Introduction
Posttraumatic stress disorder (PTSD) affects approximately 8% of the general U.S. population and between 10 and 25% of U.S. Veterans (Kessler, Sonnega, Bromet, Hughes, & Nelson, Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995). PTSD is characterized by specific clusters of symptoms, including dysfunction in re-experiencing (e.g., intrusive recollections), avoidance (e.g., avoidance of trauma reminders), dysphoria (e.g., anhedonia), and arousal (e.g., hypervigilance) (American Psychiatric Association, 2013). PTSD symptoms are also associated with reductions in quality of life and poor functional outcomes (Alonso et al., 2004). Cognitive symptoms are also embedded within the diagnostic criteria for PTSD. Specifically, individuals with PTSD report problems in concentration and everyday memory (Roca & Freeman, Reference Roca and Freeman2001), and a large literature associates PTSD with neurocognitive dysfunction in episodic memory, processing speed, attention, and executive functions (Brewin, Kleiner, Vasterling, & Field, Reference Brewin, Kleiner, Vasterling and Field2007; Scott et al., Reference Scott, Matt, Wrocklage, Crnich, Jordan, Southwick and Schweinsburg2015; Vasterling & Brailey, Reference Vasterling and Brailey2005). Cognitive deficits have been hypothesized to reflect dysfunction in prefrontal-limbic circuitry and linked to arousal symptoms (Daniels et al., Reference Daniels, McFarlane, Bluhm, Moores, Clark, Shaw and Lanius2010; Vasterling, Brailey, Constans, & Sutker, Reference Vasterling, Brailey, Constans and Sutker1998). However, controversy remains regarding the magnitude of neuropsychological deficits, their etiology, and their functional relevance (Crowell, Kieffer, Siders, & Vanderploeg, Reference Crowell, Kieffer, Siders and Vanderploeg2002; Danckwerts & Leathem, Reference Danckwerts and Leathem2003; Olff, Polak, Witteveen, & Denys, Reference Olff, Polak, Witteveen and Denys2014; Wisdom et al., Reference Wisdom, Pastorek, Miller, Booth, Romesser, Linck and Sim2014).
Notable methodological limitations in the literature have contributed to this controversy. First, many prior studies did not account for commonly occurring psychiatric comorbidities. Veterans and civilians with PTSD display high rates of alcohol and drug use disorders (Kessler et al., Reference Kessler, Sonnega, Bromet, Hughes and Nelson1995; Scherrer et al., Reference Scherrer, Xian, Lyons, Goldberg, Eisen, True and Koenen2008), and chronic use of alcohol and other substance such as cocaine, amphetamines, and benzodiazepines can have detrimental effects on neurocognitive functioning (e.g., Barker, Greenwood, Jackson, & Crowe, Reference Barker, Greenwood, Jackson and Crowe2005; Grant & Rourke, Reference Grant and Rourke2009; Jovanovski, Erb, & Zakzanis, Reference Jovanovski, Erb and Zakzanis2005; Scott et al., Reference Scott, Woods, Matt, Meyer, Heaton, Atkinson and Grant2007). Although there are some exceptions (e.g., Samuelson et al., Reference Samuelson, Neylan, Metzler, Lenoci, Rothlind, Henn-Haase and Marmar2006; Vasterling et al., Reference Vasterling, Duke, Brailey, Constans, Allain and Sutker2002), several studies have failed to either adequately characterize substance use disorders or appropriately use them in analyses (Horner & Hamner, Reference Horner and Hamner2002). Moreover, despite documented comorbidity between attention deficit/hyperactivity disorder (ADHD) and PTSD (Harrington et al., Reference Harrington, Miller, Wolf, Reardon, Ryabchenko and Ofrat2012), only eight of 60 studies in our previous meta-analysis of neurocognitive functioning in PTSD accounted for the presence of ADHD (Scott et al., Reference Scott, Matt, Wrocklage, Crnich, Jordan, Southwick and Schweinsburg2015), which raises the question of whether ADHD may partially account for neurocognitive findings in PTSD. Similarly, it has been suggested that neurocognitive outcomes in PTSD may simply reflect its established comorbidity with depression (e.g., Burriss, Ayers, Ginsberg, & Powell, Reference Burriss, Ayers, Ginsberg and Powell2008; Olff et al., Reference Olff, Polak, Witteveen and Denys2014).
