglipay, Sangha, Boutis, Beer, Craig, Burns, Farion, Mikrogianakis, Barlow, Dubrovsky, Meeuwisse, Gioia, Meehan, Beauchamp, Kamil, Grool, Hoshizaki, Anderson, Brooks, Yeates, Vassilyadi, Klassen, Keightley, Richer, DeMatteo and Osmond2016). A few studies have also shown that school-aged children are more likely to report symptoms following mTBI than preschool children (Barlow et al., Reference Barlow, Crawford, Stevenson, Sandhu, Belanger and Dewey2010; McKinlay, Ligteringen, & Than, Reference McKinlay, Ligteringen and Than2014). However, the inherent difficulty in identifying symptoms in younger children and lack of validated scales for use in preschool children raise the likelihood that symptoms are underreported in these younger age groups (Bernard, Ponsford, McKinlay, McKenzie, & Krieser, Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2017; Gioia, Schneider, Vaughan, & Isquith, Reference Gioia, Schneider, Vaughan and Isquith2009). As such, predictive outcome studies in children below the age of six remain sparse, despite notable peaks of incidence in this age group. Therefore, there remains a gap in our understanding of how younger children recover from mTBI, as well as the injury, child, and family factors that contribute to persistent or recurrent PCS.
The association between other preinjury child factors, such as learning difficulties or behavioural disturbance, with persistence of PCS has been increasingly recognised (Yeates et al., Reference Yeates, Taylor, Rusin, Bangert, Dietrich, Nuss and Wright2012). Children with premorbid learning disorders exhibit greater impairment after mTBI across a range of measures (Anderson, Catroppa, Morse, Haritou, & Rosenfeld, Reference Anderson, Catroppa, Morse, Haritou and Rosenfeld2009; Ponsford et al., Reference Ponsford, Willmott, Rothwell, Cameron, Ayton, Nelms, Curran and Ng1999). Poor preinjury behavioural functioning has also been associated with poorer outcomes following TBI (Anderson, Morse, Catroppa, Haritou, & Rosenfeld, Reference Anderson, Morse, Catroppa, Haritou and Rosenfeld2004) and may lead to secondary or new onset attention-deficit hyperactivity disorder (ADHD) (Max et al., Reference Max, Schachar, Levin, Ewing-Cobbs, Chapman, Dennis, Saunders and Landis2005).
Finally, parental response to the injury and the environment in which the child recovers have also been shown to play a role in expression of PCS as reported by children and parents (Ganesalingam et al., Reference Ganesalingam, Yeates, Ginn, Taylor, Dietrich, Nuss and Wright2008; Wade et al., Reference Wade, Cassedy, Walz, Taylor, Stancin and Yeates2011; Yeates, Taylor, Walz, Stancin, & Wade, Reference Yeates, Taylor, Walz, Stancin and Wade2010). This relationship is likely bi-directional in that the child’s symptoms may elicit a behavioural response in their parents but equally a stressful home environment may also impede a child’s recovery (Anderson & Yeates, Reference Anderson and Yeates1997; Ganesalingam et al., Reference Ganesalingam, Yeates, Ginn, Taylor, Dietrich, Nuss and Wright2008; Taylor & Alden, Reference Taylor and Alden1997). Further work is required to delineate the contributions of these factors to symptoms over extended periods (Carroll, Cassidy, Holm, Kraus, & Coronado, Reference Carroll, Cassidy, Holm, Kraus and Coronado2004).
The Current Study
In a prior study of this cohort, we examined the predictors of PCS across the first 3-month postinjury (Bernard et al., Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2016). This study highlighted that having sustained an mTBI strongly predicted PCS symptoms in the first week postinjury but showed a weakened (yet still significant) association with PCS from 1- to 3-month postinjury. Non-injury factors such as older age and preexisting learning difficulties became the significant predictors of PCS 1- to 3-month postinjury. Family factors, including higher parental stress, higher socio-economic status (SES), and being of Anglo–Saxon descent, also consistently predicted greater PCS across the first 3-months postinjury.
The current study aimed to extend the 2016 study by following up this cohort at or beyond 8-month postinjury using the same prospective, longitudinal, case-controlled design, to investigate the relative contributions of injury and noninjury factors on persistent or recurrent symptoms. It was hypothesised that by 8 or more months postinjury the most significant predictors of persistent or recurrent PCS would be preexisting child and family factors including preinjury learning difficulties or behavioural disturbance, and higher parental stress. It was also hypothesised that children with mTBI would report more symptoms than trauma controls (TCs).
METHOD
Ethics approval was obtained through from Western Health and Monash University. The participants were 64 parents of children (31 mTBI and 33 TCs) who sustained injury between the ages 2 and 12, whose PCS across the first 3-month post-injury have been previously described by Bernard and colleagues (Bernard et al., Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2016, Reference Bernard, McKinlay, Krieser, Testa and Ponsford2017; Bernard, McKinlay et al., Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2017). The current study assessed PCS at 8 or more months postinjury and examined a range of injury and non-injury predictive factors.
