INTRODUCTION
Our ability to use objects to perform familiar, everyday life tasks depends on many factors—our learned knowledge about the form and function of individual objects, the degree to which the object “affords” an action from its visual properties, the goal for a particular substep of the task, and our knowledge of the overall task and the order of the steps needed for completion (the “task schema”; see Humphreys et al., 2001, for a review). Theories differ in their stress on these different factors. For example, Cooper and colleagues (Cooper, 2002; Cooper et al., 2005) and Humphreys and Forde (1998) maintain that everyday tasks are determined by interactions between bottom-up, environmental information (object affordances and learned object–action associations) and top-down knowledge about the task schema. According to this notion, strong bottom-up activation from an object can sometimes over-ride a weakened schema in a patient, so that the patient uses the object in a way that it “affords” rather than the way it ought to be used in the task (e.g., pouring milk into an opened teapot). Similarly, objects may be used in an inappropriate order, because the objects afford an immediate action and there are impaired top-down constraints from task schema (see Forde et al., 2004).
Other theorists, however, emphasize less the role of task schema, stressing instead the possibility that task steps are generated “on the fly” to achieve intermediate goals (cf. Joe et al., 2002). One argument made here is that everyday tasks can be accomplished in many ways, depending on the specific context, so that behavior would be too fixed to be useful, if dependent rigidly on a learned schema for a task. On the other hand, there is considerable consistency in the ordering of the steps in at least routine everyday actions across normal participants, suggesting that normal participants do have stored knowledge about which steps to produce in which order (Humphreys & Forde, 1998). In cases where arguments have been made against schema being critical, relatively complex environments have been examined where patients must inter-leave a series of different tasks in a novel manner (e.g., the “2 × 3” test; Schwartz et al., 1998). Under these conditions, top-down schema may play a reduced role, because the novel situation means that the schema are insufficient for good performance (although see the data presented here).
One critical issue for theories proposing that task schema play a determining role concerns the relations between actions performed with objects in the context of an everyday task, and knowledge of individual object use. For example, Cooper and colleagues (Cooper, 2002; Cooper et al., 2005) propose the existence of two separate networks: one specifying the schema for the task [separately representing the overall task goals, various subgoals (pour water, put granules in the cup), and primitive actions (pick up, pour)], and one specifying stored representations and associated actions for individual objects. The distinction between knowledge of how to use individual objects and how to order subtask goals is supported by neuropsychological dissociations between “script” and single-object action deficits (Rumiati et al., 2001). Of interest, such dissociations can extend beyond the distinction between action and script deficits to include contrasts between how single objects are used when presented alone and in a task context. Buxbaum et al. (1997), Forde and Humphreys (2000), and Schwartz et al. (1995) all report patients who had good access to semantic knowledge of individual objects (e.g., on tasks requiring associated objects to be matched together) but who still made semantic errors when performing everyday tasks. Such cases may arise because information in the schema, about the actions that should be performed in the task, are damaged, leading to inappropriate actions being generated to the objects. According to this idea, actions in the context of a multistep task are generated through the schema (even if it is impaired), even though correct actions might be associated with the individual object representations themselves.
The opposite dissociation, in which objects are used correctly only in the context of action, has been noted by Riddoch et al. (2002). These authors reported a patient who was poor at defining and demonstrating the use of individual objects (indicating a semantic rather than a pure naming impairment) but who used the objects appropriately for everyday actions. Here higher-order knowledge, presumably from a schema for the task, helped to cue the correct actions.
If task schema interact with information about individual objects to influence how objects are used in everyday tasks, then it is possible that performance might vary according to whether familiar or unfamiliar objects are part of the repertoire for the task. Such differences might be expected particularly in subjects who are operating with reduced attentional resources, which may limit particular processes such as error monitoring along with general levels of activation within the networks supporting object–action associations and task schema. Schwartz and colleagues (e.g., see Schwartz, 2006, for a review) have noted that neuropsychological patients with a wide variety of different brain lesions can have problems in everyday life tasks, and have accounted for this in terms of there being a general decrease in cognitive resource that affects tasks requiring sustained, goal-based behavior over time. In explicit models of everyday task performance, this may be captured by there being reduced activation within the networks supporting performance (Cooper, 2002; Cooper et al., 2005), so that inappropriate actions are generated or appropriate actions are generated but in the wrong order. If patients allocate their reduced resource to the task schema rather than to the representations of individual objects, then actions with unfamiliar objects may suffer—given that bottom-up activation from such objects may be weak in the first place. In this case, the schema for the task may over-ride bottom-up activation from individual objects and bias patients toward using familiar rather than unfamiliar implements in front of them. This proposal was tested here. We predict that actions using unfamiliar implements will be omitted, but only in the context of the task.