Second, the literature is hampered by additional confounds that could affect neurocognitive functioning but are commonly discrepant between PTSD and comparison groups. Accounting for the effects of traumatic brain injury (TBI) may be particularly important in combat veterans, who have a relatively high prevalence of head injuries (Vasterling & Brailey, Reference Vasterling and Brailey2005). Most of these individuals have a mild traumatic brain injury (mTBI), which typically has minimal or subtle cognitive effects 9–12 months post-injury except in cases deemed to have “complicated” mTBI and, possibly, among individuals who have suffered multiple concussions (Boyle et al., Reference Boyle, Cancelliere, Hartvigsen, Carroll, Holm and Cassidy2014; Rohling, Larrabee, & Millis, Reference Rohling, Larrabee and Millis2012; Vasterling et al., Reference Vasterling, Brailey, Proctor, Kane, Heeren and Franz2012; c.f. Bigler et al., Reference Bigler, Farrer, Pertab, James, Petrie and Hedges2013). Nonetheless, veterans with PTSD have an increased risk of TBI (McAllister & Stein, Reference McAllister and Stein2010), and thus cognitive deficits observed in PTSD samples may be partially attributable to TBI. In addition, prior research has indicated that greater intellectual resources may protect against the development of PTSD (Breslau, Lucia, & Alvarado, Reference Breslau, Lucia and Alvarado2006; McNally & Shin, Reference McNally and Shin1995), and some authors have suggested that lower IQ may be responsible for cognitive deficits in individuals with PTSD (Bustamante, Mellman, David, & Fins, Reference Bustamante, Mellman, David and Fins2001; Gilbertson et al., Reference Gilbertson, Paulus, Williston, Gurvits, Lasko, Pitman and Orr2006). Thus, appropriate consideration of differences in intellectual resources is critical.
Third, numerous studies have pointed to the importance of conducting performance validity assessments in neuropsychological evaluations with psychiatric populations, especially those with potential secondary gain from poor results (Heilbronner et al., Reference Heilbronner, Sweet, Morgan, Larrabee and Millis2009; Schroeder & Marshall, Reference Schroeder and Marshall2011; c.f. Barrash et al., Reference Barrash, Denburg, Moser, Woolson, Schumacher and Doebbeling2007). Performance validity tests (PVTs) attempt to ensure that individuals engaging in neuropsychological assessment are exerting adequate test-taking effort. Although the interpretation of PVTs can be complex, ensuring that research participants perform above established cutoffs increases confidence that results are not due to inadequate test-taking effort.
Few studies have examined cognitive functioning after administering PVTs in PTSD (Horner, Mintzer, Turner, Edmiston, & Brawman-Mintzer, Reference Horner, Mintzer, Turner, Edmiston and Brawman-Mintzer2013; Marx, Doron-Lamarca, Proctor, & Vasterling, Reference Marx, Doron-Lamarca, Proctor and Vasterling2009). In a sample of individuals referred for worker’s compensation claims, Demakis, Gervais, and Rohling (Reference Demakis, Gervais and Rohling2008) showed that, after controlling for performance validity, PTSD symptoms were not significantly correlated with neuropsychological performance. However, only 22% of their sample had a diagnosis of PTSD, and all individuals were drawn from a medico-legal context, limiting the generalizability of findings. Wisdom and colleagues (2014) found minimal neuropsychological deficits in a PTSD sample after excluding individuals who performed below cutoffs on formal PVTs. However, these authors used a cutoff on a self-report questionnaire (PTSD Checklist) to indicate PTSD caseness, such that individuals with moderate levels of PTSD symptom reporting could be included in the healthy comparison group, which might not provide adequate diagnostic accuracy. Thus, no study to date examining neuropsychological functioning in PTSD has used a diagnostic interview with a priori criteria for PTSD while also administering PVTs.
Lastly, few studies have investigated the functional relevance of observed neuropsychological deficits. Wild and Gur (Reference Wild and Gur2008) showed that worse verbal memory was associated with poorer treatment outcomes in individuals undergoing cognitive behavioral therapy for PTSD, suggesting that verbal memory difficulties may limit recovery in individuals engaged in treatments reliant on verbal processes. Geuze, Vermetten, deKloet, Hijman, and Westenberg (Reference Geuze, Vermetten, de Kloet, Hijman and Westenberg2009) showed that episodic memory performance uniquely contributed to ratings of social and occupational functioning, such as time spent in productive activities or with family and friends. To our knowledge, however, no studies have examined the functional relevance of attention, executive functioning, or processing speed performances in PTSD. In other psychiatric and neurological disorders, executive functioning and processing speed deficits have been associated with functional difficulties, including driving (e.g., Marcotte et al., Reference Marcotte, Rosenthal, Roberts, Lampinen, Scott, Allen and Corey-Bloom2008), medication management (e.g., Hinkin et al., Reference Hinkin, Hardy, Mason, Castellon, Durvasula, Lam and Stefaniak2004), and occupational functioning (e.g., McGurk & Mueser, Reference McGurk and Mueser2006).
In sum, despite substantial research into neurocognitive functioning in PTSD, questions remain regarding the factors that account for observed findings and the functional relevance of neurocognitive deficits. Here, we aimed to examine the influence of potentially critical factors in accounting for reduced neurocognitive performance in individuals with PTSD. This study is the first to examine these factors while also using a “gold standard” diagnostic interview for PTSD, administering multiple performance validity assessments, and examining associated functional outcomes. Consistent with frontal/subcortical dysfunction and the results of our meta-analysis, we hypothesized that, after controlling for performance validity, veterans with PTSD would show moderate performance differences in episodic memory, attention/working memory, information processing speed, and executive functions compared to a group of veterans with combat exposure but no PTSD. We also hypothesized that deficits in episodic memory, processing speed, and executive functions would be associated with PTSD-associated arousal symptoms, worse occupational performance, and lower quality of life.