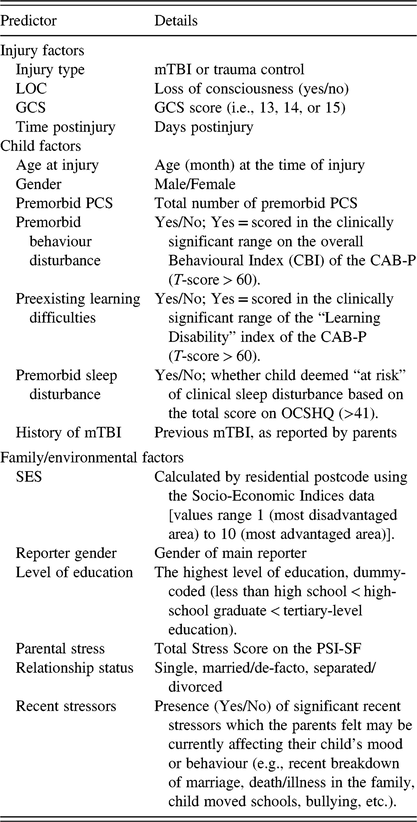
The details of the research design, recruitment procedures, inclusion/exclusion criteria, and study population have been previously described (Bernard et al., Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2016), but in brief the study adopted a prospective longitudinal design to examine symptom presentation across the postinjury period for children who sustained an mTBI or extracranial injury (TC group). Symptom ratings at follow-up were compared with pre-injury estimates (i.e. adjusted scores) as rated by parents at recruitment within 72 hr of injury. Demographic, preinjury measures (i.e., preinjury symptoms, child behaviour, child sleep, parental stress), educational and medical history and injury-related information were collected from parents and medical records at recruitment. The parents of children in the study were re-contacted via telephone 1 week, 1 month, 3 months, and at or beyond 8-month postinjury. The PCS symptom scale and measures of child behaviour, sleep, and parental stress were re-administered. An overview of study variables is provided in Table 1, and the summary of measures used outlined below.
Table 1. Outline of injury, child, and family predictor variables collected

mTBI, mild traumatic brain injury; LOC, loss of consciousness; GCS, Glasgow Coma Score; CAB-P, Clinical Assessment of Behaviour (parent report version); OCSHQ, Owen’s Children’s Sleep Habits Questionnaire; SES, socio-economic status; PSI-SF, Parental Stress Index – Short Form.
Measures
The SES score was calculated based on the participants’ residential postcode using the Socio-Economic Indexes for Areas developed by the Australian Bureau of Statistics, with 1 indicating most disadvantaged, and 10 the most advantaged area. At long-term follow-up (>8-month postinjury), some additional information was collected from parents since the last 3-month review. This included information about any concussions/head injuries (Yes/No), other neurological events (Yes/No), new medical diagnoses, newly diagnosed or identified learning difficulties, current relationship status of parents/carers (married or de-facto, single, divorced, widow), and whether the child had been exposed to any significant recent stressors (Yes/No) which parents felt may be currently affecting their child’s mood or behaviour (e.g., recent marriage breakdown, family death/illness, moving schools, bullying, etc.).
Injury characteristics
Injury severity was assessed using the GCS (Jennett, Reference Jennett1976) on presentation to emergency department (ED) and parental report of loss of consciousness (when witnessed). Unfortunately, assessment of PTA was not routinely conducted in the ED. Additional information collected from ED records included time of admission, wait time, length of stay, injury description, and diagnosis.
Child factors
Parental ratings of childrens’ premorbid behaviour were obtained at recruitment using the 70-item Clinical Assessment of Behaviour-Parent version (CAB-P), suitable for ages 2–18 (Bracken & Keith, Reference Bracken and Keith2004). The CAB-P was re-administered at 1, 3, and >8-months postinjury. The CAB produces a Behavioural Index (CBI) with two scales: internalising behaviour and externalising behaviour. Children were classified as having significant behavioural disturbance and learning difficulties if they scored in the clinically significant range of the Behavioural Index, and “Learning Disability” index of the CAB-P (T-score > 60), respectively.
The Owen’s Children’s Sleep Habits Questionnaire (CSHQ; Owens, Spirito, & McGuinn, Reference Owens, Spirito and McGuinn2000) assessed preinjury sleep habits at recruitment and was re-administered 1, 3, and >8-month postinjury. The CSHQ is a 36-item parental-report measure of sleep problems in school children, also validated in toddlers and preschool children (Goodlin-Jones, Sitnick, Tang, Liu, & Anders, Reference Goodlin-Jones, Sitnick, Tang, Liu and Anders2008). A clinical cut-off score of 41 suggested a child was at “a-risk” of clinical sleep disturbance.
Family factors
Levels of parental stress were measured using the Parenting Stress Index (PSI)-Short Form, a 36-item self-report questionnaire derived from the full-length PSI test (Abidin, Reference Abidin1983). A Total Stress Score reflects personal parental stress and stress derived from parent–child interactions and child’s behaviour. It was administered at recruitment (premorbid measure), 3-, and >8-months postinjury.