METHOD
We assessed the performance of five brain-injured patients along with age-matched controls on nine everyday tasks, each of which was made up of familiar objects along with one unfamiliar object (e.g., a nonprototypical teapot, for the task of making a cup of tea). In a separate session, we evaluated the patients' knowledge about the unfamiliar objects when presented in isolation. The difference in familiarity between the control target objects and the experimental targets was evaluated by ten age-matched controls. (See Figure 1 for examples of pairs of teapots and cheese graters.)

Example of target objects used among everyday task objects.
Subjects
Five patients took part (mean age = 51; SD = 18, all men). Four had damage including the frontal lobes (along with damage to other brain regions). The fifth had suffered carbon monoxide poisoning and had disseminated brain lesions including subcortical areas (see Humphreys & Forde, 1998, for an MRI scan) and most prominently around the left intraparietal sulcus (see Table 1 for details of the patients and the lesions). One patient had clear symptoms of action disorganization syndrome (ADS), making abnormal numbers of errors in everyday tasks (patient FK; see Humphreys & Forde, 1998; Forde et al., 2004). The other patients did not present with such marked problems in simple everyday life tasks (see Humphreys & Forde, 1998, for data from patient FL and DS).
Details of the patients

Although the patients form a heterogeneous set, we treated them as a single group, comparing their performance with control participants and, where possible, showing statistical generalization across patients. However, we also present the data from the individual patients, so effects of the magnitude of the disorder (worse in patient FK than the others) and lesion site (involving frontal regions in GA, PH, FK, and DS) can be assessed.
Five age- and sex-matched controls (mean age = 50; SD = 18), without history of brain lesion, were also recruited. A different control group of 10 participants (mean age = 51; SD = 22, six male) rated the familiarity of the control and experimental target objects. All subjects gave informed consent to participate and the project was approved by the South Birmingham Research Ethics Committee. All the data collected were in compliance with the regulations of the School of Psychology, University of Birmingham Research Ethics Committee, and the data are in accordance with the guidelines of the Helsinki Declaration.
Procedure
Evaluation of object familiarity.
Target objects (both control and experimental) were presented one at a time on a table in front of each rater. The raters were asked to judge the familiarity of the target objects using a 5-point scale (1-very unfamiliar to 5-very familiar). The order of presentation for the two types of objects (familiar and unfamiliar) was mixed and randomized. A different randomized order was used for each rater.
Object identification.
In one session (conducted after the everyday tasks), the patients were asked to name and demonstrate the use of all of the objects in the tasks—this included both familiar objects and the unfamiliar (target) objects. The objects were presented the same way as the everyday actions assessment, with all of the objects placed on a table, in random locations, in front of the patients. The patients were asked to name and to make gesture to all of the objects in the task array, with one object being cued at a time, presented in random order. Gestures were made with the patients holding the objects (as they would in the everyday tasks). Gestures were videotaped and scored on the basis of whether the content of the action related to the function of the object (ignoring errors in the orientation of the action). Correct naming was based on generation of the exact name. In a separate session, the same procedures were repeated with patients using only the familiar versions of the target objects, again cued one at a time.
Everyday actions.
The participants performed nine everyday tasks. Depending on the patient, the tasks were either given one at a time or they were administered in a “2 × 3” procedure (see Schwartz et al., 1998), where the nine tasks were grouped into three sets of three tasks. For both the isolated tasks and the 2 × 3 procedure, the objects were placed at random positions on a table in front of the participant (for the 2 × 3 procedure, the objects from different tasks were randomly intermingled). In the isolated task procedure, the participant was simply asked to perform the particular task. For the 2 × 3 procedure, the participants were asked to perform each of three tasks twice, without carrying out the same task consecutively (Schwartz et al., 1998). The 2 × 3 procedure was used with just two patients (PH, DS), who were able to cope with the demands of this situation. The other three patients (FK, GA, FL) all found it difficult to perform even one of the tasks in the 2 × 3 context, and hence the simpler, isolated task procedure was used. The control participants only undertook the more difficult 2 × 3 procedure, providing a conservative test of possible impairment in the patients. For both the 2 × 3 and the isolated task procedures, the participants were asked to use all of the objects to carry out the tasks. The tasks and objects are listed in Appendix 1.