Methods
Participants
Forty-four veteran participants diagnosed with current PTSD via the Clinician Administered PTSD Scale (CAPS; see below) and 40 demographically matched combat-exposed veterans were assessed between August 2009 and December 2014. Participants were recruited from the VA Connecticut Healthcare System through referrals from other National Center for PTSD studies; via advertisements placed in clinics and public spaces within the hospital; and through outreach in veteran communities. The study received Institutional Review Board approval from both VA Connecticut and Yale University. No participants were inpatients at the time of enrollment, and 52.5% of individuals with PTSD reported taking psychotropic medications. See Table 1 for demographic and psychosocial information for this sample.
Table 1 Demographic, military, and mental health characteristics of the samples
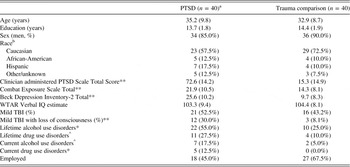
a Characteristics listed are from the final sample after excluding participants who exhibited insufficient effort.
b Chi-square test compares Caucasian to all other groups.
PTSD=posttraumatic stress disorder; TBI=traumatic brain injury; WTAR=Wechsler Test of Adult Reading
^p<.10; *p<.05; **p<.01
Written informed consent was obtained after participants were provided with a full description of the study. A trained and certified clinical psychologist or master’s level clinician administered the CAPS (Blake et al., Reference Blake, Weathers, Nagy, Kaloupek, Gusman, Charney and Keane1995) to assess PTSD symptoms. CAPS training included review of online training materials, observation of at least four CAPS sessions conducted by experienced clinicians, and rating of audio recordings for establishing inter-rater reliability. Kappa coefficients were between .80 and .90 for all interviewers. Participants were classified into current PTSD and trauma comparison (TC; without PTSD according to DSM-IV criteria). TC participants did not meet criteria for a lifetime diagnosis of PTSD or for current partial PTSD (Pietrzak, Goldstein, Southwick, & Grant, Reference Pietrzak, Goldstein, Southwick and Grant2012).
Based upon a structured clinical interview, participants with a history of moderate or severe TBI (i.e., loss of consciousness for greater than 30 min, post-traumatic amnesia for greater than 24 hr) or neurological disorders (e.g., epilepsy) were excluded. Information regarding history of childhood learning disorders, repeated grades in school, and diagnoses of ADHD were elicited as part of the clinical history. Participants who received a diagnosis of ADHD or learning disorder by a physician or psychologist before age 18 were excluded. The Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, Reference First, Spitzer, Gibbon and Williams2002) was administered to assess Axis I psychiatric diagnoses. Participants meeting lifetime criteria for a psychotic disorder or bipolar disorder and participants using benzodiazepines were excluded due to their significant cognitive effects (Barker, Greenwood, Jackson, & Crowe, Reference Barker, Greenwood, Jackson and Crowe2004). Participants in the PTSD group with substance use disorders were not excluded to recruit a representative sample of veterans with PTSD. Participants in the TC group were excluded if they had current or lifetime substance dependence.
Measures
Behavioral and Functional Assessments
The Combat Exposure Scale (Keane et al., Reference Keane, Fairbank, Caddell, Zimering, Taylor and Mora1989) afforded a measure of combat severity. The Beck Depression Inventory-2 (BDI-2; Beck, Steer, & Brown, Reference Beck, Steer and Brown1996) was used as a measure of depressive symptomatology. Military-related concussions were evaluated by postdoctoral fellows or neuropsychologists with a modified version of the Military Acute Concussion Evaluation (French, McCrea, & Baggett, Reference French, McCrea and Baggett2008), a structured interview that queries blast exposures, number of head injuries with loss or alteration of consciousness, details of head injuries, and post-concussive symptoms. A neuropsychologist independently assessed TBI severity using American Congress of Rehabilitation Medicine (1993) criteria. Criteria for mild TBI included: (1) alteration of consciousness or loss of consciousness not greater than 30 min; and/or (2) a period of posttraumatic amnesia that lasted at most 24 hr.