Postconcussion Symptom Scale
Symptoms in children were assessed using a 28-item symptom scale documenting the presence and severity [5-point severity scale ranging from “0” (not experienced at all) to “4” (a severe problem)] of each symptom. Given the lack of validated scales for this younger population, a comprehensive list of symptoms was generated from the most commonly used and available Postconcussion Symptom Scale (PCSS) where the parental report was available. Based on a review by Gioia (Gioia et al., Reference Gioia, Schneider, Vaughan and Isquith2009), the scales included the Rivermead Postconcussive Questionnaire (Gagnon, Swaine, Friedman, & Forget, Reference Gagnon, Swaine, Friedman and Forget2005), Postinjury Symptom checklist (Yeates et al., Reference Yeates, Taylor, Barry, Drotar, Wade and Stancin2001), and Acute Concussion Evaluation (Gioia, Collins, & Isquith, Reference Gioia, Collins and Isquith2008). The aim was to capture the widest range of symptoms possible. Therefore, the physical/somatic, cognitive, behavioural, affective, and sleep-related symptoms from the above scales were cross-checked, with equivalent items matched together (e.g., “was sensitive to noise” matched with “noise sensitivity”). This resulted in a 28-item PCSS with a 5-point severity scale ranging from 0 to 4. Severity scores were also dichotomised to indicate the presence or absence of symptoms as follows; scores of 0 (“not experienced at all”) and 1 (“no more of a problem”) as “Non-symptomatic” and scores of 2 (“mild problem”), 3 (“moderate problem”), and 4 (“severe problem”) as “Symptomatic.” Preliminary reliability analysis revealed good internal consistency across follow-up time points (Cronbach’s α mean across time points = .86 (SD = 0.02, range = 0.06), with no single items reducing the α value below .84, if deleted), providing justification for inclusion of all 28 items (Cronbach, Reference Cronbach1951).
The PCSS was completed via telephone interview with parents. Retrospective parent ratings of premorbid PCS were also collected during the first interview, and PCS scores presented reflect a change from this premorbid level (i.e., Time 1 = Time 1 rating – baseline rating). In response to difficulties highlighted by previous research groups around PCS assessment in younger children (Barlow et al., Reference Barlow, Crawford, Stevenson, Sandhu, Belanger and Dewey2010; Hooper et al., Reference Hooper, Alexander, Moore, Sasser, Laurent, King, Bartel and Callahan2004; McKinlay et al., Reference McKinlay, Ligteringen and Than2014), our study adopted a semi-structured interview style when administering the PCS checklist. Concrete behavioural exemplars were supplied for each symptom to assist parents with identification of symptoms in their children and avoid misinterpretation of terminology (Bernard, McKinlay, Krieser, Testa, & Ponsford, Reference Bernard, McKinlay, Krieser, Testa and Ponsford2017; Bernard, Ponsford et al., Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2017).
Data Analysis
Analysis was conducted using Stata Statistical Software Version 14 (StataCorp, 2013). Sample characteristics were described using means and standard deviations, unless otherwise stated. t-tests and ANOVAs were used to test for injury group differences on normally distributed data. Pearson Chi-Square (χ2) and Mann–Whitney U tests were used to conduct group comparisons for variables not normally distributed. Between-group comparisons of injury characteristics, medical and family factors, were conducted using Pearson χ2 cross-tabulations. Group differences in individual symptom frequency were examined, but to reduce the risk of type 1 error, comparisons were made at a subcategory level (i.e., somatic, sleep, cognitive, behavioural, and affective) using χ2 analysis, with Bonferroni adjustment of familywise α. Unless otherwise specified, statistical significance was set at 0.05, and bonferroni adjusted α levels were adopted when multiple comparisons were made. In the symptom subcategory analysis (Table 4), α values were adjusted to correct for familywise error rate (somatic α = .006, sleep α = .013, cognitive α = .007, behavioural α = .008, affective α = .017).
The main outcome variable (total PCS) was recoded as an ordinal categorical variable (whereby 0 = no PCS, 1 = 1–2 PCS, 2 = 3–5 PCS, and 3 = >6 PCS). To identify the key variables and reduce the number of variables relative to sample size, initial separate ordinal logistic regression analyses were run to examine the predictive utility of each of the 15 predictor variables (outlined in Table 1) on persistent or recurrent PCS (i.e., univariate analyses). As recommended by Hosmer and colleagues, a p value of 0.2 was applied to determine which variables would be included in the final model (Reference Hosmer, Lemeshow and Sturdivant2013). The use of the more liberal p value was to capture variables that may show weak associations by themselves, but exhibit stronger associations with the outcome variable when combined with other variables.