In addition to the experimental versions of the tasks (where one unfamiliar object was used), the patients were also given “control” versions, where all the objects were familiar (a familiar exemplar being substituted for the unfamiliar object). The positions of the objects were matched across the experimental and control conditions. Appendix 1 lists the objects used for each task, and the target objects which altered across the conditions are marked by asterisks. Patients in the 2 × 3 version were given the experimental conditions first (with the unfamiliar implements), followed by the control conditions. For the isolated task procedure, the experimental and control conditions were administered in a random order for each patient.
Scoring
The everyday actions were videotaped and scored according to the task steps and actions carried out by the majority of the control participants (at least 3/5). These steps are listed in Appendix 2, and they conform to the minor subtasks (A2 steps) as defined by the hierarchical action coding system by Schwartz et al. (1991). The A2 steps represent specific subgoals that are achieved by a series of A1 steps (the smallest action units that alters an object's location or state). For example, the A1 steps “open butter lid,” “scoop butter,” “spread butter” are carried out to achieve the A2 step “apply butter to bread,” which in turn contributes toward the main task goal “make a sandwich.” We also scored the occurrence of errors. The error categories were similar to those used by previous investigators (see Humphreys & Forde, 1998; Schwartz et al., 1995), and they are listed in Appendix 3 along with examples of each error type.
RESULTS
Familiarity Rating
The effect of target object type (familiar, unfamiliar) on familiarity ratings was examined by separate analyses based on the means across subjects [familiar(SD) = 4.66(0.40), unfamiliar(SD) = 2.22(0.65)] and across items [familiar(SD) = 4.66(0.65), unfamiliar(SD) = 2.22(0.83)], respectively. Paired t tests revealed significant differences in familiarity ratings between the two types of target object, on both the analysis by subjects [t(9) = 17.3; p < .001] and by items [t(8) = 7.4; p < .001].
Object Knowledge
There were 9 target objects and 44 nontarget (other) objects in the task arrays. In Table 2, we present the data on object naming and gestures to individual objects across the patients and controls. A mixed-design analysis of variance (ANOVA) with Group (control, patient) as between-subject factor, and Object type (unfamiliar target, familiar target, familiar nontarget) and Test (naming, gesturing) as within-subject factors was conducted. As shown in Table 2, the patients' overall object knowledge was significantly worse than that of controls [F(1,8) = 35.88; p < .001]. We also found overall effects of Object type [F(2,16) = 17.43; p < .001] and Test [F(1,8) = 14.34; p = .005]. There was also a significant interaction between Object and Group [F(2,16) = 7.98, p = 0.004], and Object and Test [F(2,16) = 13.30; p < .001] but not between Test and Group [F(1,8) = 4.95; p = .057]. There were no effects of Object Type or Test for controls. In patients, significant differences between naming and gesturing occurred for unfamiliar targets [t(4) = −5.01; p = .007]. For these objects, gesturing was better than naming. However, gesturing did not differ for the familiar and unfamiliar targets (Table 2).
The mean percentage (SD) correct scores for naming and gesturing to unfamiliar (target) and unfamiliar (nontarget) objects by the patients and controls

Everyday Actions With Unfamiliar Objects
We found no effect of practice on the repeated administration of the 2 × 3 task. Loglinear regression was carried out to compare the patients' performance across trials under the two experimental conditions. Factors of Practice (first, second trial), Patient (DS, PH), Condition (Normal, Unusual) were entered into the models. These effects were examined on the following key performance measures: (1) A2 steps completed/A2 steps not completed (see Appendix 2 for a list of necessary A2 steps); (2) total errors/A2 steps completed; and (3) target object omission errors/A2 steps completed. There were effects of Condition × A2 completed/not completed [χ2(1) = 6.44; p = .01]; Condition × total errors/A2 completed [χ2(1) = 10.71; p = .001]; and Condition × target object omission errors/A2 [χ2(1) = 12.92; p < .001]. These effects were not qualified by interactions with either Patient or Practice. For the controls, there was again no effect of Practice on the number of target objects omitted [t(4) = 1.18; p = .31], on the number of other objects omitted (t < 1.0), on total errors (t < 1.0), or the total A2 steps completed (t < 1.0). Consequently, we only used the initial task data to compare performance with familiar and unfamiliar objects, along with the results from the patients who undertook the simplified versions of the tasks once.