Neuropsychological Assessment
Participants were administered a comprehensive, standardized neuropsychological assessment designed to be sensitive to the potential neurocognitive effects of PTSD. Neuropsychology postdoctoral fellows or bachelor’s-level clinicians with extensive training by neuropsychologists administered the neuropsychological battery (see Table 2 for details on individual tests). Participants were also administered both standalone and embedded measures of performance validity. Standalone PVTs included the Test of Memory Malingering (TOMM; Tombaugh & Tombaugh, Reference Tombaugh and Tombaugh1996) and an 18-item version of the Digit Memory Test (DMT; Hiscock & Hiscock, Reference Hiscock and Hiscock1989; Woods et al., Reference Woods, Conover, Weinborn, Rippeth, Brill and Heaton2003), while the CVLT Forced Choice (Delis, Kramer, Kaplan, & Ober, Reference Delis, Kramer, Kaplan and Ober2000) served as an embedded PVT. Participants were classified as demonstrating inadequate effort if they performed below established cutoffs on any PVT. Cutoff scores for adequate performance were ≥45 of TOMM Trial 1 or Trial 2 (Denning, Reference Denning2012; O’Bryant et al., Reference O’Bryant, Gavett, McCaffrey, O’Jile, Huerkamp, Smitherman and Humphreys2008), ≥90% correct on the DMT (Berry, Allen, & Schmitt, Reference Berry, Allen and Schmitt1991; Woods et al., Reference Woods, Conover, Weinborn, Rippeth, Brill and Heaton2003), and ≥14 on CVLT Forced Choice (Delis et al., Reference Delis, Kramer, Kaplan and Ober2000). Before the assessment, participants underwent urine toxicology exams sensitive to illicit (e.g., cocaine) and licit (e.g., benzodiazepines) substances to ensure acute substance effects did not impact performances.
Table 2 Neuropsychological domains and tests examined

COWAT=Controlled Oral Word Association Test; CVLT-2=California Verbal Learning Test, 2nd Edition; DKEFS=Delis Kaplan Executive Functions Scale; Rey-O=Rey Osterreith; WAIS-IV=Wechsler Adult Intelligence Scale, 4th Edition.
Functional Outcomes
We used the World Health Organization’s Health and Work Performance Questionnaire (HPQ; Kessler et al., Reference Kessler, Ames, Hymel, Loeppke, McKenas, Richling and Ustun2004) to examine occupational functioning. The HPQ measures performance at work (presenteeism) and hours missed from work (absenteeism). Reports of HPQ presenteeism and absenteeism have performed well when validated against supervisors’ evaluations and other job performance metrics (Kessler et al., Reference Kessler, Ames, Hymel, Loeppke, McKenas, Richling and Ustun2004). Ratios created from the measure compare individuals’ missed hours to the number of hours their employer expected them to work (relative absenteeism) and performance relative to workers with a similar job type (relative presenteeism). Relative absenteeism is expressed as a percentage of expected hours over the prior 4 weeks and ranges between a negative number (works more than expected) and 1.0 (always absent), with higher scores representing worse occupational functioning. The measure of relative presenteeism asks participants to rate their performance over the past 4 weeks and the performance of an individual in a job similar to theirs on an 11-point scale that ranges from 0 (worst) to 10 (best). Relative performance ratio is calculated by dividing the participant’s rating by the score of most workers.
Ratings of health-related quality of life (HRQoL) were collected using the Veteran’s RAND 12-item Health Survey (VR-12; Kazis et al., Reference Kazis, Selim, Rogers, Ren, Lee and Miller2008), a brief adaptation of the Short Form-36, which assesses both physical and mental health functioning. These are widely used measures of functional status in studies of veterans, and many studies support their reliability and validity (Jones et al., Reference Jones, Kazis, Lee, Rogers, Skinner, Cassar and Hendricks2001). In accordance with standardized procedures, scores were converted into physical component summary (PCS) and mental component summary (MCS) scores using updated normative data (Selim et al., Reference Selim, Rogers, Fleishman, Qian, Fincke, Rothendler and Kazis2009).
Analyses
Neuropsychological measures in which higher scores reflected worse performance were multiplied by -1 so that lower scores reflected worse performance across the whole battery. All dependent measures were normally distributed (Kolmogorov-Smirnov p>.05) except for the DKEFS Color-Word Interference Condition and Trailmaking Number-Letter Switching, which were transformed using an inverse transformation, resulting in normally distributed variables.
Chi-square tests and independent samples t tests were used to compare groups on demographic and clinical characteristics. To reduce the possibility of Type I error and account for likely inter-correlation between dependent variables, group differences were analyzed with multivariate analysis of variance (MANOVA), with raw scores from neurocognitive tests chosen on a priori and classified into the neuropsychological domains shown in Tables 2 and 3. Tests of multivariate normality and sphericity showed no violations of assumptions. The RCFT-Copy was analyzed with ANOVA because it was the only visuoconstructional test available. For correlations among neurocognitive functioning, PTSD symptoms, and functional outcomes, Z scores were created from raw scores of measures, which were averaged to generate putative composite measures of neurocognitive functioning within that domain.
Table 3 Neuropsychological performance in the PTSD and Trauma Comparison groups

Note. Data are presented as M (SD) unless otherwise noted.