The final model included variables identified from the process described above and was analysed using random effects ordinal logistic regression with variables entered simultaneously. The advantages of using random effects regression modelling are that it (1) estimates both individual and injury group trend lines over multiple time points; (2) is less restrictive regarding missing data and uses data from all individuals and therefore does not rely on endpoint analysis, and (3) allows time-invariant variables (e.g., gender) to be absorbed by the intercept (Gibbons, Hedeker, Elkin, & et al., Reference Gibbons, Hedeker, Elkin, Waternaux, Kraemer, Greenhouse, Shea, Imber, Sotsky and Watkins1993). Based on these criteria, six variables were included in the final model, including reporter education, premorbid parental stress, premorbid behaviour, premorbid learning difficulties, number of acute PCS, and loss of consciousness. The percentage of PCS within each group was calculated using cross-tabs.
RESULTS
Multiple attempts were made to contact all 101 (55 TC and 46 mTBI) participants who were initially enrolled in the study and who participated in the 3-month follow-up (Bernard et al., Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2016). From this original cohort, long-term follow-up was successfully completed in 67% of mTBI (n = 31) and 60% of TC children (n = 33). Of the remaining 37 participants, 20 were uncontactable and 17 (7 mTBI and 10 TC) declined to participate due to time constraints (n = 5), considering that participation was not relevant as their child was symptom-free (n = 4), or they did not specify a reason (n = 8), opting out via text/e-mail. Importantly, all parents reporting symptoms in their child at the 3-month follow-up (n = 17) agreed to participate.
As outlined in Table 2, the demographic and injury characteristics of those followed up versus those not included were largely comparable. Of note, those successfully followed up had significantly higher SES (based on the residential postcode) and lower rates of premorbid learning difficulties. Importantly, children who were symptomatic at 3-months postinjury were equally spread across the two groups.
Table 2. Demographics, injury factors, and premorbid characteristics by follow-up status (i.e., children included in the follow-up vs. those who were not)

Note. All values represent the number of children (%) within included/exclude group unless otherwise specified.
mTBI, mild traumatic brain injury group; TC, trauma control group; SES, socio-economic status; HS, high-school graduate; LOC, loss of consciousness.
a All reported loss of consciousness was suspected to be less than 10 s.
b Presence of PCS at 3-month follow-up.
c Value represents a decile value determined by postcode (ranging 0–10). Lower decile value = lower SES.
* Significance at α below .05 level
** Significance at α below .01 level.
Participant demographics, children’s injury details and child/parent preinjury factors are outlined in Table 3. Injury groups followed up did not significantly differ with regards to demographic, child, educational and family factors, premorbid behavioural problems, premorbid sleep disturbance, time postinjury, or number of premorbid PCS. The exception to this was age, whereby the average age at injury was slightly younger in TCs. Roughly, two-thirds of children were male which is consistent with epidemiological studies of this population (Koepsell et al., Reference Koepsell, Rivara, Vavilala, Wang, Temkin, Jaffe and Durbin2011). The majority of injuries were due to falls (84% TC and 87% mTBI) with remaining injuries mostly sports-related. Based on the GCS scores, the mTBI group’s injuries were very mild, with 95% scoring the maximum 15 out of 15. Baseline assessment of behaviour and sleep habits revealed no statistically significant differences in scores between mTBI and TC children (Table 3).
Table 3. Demographics, injury factors, and premorbid characteristics of mTBI and TC groups

Note. All values represent the number of children (% within included/exclude group) unless otherwise specified.
mTBI, mild traumatic brain injury group; TC, trauma control group; SES, socio-economic status; HS, high-school graduate; LOC, loss of consciousness.
a All reported loss of consciousness was suspected to be less than 10 s.
b Learning difficulties defined by whether child met clinical significance on the “Learning Disability” index of the Clinical Assessment of Behaviour scale (T-score > 60).
c Behavioural disturbance as defined by whether child met clinical significance on the overall index of the Clinical Assessment of Behaviour (T-score > 60).
d Sleep disturbance as defined by whether child deemed “at risk” of clinical sleep disturbance based on the total score on Owen’s Children’s Sleep Habits Questionnaire (>41).
e Value represents a decile value determined by postcode (ranging 0–10). Lower decile value = lower SES.
f Stressors were coded according to the description provided in Table 1.
Follow-up occurred at an average of 23-months postinjury (Median = 23.50). Time postinjury ranged from 8 to 41 month (Mean = 24.29, Median = 25.00) for the mTBI group and 9 to 37 month (Mean = 23.18, Median = 23.00) for the TC group. One child in the mTBI group was suspected to have sustained another “concussion” 2 months earlier (i.e., his mother described some postinjury headaches and dizziness). His symptoms were reported to have resolved quickly, and he was not admitted to an ED. No parents reported their child having sustained any other significant neurological events. Five mTBI and two TC children had new medical or health diagnoses: three mTBI children had since been diagnosed with ADHD, one mTBI child was diagnosed with “mild autism”, one TC child had been diagnosed with “Anxiety” after suffering a panic attack 6 months before follow-up, one mTBI child had a new allergy (anaphylactic), and one mTBI child also had ongoing tinnitus since concussion (not accounted for in PCSS).
Characteristics of Persistent or Recurrent PCS
Parent-reported symptoms across the first 3-months postinjury previously described by Bernard, Ponsford et al. (Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2017) were updated to incorporate symptom prevalence beyond 8-month postinjury. As illustrated in Figure 1a, by 8 or more months postinjury, the number of symptoms in the mTBI group continued to reduce slightly from 3-months postinjury. By comparison, rates of symptoms in the TC group (Figure 1b) increased beyond 3-month postinjury. At long-term follow-up, rates of symptoms between the mTBI and TC groups did not differ significantly (U = 489.0, p = .70, r = .06), with roughly ~30% of parents reporting at least one persistent or recurrent symptom (29.1% in the mTBI group, 27.3% in the TC group). Characteristics of symptoms by group are outlined in Table 4. Group comparison of symptom subcategories revealed no significant differences between the mTBI and TC groups on either somatic/physical symptoms (χ 2 (1) = 0.24; p = .63), sleep symptoms (χ 2 (1) = 0.42; p = .52), cognitive symptoms (χ 2 (1) = 0.72; p = .40), behavioural/psychological symptoms (χ 2 (1) = 0.58; p = .45), or affective symptoms (χ 2 (1) = 1.24; p = .27). Collapsing across groups, the most persistent or recurrent symptoms were increased emotionality (11%), anxiety (11%), difficulty concentrating and completing tasks (9%), headaches (8%), and aggression (8%). At an individual symptom level, rates of parental reported “aggression” and “difficulty completing tasks” were higher in the mTBI group, while “problems coping with change” and “anxiety” were higher in the TC group (Table 4). In terms of single versus multiple reports of ongoing symptoms, the majority (75%) endorsed two or more symptoms. Twenty-five percent of parents endorsed a single symptom.
Table 4. Percentages of children who present with symptoms beyond 8-month postinjury, by injury group (mTBI, TC)

mTBI, mild traumatic brain injury; TC, trauma control.

Fig. 1. (a) Number of symptoms (adjusted from premorbid levels) across the postinjury follow-up period, as reported by parents of children who sustained an mTBI. (b) Number of symptoms (adjusted from premorbid levels) across the postinjury follow-up period, as reported by parents of children who sustained a mild injury to the body (TC group).
To gain further understanding of symptom patterns over time, characteristics of symptom reporting at 3 month were compared with those at longer-term follow-up at an individual level. Of the 14 parents of mTBI children whose parents endorsed symptoms 3-month postinjury, all participated in longer-term follow-up. Of this group, eight reported that the child’s symptoms had ceased entirely, two reported an increased number of symptoms (all within cognitive/psychological symptom categories), one reported persistance (or possibly resolution and recurrence) of one symptom (“more emotional”), and three reported a decrease in symptom numbers. In eight cases (five TC and three mTBI), parents who denied any symptoms at 3 months reported symptoms at longer-term follow-up, but in half of the cases this was only one symptom. In the TC group, most frequently reported symptoms were psychological (“difficulties coping with change” (n = 3) and “anxiety or worry” (n = 4)). In 8% of the sample who endorsed 1–2 physical/somatic symptoms (mostly “headaches”), the majority (6%) did not report any cognitive, sleep, behavioural, or affective symptoms. Similarly, for those reporting multiple symptoms, symptoms tended to cluster in the cognitive and behavioural domains as highlighted above.
Predictors of Persistent or Recurrent PCS (>8-Month Postinjury)
The results from the preliminary univariate ordinal logistic regression analyses suggested that six variables were associated with persistent or recurrent symptoms, which were included in the final model. These included: level of reporter education, parental stress (premorbid), pre-existing behaviour disturbance, preexisting learning difficulties, PCS (acute), and loss of consciousness. Excluded variables included: injury type, GCS, time postinjury, age at injury, gender, premorbid PCS, premorbid sleep disturbance, history of mTBI, SES, reporter gender, level of reporter education, relationship status, and recent stressors.
The results from the final multivariate model examining predictors of persistent or recurrent PCS at or beyond 8-month postinjury are outlined in Table 5. The only significant predictor of outcome was reporter level of education, with parents of both lower [<HS (high-school graduates)] and higher (>HS) levels of educational attainment both more likely to report persistent or recurrent PCS compared with those who completed high school with no further study. The presence of pre-existing learning difficulties approached significance as a predictor of symptom outcomes (p = 0.053).
Table 5. Results from the final model of the ordinal regression analysis examining the predictors of persistent symptoms

DISCUSSION
This was one of the few longer-term follow-up studies to prospectively examine the injury and noninjury-related predictors of “post-concussive-like” symptoms in children following mTBI, as compared with children who sustained mild extracranial injury. Follow-up occurred on average two years postinjury but ranged from eight to 41 months in the mTBI group and nine to 37 months for the TC group. In response to difficulties highlighted by previous research groups around PCS assessment in younger children (Barlow et al., Reference Barlow, Crawford, Stevenson, Sandhu, Belanger and Dewey2010; Hooper et al., Reference Hooper, Alexander, Moore, Sasser, Laurent, King, Bartel and Callahan2004; McKinlay et al., Reference McKinlay, Ligteringen and Than2014), our study adopted a structured interview approach to symptom assessment rather than having parents self-complete a checklist.