COWAT=Controlled Oral Word Association Test; CVLT-2=California Verbal Learning Test, 2nd Edition; DKEFS=Delis Kaplan Executive Functions Scale; Rey-O=Rey Osterreith; WAIS-IV=Wechsler Adult Intelligence Scale, 4th Edition.
In an effort to reduce Type I error, correlational analyses were only conducted on those variables that, consistent with our a priori hypotheses, differentiated PTSD and TC groups. Hierarchical regression analyses were conducted to examine the unique contribution of neurocognitive performance to functional outcomes in the PTSD group. In each regression, PTSD symptoms were entered in the first step, and neurocognitive Z scores were entered in the second step. The critical alpha level was set at .05.
As shown in Table 1, groups were comparable on age, education, race/ethnicity, gender, and an estimate of premorbid verbal IQ, the Wechsler Test of Adult Reading (WTAR; Wechsler, Reference Wechsler2001). Although only 18 individuals in the PTSD group and 27 individuals in the TC group were employed, employment numbers may have been reduced because 10 PTSD participants and 6 TC participants were enrolled in school on a full-time basis. The PTSD and TC groups differed in depression symptoms, mTBI with loss of consciousness (LOC), lifetime alcohol use disorders, and current alcohol and drug use disorders. Thus, lifetime alcohol use disorder, current alcohol/substance use disorder (combined), depression symptoms, and mTBI were included in follow-up MANCOVAs to examine their influence on significant results.
Results
Neuropsychological Performance
Four veterans with PTSD were classified as exhibiting insufficient test-taking effort, while all TC individuals were classified as putting forth adequate effort. Individuals who exhibited insufficient effort were excluded from further analyses, leaving 40 individuals with PTSD for analysis.
Table 3 shows results of MANOVAs after excluding participants with insufficient effort, which revealed significant group differences in speed of information processing (F[3,76]=3.01; p=.04) and executive functions (F[3,76]=3.6; p=.02), but no group differences in attention/working memory, verbal/language functioning, visuoconstruction, or episodic memory (ps > .10). Follow-up analyses revealed that Veterans with PTSD exhibited reduced performance on the WAIS-IV Coding (p=.04), Symbol Search (p=.02), and DKEFS Trailmaking Number Sequencing (p=.006) subtests; and D-KEFS Color-Word Interference Inhibition Trial (p=.002).
Effects of Comorbidities on Neuropsychological Performance
In follow-up MANCOVAs, depression symptoms were not associated with processing speed (F[3,75]=1.27; p=.29) or executive functioning (F[3,75]=0.25; p=.86), and PTSD remained significant in these models (F[3,75]=3.32; p=.02 and F[3,75]=2.90; p=.04, respectively). mTBI with LOC was not a significant predictor of cognitive performance in processing speed (F[3,75]=0.72; p=.54) or executive functioning (F[3,75]=1.00; p=.40), and PTSD remained significant in these models (p=.02 and p=.04, respectively). Although current substance/alcohol use disorders were significantly associated with executive functioning (F[3,75]=3.12; p=.03), PTSD remained significant after including this variable (F[3,75]=4.52; p=.006). Neither current (F[3,75]=1.12; p=.35) nor lifetime (F[3,75]=1.54; p=.21) alcohol/substance use disorders were associated with processing speed; PTSD also remained significant (F[3,75]=3.45; p=.02 and F[3,75]=3.24; p=.03, respectively). We also conducted supplementary analyses after excluding the seven PTSD individuals with current alcohol/substance use disorders. Results remained significant for processing speed (F[3,76]=3.1; p=.03) and executive functioning (F[3,76]=4.1; p=.01) even after exclusions.
Associations with PTSD Symptomatology and Everyday Functioning
Next, we examined whether executive functioning and processing speed Z scores were associated with PTSD symptom severity and with specific PTSD symptom clusters using a well-validated four-factor emotional numbing symptom model separating PTSD symptoms into re-experiencing, avoidance, numbing, and hyperarousal symptoms (Asmundson, Stapleton, & Taylor, Reference Asmundson, Stapleton and Taylor2004). As shown in Table 4, in the whole sample, executive functioning was negatively associated with CAPS Total Score, and specific clusters of numbing and hyperarousal symptoms, while information processing speed was only associated with hyperarousal symptoms of PTSD. However, in the PTSD group alone, no symptom clusters were significantly associated with executive functioning or processing speed.
Table 4 Correlations between PTSD symptom clusters and neurocognitive performance

*p<.05.
CAPS=Clinician Administered PTSD Scale; PTSD=posttraumatic stress disorder.
Table 5 shows correlations between PTSD symptom severity, neurocognitive performance, and functional outcomes within the PTSD group. We found a significant correlation between executive functioning and HPQ relative absenteeism, such that worse performance was associated with greater work absenteeism. CAPS Total Score was significantly associated with lower presenteeism on the HPQ, although neurocognitive performance was not associated with HPQ presenteeism. Analyses of the VR-12 revealed that both executive functioning and processing speed were significantly associated with the VR-12 PCS, such that better performance was associated with reports of higher HRQoL, although CAPS Total was not significantly associated with the VR-12 PCS. In contrast, CAPS Total was significantly associated with the VR-12 MCS, but neither neurocognitive domain was associated with MCS.