As hypothesised, by eight or more months postinjury, having sustained an mTBI no longer predicted persistent or recurrent symptoms and in fact parents of children in the TC group were equally likely to report “post-concussive like” symptoms at follow-up. The overall predictive utility of non-injury factors measured in this study was weak, with parent (reporter) education being the only significant predictor of persistent or recurrent symptoms. Specifically, both lower and higher levels of educational attainment (i.e. High-School Certificate) were associated with higher symptom reporting, compared with parents who obtained a high-school certificate. The presence of pre-existing learning difficulties, as defined by a clinically significant subscale score on the CAB (i.e. not a diagnosed learning disorder), approached significance as a predictor of symptoms, so possibly with a larger sample this result would have reached significance. Non-injury factors that had demonstrated predictive utility 3-month postinjury, such as older age, higher parental stress, higher SES, and reporters of Anglo–Saxon descent (Bernard et al., Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2016), were no longer significant predictors at or beyond eight months postinjury. In particular, it is important to acknowledge that the total number of symptoms did not differ as a function of age, as highlighted in previous research (Barlow et al., Reference Barlow, Crawford, Stevenson, Sandhu, Belanger and Dewey2010; Bernard et al., Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2016; McKinlay et al., Reference McKinlay, Ligteringen and Than2014). The remaining variables that were analysed in this study, including gender, premorbid PCS, premorbid behaviour or sleep disturbance, reporter (parent) gender or relationship status, recent stressors, or history of mTBI, were also not shown to predict persistent or recurrent PCS.
Taken together, these findings are broadly consistent with previous studies. Prior research has suggested that PCS outcomes are best accounted for by a combination of injury characteristics (e.g., severity of injury) and noninjury-related factors (Kirkwood et al., Reference Kirkwood, Yeates, Taylor, Randolph, McCrea and Anderson2008; Zemek et al., Reference Zemek, Farion, Sampson and McGahern2013) and that typically injury-related factors progressively weaken in their association with PCS over time. This was confirmed by the combined findings from the current study and the earlier study by our group (Bernard et al., Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2016). This relationship provides some support for the presence of neurophysiological changes underpinning the symptoms in the early postinjury stages (Giza & Hovda, Reference Giza and Hovda2014) but suggests that noninjury factors play a significant role in symptoms that present beyond this phase.
With regards to non-injury factors, previous studies have demonstrated that pre-existing child, demographic, and family/parental factors may contribute to persistent or recurrent PCS following mTBI to varying degrees. McNally et al. (Reference McNally, Bangert, Dietrich, Nuss, Rusin, Wright, Taylor and Yeates2013) found that higher rates of premorbid symptoms were the strongest predictor of child and parent symptoms ratings, while parental psychological adjustment was the strongest predictor of parent symptoms ratings. In a study examining PCS at six to 18 months post-injury, Olsson et al. (Reference Olsson, Lloyd, LeBrocque, McKinlay, Anderson and Kenardy2013) found that parental stress, anxiety, and children’s level of cognitive functioning were the strongest predictors of persistent or recurrent PCS. Similarly, the role of parental stress in symptom reporting has been documented in our earlier study, along with other demographic factors of the parents reporting the symptoms (Bernard et al., Reference Bernard, Ponsford, McKinlay, McKenzie and Krieser2016). In a large multicentre study, Zemek et al. (Reference Zemek, Farion, Sampson and McGahern2013) found that being of female sex, aged above 13, having a history of migraine, concussion (with symptoms > 1 week), sensitivity to noise, and fatigue, were all moderate predictors of persistent or recurrent PCS at 28-day postinjury. Ponsford et al. (Reference Ponsford, Willmott, Rothwell, Cameron, Ayton, Nelms, Curran and Ng2001) also found that preexisting learning difficulties were a significant predictor of PCS following mTBI.
The mechanisms whereby preexisting child and family factors contribute to the persistence of symptoms following mTBI remain unclear. The association of reporter education level with symptom reporting may reflect variations in awareness or understanding of mTBI. For instance, parents with higher education may have greater exposure to public information around PCS and therefore may misattribute or overinterpret symptoms in the context of a suspected mTBI. This bias would not apply to parents of children who sustained extracranial trauma and therefore not contribute to inflated reporting of symptoms in this population. Nonetheless findings from this study highlight the nonspecific nature of symptoms after trauma and suggest a range of biopsychosocial factors could contribute to the expression and/or detection of “post-concussive like” symptoms in the general population (Mittenberg, Wittner, & Miller, Reference Mittenberg, Wittner and Miller1997). Parents with lower education have also been shown to be at greater risk of response bias and, therefore, may be more likely to endorse symptoms when asked specifically (Meisenberg & Williams, Reference Meisenberg and Williams2008).
The association of preexisting learning difficulties with poorer mTBI outcomes has been reasonably well documented (Babikian, McArthur, & Asarnow, Reference Babikian, McArthur and Asarnow2013; Ponsford, Olver, Nelms, Curran, & Ponsford, Reference Ponsford, Olver, Nelms, Curran and Ponsford1999; Satz et al., Reference Satz, Zaucha, McCleary, Light, Asarnow and Becker1997; Zemek et al., Reference Zemek, Farion, Sampson and McGahern2013), but the mechanisms underpinning this relationship remain unclear. The “threshold theory” described by Satz (Reference Satz1993) proposes that once brain reserve is depleted beyond a critical threshold (i.e., from TBI), functional deficits may begin to emerge (Satz, Reference Satz1993). As such, even after mTBI, lower thresholds may render the onset and maintenance of symptoms more likely. This finding has been reasonably well supported across studies of older children (Babikian et al., Reference Babikian, McArthur and Asarnow2013; Biederman et al., Reference Biederman, Feinberg, Chan, Adeyemo, Woodworth, Panis, McGrath, Bhatnagar, Spencer, Uchida, Kenworthy, Grossman, Zafonte and Faraone2015; Fay et al., Reference Fay, Yeates, Taylor, Bangert, Dietrich, Nuss, Rusin and Wright2010) and adults following mTBI (Kraus et al., Reference Kraus, Schaffer, Ayers, Stenehjem, Shen and Afifi2005). An alternative view is that parents may endorse symptoms that relate to the child’s premorbid state to the injury itself.
In the current study, examination of symptom profiles at or beyond eight months postinjury suggested that total number of symptoms did not vary between the mTBI and TC groups. Interestingly, while symptoms reported decreased in the mTBI group overall, the parents of TC children reported an increase in symptoms from 3-month postinjury. Inspection of this pattern in individual participants revealed that some parents reported stability or a slight increase/decrease in the number of symptoms at 3 month and a small subset (5 TC, 3 mTBI) described a new onset of symptoms that were not present at 3 month. At an individual symptom level, the most persistent or recurrent symptoms were “increased emotionality”, “anxiety”, “difficulty concentrating and completing tasks”, “headaches”, and “aggression”. The study’s small sample size prevented comparisons at an individual symptom level, but qualitatively rates of parent reported “aggression”, “more emotional”, and “difficulty completing tasks” were higher in the mTBI group, while “problems coping with change” and “anxiety” were higher in the TC group (Table 4). Interestingly, parental endorsement of symptoms at long-term follow-up tended to cluster into two groups, as also described by Risen et al. (Reference Risen, Reesman, Yenokyan, Slomine and Suskauer2017). The majority of parents who endorsed one to two physical/somatic symptoms (mostly “headaches” with one case of “sensitivity to noise”) did not report any cognitive, sleep, behavioural, or affective symptoms. Similarly, those who reported multiple symptoms tended to cluster on the cognitive and behavioural domains. This is perhaps not surprising given the previously discussed association between non-injury psychosocial factors and recovery.
The finding that symptoms increased in the control group from 3 months to longer-term follow-up certainly deserves some discussion. First, it reinforces the notion that while these symptoms are common following mTBI, they are not exclusive to this population and may in part reflect a range of premorbid difficulties or effects of injury more generally (Hawley, Reference Hawley2003; Mittenberg et al., Reference Mittenberg, Wittner and Miller1997). Consistent with this are studies showing that symptoms reported are not specific to the TBI population. For example, research examining the presence of postconcussive-like symptoms in non-mTBI samples has revealed a variety of populations to endorse PCS, including general outpatients assessed for minor medical problems (Lees-Haley & Brown, Reference Lees-Haley and Brown1993) and psychological treatment (Fox, Lees-Haley, Earnest, & Dolezal-wood, Reference Fox, Lees-haley, Earnest and Dolezal-wood1995; Iverson, Reference Iverson2006), personal injury claimants (Dunn, Lees-Haley, Brown, Williams, & English, Reference Dunn, Lees-Haley, Brown, Williams and English1995), individuals with chronic pain (Gasquoine, Reference Gasquoine2000), and even the healthy population (Iverson & Lange, Reference Iverson and Lange2003). Given the finding from this study, it would appear important for researchers to consider the impact of recent/current stressors and/or significant life events at the time of assessment, and the potential impact of these on child and parent report of symptoms.