Table 5 Correlations between PTSD symptoms, neurocognitive performance, and functional measures within the PTSD group.

*p<.05.
**p<.01.
CAPS=Clinician Administered PTSD Scale; HPQ=World Health Organization Health and Work Performance Questionnaire; HRQoL=Health Related Quality of Life.
In the first step of a hierarchical regression analysis examining the relationship between executive functioning Z scores and HPQ relative absenteeism in the PTSD group, CAPS Total Score was not significant in the model, and the model accounted for little variance (R2=0.02; p=.60). When the executive functioning Z score was entered in the second step of the regression, it was a significant explanatory variable in the model (p=.03) and accounted for significant variance (R2 change=0.29; p=.03), although the overall R2 (0.30) was only marginally significant (p=.07). Similarly, for the VR-12 PCS, CAPS Total Score was not significant in the model, and the model accounted for little variance (R2=0.01; p=.66). When processing speed and executive functioning Z scores were entered in the second step of the regression, neither variable was significant in the model (p=.60 and p=.13, respectively), although addition of these variables accounted for significant variance in the step (R2=.21; p=.04) and in the model (R2 change=.21; p=.02).
Discussion
Consistent with hypotheses and our recent meta-analysis (Scott et al., Reference Scott, Matt, Wrocklage, Crnich, Jordan, Southwick and Schweinsburg2015), we found neurocognitive effects of a medium magnitude in speed of information processing and executive functions in veterans with PTSD compared to a demographically and IQ-matched, trauma-exposed comparison group. Our results are generally consistent with current fronto-limbic models of brain dysfunction in PTSD, which highlight altered arousal and dysfunctional communication between prefrontal and limbic/subcortical brain regions. The largest effect size and measure with the most robust association with PTSD symptoms was a version of the classic Stroop test, the DKEFS Color-Word Interference Test. This finding converges with accumulating evidence that PTSD is associated with difficulty inhibiting inappropriate or automatic responses (Casada & Roache, Reference Casada and Roache2005; Shucard, McCabe, & Szymanski, Reference Shucard, McCabe and Szymanski2008; Vasterling et al., Reference Vasterling, Brailey, Constans and Sutker1998). Together, these results bolster a model of generalized inhibitory control dysfunction in PTSD, which could help explain difficulties in regulation of both neuropsychological and emotional processes that have been noted in the disorder (Aupperle, Melrose, Stein, & Paulus, Reference Aupperle, Melrose, Stein and Paulus2012; Vasterling et al., Reference Vasterling, Brailey, Constans and Sutker1998).
In contrast to our hypotheses and much of the prior literature (e.g., Bremner et al., Reference Bremner, Randall, Scott, Capelli, Delaney, McCarthy and Charney1995; Brewin et al., Reference Brewin, Kleiner, Vasterling and Field2007; Jelinek et al., Reference Jelinek, Jacobsen, Kellner, Larbig, Biesold, Barre and Moritz2006; Vasterling et al., Reference Vasterling, Duke, Brailey, Constans, Allain and Sutker2002), we found no significant differences on measures of episodic memory or attention in our sample of veterans. There are several potential reasons for these discrepancies. First, our study excluded conditions that could significantly affect attention and memory, including ADHD, learning disorders, and significant head injuries, while many prior studies did not specify whether these comorbidities were excluded (Scott et al., Reference Scott, Matt, Wrocklage, Crnich, Jordan, Southwick and Schweinsburg2015). In addition, we specifically tested performance validity and excluded individuals who may have exhibited suboptimal effort. Regarding memory specifically, our sample was relatively young compared to many prior samples (e.g., Vietnam veterans, Holocaust survivors). Although studies examining the combined effects of PTSD and aging on neurocognitive functioning have been mixed, the largest effects have been in episodic memory (Cohen et al., Reference Cohen, Neylan, Yaffe, Samuelson, Li and Barnes2013; Golier, Harvey, Legge, & Yehuda, Reference Golier, Harvey, Legge and Yehuda2006; Schuitevoerder et al., Reference Schuitevoerder, Rosen, Twamley, Ayers, Sones, Lohr and Thorp2013). Moreover, most prior effects have been found with narrative (story) memory, which was not assessed in this study.
Our results differ from those of Wisdom and colleagues (2014) and Demakis et al. (Reference Demakis, Gervais and Rohling2008), who found minimal neurocognitive deficits in individuals with PTSD symptoms once performance validity was examined. One reason for this discrepancy may be the differences in diagnostic criteria for PTSD among studies. We used a gold standard diagnostic interview, the CAPS, to establish a PTSD diagnosis, and our comparison group had clear criteria for inclusion/exclusion. In contrast, Wisdom and colleagues (2014) used a self-report measure of PTSD symptoms in individuals drawn from a clinical database, and groups were defined by being split at a specific cut-score. Self-report measures create difficulty in distinguishing between trauma-related PTSD symptoms and global psychiatric distress, and splitting at a cut-score is not ideal for group comparisons in a clinical sample, as groups could overlap significantly in symptomatology. In addition, although the sample from Demakis and colleagues (2008) were medico-legal claimants with symptoms of PTSD, only 22% carried a PTSD diagnosis, which may limit the generalizability of findings.