Clinical Implications
Experiencing prolonged symptoms following mTBI can be frustrating for children and challenging for parents. They can result in delayed return to school or sport, necessitate academic support, and/or increased reliance on health services (Gioia, Reference Gioia2016; Kirkwood, Peterson, Baker, & Connery, Reference Kirkwood, Peterson, Baker and Connery2017). Additionally, clinicians working in settings where these children present need to make informed decisions regarding the management of mTBI in children of varying ages (Yeates & Taylor, Reference Yeates and Taylor2005). To date, research has highlighted the complex interplay of child and family/environmental factors on persistent or recurrent “post-concussive-like” symptoms but has only been modestly successful in providing guidance with respect to which factors contribute most to outcomes. In a recent review, Zemek et al. (Reference Zemek, Barrowman, Freedman, Gravel, Gagnon, McGahern, Aglipay, Sangha, Boutis, Beer, Craig, Burns, Farion, Mikrogianakis, Barlow, Dubrovsky, Meeuwisse, Gioia, Meehan, Beauchamp, Kamil, Grool, Hoshizaki, Anderson, Brooks, Yeates, Vassilyadi, Klassen, Keightley, Richer, DeMatteo and Osmond2016) devised a clinical “risk score” for use in the ED to predict persistent or recurrent symptoms following mTBI. This showed some “modest discrimination” of persistent or recurrent PCS 1-month postinjury, but further validation studies are required. Unfortunately, the present study has identified that prediction of persistent or recurrent symptoms at long periods of time after injury is much more difficult. Equally, it has highlighted the importance of clinicians considering a broad range of potential contributory factors other than mTBI, particularly in children who present with symptoms at long periods after injury (Kirkwood et al., Reference Kirkwood, Yeates, Taylor, Randolph, McCrea and Anderson2008). The current study further highlights the need for researchers in this area to measure and control for a wide range of both pre-existing and concurrent child/family factors which may be perpetuating symptoms or leading to overreporting of symptoms by parents. The routine inclusion of well-matched injury control groups to control for risk factors and experience of a traumatic event (Carroll, Cassidy, Holm et al., Reference Carroll, Cassidy, Holm, Kraus and Coronado2004), and collection of preinjury measures of children’s learning difficulties, behaviours, and psychological state, and of parental and environmental stressors, appear essential in future studies.
Limitations
The current study has a number of limitations that warrant consideration. First, the timing of follow-up varied widely which made it challenging to discuss time frames with any specificity. The possibility of sampling bias must also be considered. For instance, all 17 parents who endorsed symptoms 3-month postinjury agreed to participate in longer-term follow-up, while a small subset of those who declined (n = 4) stated this was because their child was symptom-free. This may have inflated symptom reporting. Furthermore, the fact that SES was significantly higher in long-term follow-up participants potentially limits the generalisability of findings. The age differences between the groups may also have limited interpretation of the impact of age on outcomes. The sole reliance on parental report was another limitation. Ideally, PCS outcomes should be measured using a combination of child, parent, and teacher report where applicable (Gioia et al., Reference Gioia, Schneider, Vaughan and Isquith2009). Similarly, classification of “learning difficulties” based solely on the parental report of child behaviours on the CAB is not sufficient to make a diagnosis and should be interpreted with caution. It limits direct comparison with studies employing more formal learning disorder diagnoses (McKinlay, Dalrymple-Alford, Norwood, & Fergusson, Reference McKinlay, Dalrymple-Alford, Norwood and Fergusson2002). Unfortunately, including child and teacher report of symptoms and behaviour was beyond the scope and funding of the study.
Further to the above, it was unclear from the data collected whether symptoms being reported at the long-term follow-up were persistent (i.e., had persisted since the 3-month review) or recurrent (i.e., had dissipated and returned between reviews) as participants were not asked specifically. The number of predictors considered in the study was not exhaustive. There are additional variables shown to be associated with ongoing postconcussive-like symptoms. While interrater child/parent reliability has been shown to be moderate, it is variable and there is a tendency for parents to overreport externalising symptoms and miss internalised symptoms (Hajek et al., Reference Hajek, Yeates, Taylor, Bangert, Dietrich, Nuss, Rusin and Wright2011; McKinlay et al., Reference McKinlay, Ligteringen and Than2014). Finally, the study’s small sample size represented a limitation with regards to analysis and statistical power.
Future Directions
The ultimate goal of research in this area is to develop a comprehensive and integrated biopsychosocial model of outcomes that helps guide clinical management of symptoms (Yeates, Reference Yeates2010). The focus of this study was on predictors of outcome based on the information known at the time of injury, given that this is of clinical usefulness. However, to better understand the aetiology of persistent or recurrent symptoms beyond the acute postinjury phase, examination of concurrent factors impacting symptom reporting would also be useful. When undertaking longer-term follow-up studies, it would also be helpful for researchers to distinguish between persistent and recurrent symptoms. The relative contribution of injury and non-injury factors as predictors of PCS may also vary as a function of symptom type (Yeates & Taylor, Reference Yeates and Taylor2005). While this study lacked the sample size to investigate this theory further, larger studies could focus on subcategories or clusters of symptoms rather than total number of symptoms. Whilst this study did not find any significant association of age at injury with symptom numbers, larger studies may be able to better examine individual symptoms profiles in children of varying ages. Consideration that younger children may experience symptoms outside of what is typically on a PCSS is also important (Suskauer, Rane, Reesman, & Slomine, Reference Suskauer, Rane, Reesman and Slomine2018). Future studies could also collect multi-informant report of symptoms from parents, teachers, and children (Gioia et al., Reference Gioia, Schneider, Vaughan and Isquith2009).
ACKNOWLEDGEMENTS
The authors would like to acknowledge the time contribution of participants and their parents who were involved in this study. This research work was partially supported by a grant awarded to Professor Jennie Ponsford and Dr Audrey McKinlay from the Jack Brockoff foundation, and from Dr Coco Bernard’s Doctoral Research fund.
CONFLICT OF INTEREST
The authors have nothing to disclose.