We additionally examined the relationships of executive functioning and processing speed performance with overall severity of PTSD and with specific symptom clusters. In the whole sample, there was a negative association between executive functioning performance and overall PTSD symptom severity. Yet when we examined these associations within the PTSD group, correlations were small and non-significant. This finding could suggest a threshold effect of PTSD status on neurocognitive functioning, such that once an individual meets diagnostic criteria for PTSD, the severity of symptoms becomes less critical for neurocognitive functioning.
Alternatively, this finding could be due to a restricted range of CAPS scores within the PTSD sample, or to the overall distribution of the CAPS scores. Moreover, partially consistent with our hypotheses, we found a negative association between executive functioning in relation to PTSD clusters of both numbing and hyperarousal symptoms, and a relationship between hyperarousal symptoms and processing speed. Although limited in scope, these results are consistent with prior studies in PTSD (e.g., Flaks et al., Reference Flaks, Malta, Almeida, Bueno, Pupo, Andreoli and Bressan2014; Olff et al., Reference Olff, Polak, Witteveen and Denys2014) and suggest that executive functioning difficulties may be related to dysfunction in prefrontal systems that are involved with complex cognitive control and inhibitory processing. Interestingly, the relationships between executive functioning, processing speed, and PTSD symptom clusters were all non-significant when examined within the PTSD group alone, again suggesting that neurocognitive functioning may be less associated with symptom severity once an individual develops PTSD.
Another primary aim was to explore the clinical significance of neuropsychological functioning in PTSD by examining relationships with specific functional outcomes. Unexpectedly, PTSD symptoms and neurocognitive functioning diverged in their associations with occupational outcomes, such that executive functioning was related to work absenteeism, while only PTSD symptoms were related to presenteeism (i.e., self-perception of occupational performance). Importantly, executive functioning performance uniquely accounted for significant variability in work absenteeism above and beyond PTSD symptoms.
Although studies have reported higher rates of absenteeism in individuals with PTSD and other stress-related mental illnesses (Berndt, Bailit, Keller, Verner, & Finkelstein, Reference Berndt, Bailit, Keller, Verner and Finkelstein2000; Hoge, Terhakopian, Castro, Messer, & Engel, Reference Hoge, Terhakopian, Castro, Messer and Engel2007), no prior studies have examined how neurocognitive difficulties might contribute to these outcomes. Our results suggest that impairment of higher-order cognitive skills may affect work attendance, although the reasons for this relationship are unclear. One possibility is that executive functioning difficulties may relate to the effectiveness with which an individual copes with PTSD symptoms, leading to increased absenteeism.
Another possibility is that individuals with PTSD and executive dysfunction may have difficulty performing their duties, resulting in decreased attendance. In contrast, while PTSD symptoms were negatively associated with presenteeism, neurocognitive variables were not associated with presenteeism. This finding converges with prior studies showing that complaints of cognitive decline are more strongly associated with affective symptoms than objective cognitive performance in clinical populations (Errico, Nixon, Parsons, & Tassey, Reference Errico, Nixon, Parsons and Tassey1990; Richardson-Vejlgaard, Dawes, Heaton, & Bell, Reference Richardson-Vejlgaard, Dawes, Heaton and Bell2009). Thus, one possible explanation is that perceptions of work performance may be similar to perceptions of cognitive functioning in that they are more related to affective symptoms than neurocognitive performance. Our results are limited, however, by the small number of employed veterans in our sample and should be treated with caution until they are replicated and expanded upon.
We also found an intriguing divergence between neurocognitive performance and PTSD symptoms in their relationships with measures of physical and mental health-related QoL. Specifically, while processing speed and executive functioning were associated with physical HRQoL but not mental HRQoL, PTSD symptoms were associated with mental HRQoL but not physical HRQoL. Prior studies in a variety of neurological and psychiatric disorders have found moderate relationships between cognitive deficits and general HRQoL (Andreou & Bozikas, Reference Andreou and Bozikas2013; Mohamed et al., Reference Mohamed, Rosenheck, Swartz, Stroup, Lieberman and Keefe2008; Pirogovsky, Woods, Filoteo, & Gilbert, Reference Pirogovsky, Woods, Filoteo and Gilbert2012), and our findings converge with research showing that better cognitive performance is associated with higher self-reported physical health and lower rates of chronic disease in the general population (e.g., Schnittker, Reference Schnittker2005).
Although it was surprising that cognitive functioning was not related to mental HRQoL, this discrepancy is consistent with research in other psychiatric and neurological disorders showing divergent relationships between aspects of HRQoL and mood symptoms and cognitive performance (e.g., Tas et al., Reference Tas, Brown, Cubukcuoglu, Aydemir, Danaci and Brüne2013; Woods, Scott, Fields, Poquette, & Tröster, Reference Woods, Scott, Fields, Poquette and Tröster2008). Individuals with PTSD and poorer processing speed and executive functioning may have greater medical comorbidities leading to lower self-rated physical health, or they may perceive their cognitive functioning as a physical health concern. Clearly, the contributions of neurocognitive functioning and mood symptoms to functional outcomes in PTSD and related disorders warrant further exploration.
Considered alongside previous studies, our results reinforce the overall complexity of understanding neurocognitive functioning in PTSD and its relationship to comorbidities and everyday functioning. PTSD appears to be a heterogeneous disorder, and there is still much to be learned regarding which individuals with PTSD might evidence deficits and how they might impact occupational, social, or other functioning. Overall, our findings emphasize that neurocognitive dysfunction is not an invariant feature of PTSD (Scott et al., Reference Scott, Matt, Wrocklage, Crnich, Jordan, Southwick and Schweinsburg2015; Twamley, Hami, & Stein, Reference Twamley, Hami and Stein2004) and may depend on the profile of symptoms and severity within certain clusters of symptoms. Further research will be needed to determine which cognitive abilities (e.g., response inhibition) within a domain are associated with dimensional PTSD symptoms, and to investigate other factors not commonly examined, such as PTSD chronicity. Moreover, few studies have examined the associations between neurocognitive outcomes and functional/structural brain changes in PTSD. Such investigations could strengthen understanding of brain-behavior relationships in PTSD and cognition-emotion interactions more generally.
Limitations of our study included a moderate sample size, predominantly male veteran sample, lack of collateral report regarding functioning, and limited employment. Although we used well-validated PVTs, it is nonetheless possible that some patients exerting inadequate effort were included. Moreover, cross-sectional research cannot determine whether these group differences represent acquired dysfunction or pre-existing vulnerabilities. Previous longitudinal and twin studies have suggested that some, but not all, neurocognitive dysfunction observed in PTSD may represent vulnerability factors (Gilbertson et al., Reference Gilbertson, Paulus, Williston, Gurvits, Lasko, Pitman and Orr2006; Marx et al., Reference Marx, Doron-Lamarca, Proctor and Vasterling2009; Parslow & Jorm, Reference Parslow and Jorm2007).
Although the individuals in our sample had psychiatric and medical comorbidities including mTBI and substance use disorders, which decreases our ability to attribute neurocognitive differences exclusively to PTSD, excluding these individuals would have limited the generalizability of our findings, especially to other veterans. PTSD is a disorder that commonly presents with multiple comorbidities, and studying individuals that do not evidence symptomatology from other disorders reduces external validity. However, future studies could benefit from having groups without substance use disorders to further examine specificity of cognitive deficits to PTSD. An additional limitation is the exclusion of ADHD given its high comorbidity with PTSD (Antshel et al., Reference Antshel, Kaul, Biederman, Spencer, Hier, Hendricks and Faraone2013), potentially reducing generalizability.
In conclusion, results suggest that PTSD is associated with neurocognitive deficits that are related to negative functional outcomes. To our knowledge, this is the first study to examine the relationship between cognitive difficulties and functional performance after accounting for the effects of PTSD symptoms. Clinically, our findings suggest that assessment of neurocognitive performance may be beneficial during PTSD treatment, as cognitive dysfunction may influence work and health-related outcomes and have the potential to interfere with progress in treatment. Future studies should include a more in-depth examination of neurocognitive effects on psychosocial and mental health functioning (e.g., manifest measures of work performance), as well as collateral reports from individuals who work or live with participants. Further examination of the cognitive profile of PTSD and ADHD comorbidity would allow for greater generalizability (Antshel, Biederman, Spencer, & Faraone, Reference Antshel, Biederman, Spencer and Faraone2014). Finally, intervention research that examines the influence of neurocognitive deficits on treatment outcomes will be critical (Nijdam, de Vries, Gersons, & Olff, Reference Nijdam, de Vries, Gersons and Olff2015).
Acknowledgments
This work was supported by a Department of Veterans Affairs Career Development Award (IK2CX000772) to Dr. Scott, as well as the National Center for PTSD (NCPTSD). Dr. Krystal’s participation was supported by the National Center for Advancing Translational Science (1UH2TR000960-01), the Department of Veterans Affairs (NCPTSD), the National Institute on Alcohol Abuse and Alcoholism (P50AA12870, M01RR00125), and the Yale Center for Clinical Investigation (UL1 RR024139). Portions of this research were presented at the 2014 Annual Meeting of the American Psychological Association (APA). The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs. The authors declare no conflicts of interest.