Object omissions.
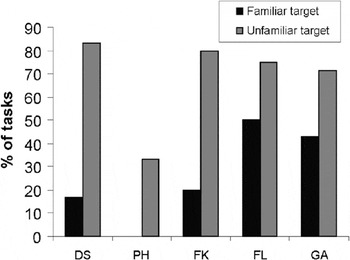
We examined if the presence of an unfamiliar implement increased the likelihood of omission errors. A mixed-design ANOVA was conducted with familiarity of target objects (familiar, unfamiliar) as the within-subject factor and Group (control, patient) as a between-subject factor. There was a significant increase in the omission of actions with the unfamiliar target objects relative to when a familiar object was used [Figure 2; F(1,8) = 24.82; p = .001]. The interaction between Familiarity and Group was borderline significant [F(1,8) = 5.13; p = .053]. There were increased omissions with unfamiliar relative to familiar objects, and for patients relative to controls, even though the controls only performed the 2 × 3 task [t(4) = 4.85; p = .001]. This result held across the patients (Figure 2).

Omissions of actions to the familiar and unfamiliar target object.
We also examined omissions for other (nontarget) objects involved in the tasks using a mixed-design ANOVA (Familiarity × Group). There was no effect of the type of target on the omissions of other objects, for either the patients or the controls [F(1,8) = 0.18; p = .68; interaction F(1,8) = 0.71; p = .42].
General task performance.
To assess any general effects of the unusual implement on task performance, we summed errors on the tasks omissions (of target and nontarget objects), object misuse (of target and nontarget objects), sequence errors, perseverations, additions and spatial errors (see Appendix 3).
A 2 × 2 ANOVA (Familiarity × Group) showed a significant effect of familiarity [F(1,8) = 80.67; p < .001] and a significant Familiarity × Group interaction [F(1,8) = 6.00; p = .04]. With familiar objects, the total errors made by the patients (mean = 11; SD = 6) did not differ from those committed by controls when the unusual implement was present [mean = 7; SD = 2; t(8) = 1.33; p = .22; the mean error rate for controls in the familiar condition was 4; SD = 2]. The total errors made by the patients increased significantly when the unusual implement was present (mean = 18; SD = 6). The errors by the patients were greater when the unusual implement was present than when it was absent [t(4) = 12.78; p < .001], and the patients then made reliably more errors than the controls [t(8) = 3.87; p = .005].
When each error type was examined individually (Figure 3), there was a difference between patients and controls for target omissions with unfamiliar targets [t(8) = 4.45; p = .002]. There were no other differences. Nevertheless, when target object errors (omissions and misuse) were excluded, there remained a significant condition effect (unfamiliar or familiar implement present) for the patients [t(4) = 3.3; p = .03], but not for the controls [t(4) = 1.41; p = .23]. These last results indicate that the presence of the unusual implement extended beyond the implement itself to influence wider aspects of task execution in the patients.

Numbers of errors made by patients and controls.
Goal achievements.
The patients were also assessed on their ability to complete A2 steps leading to the task goal. There were a total of 47 steps to be completed for the 9 tasks (Appendix 2). Despite making frequent omissions with the unfamiliar targets, the patients nevertheless, like the controls, maintained similar levels of steps when this implement was present [Figure 4; for the overall effect of Familiarity, F(1,8) = 4.52, p = .07; for the Familiarity × Group interaction, F(1,8) = 0.14; p = .72]. The patients performed on average 43 A2 steps with familiar targets (SD = 3) and 41 (SD = 4) with an unfamiliar target [t(4) = −1.91; p = .13]. The number of A2 steps completed by the patients when the unusual implement was present did not differ from that of the controls [t(8) = 1.48; p = .17 for the contrast between the patients and the controls on tasks with the unfamiliar implement]. The mean number of A2 steps completed by controls in the familiar condition was 45 (SD = 2), while the controls carried out an average of 44 steps in tasks with unfamiliar targets (SD = 2).

A2 steps completed by each patient and the controls.
Effect of target object knowledge on actions.
The patients were less likely to name the unfamiliar than the familiar targets in isolation (although their gestures did not differ to isolated unfamiliar and familiar targets). Could the problems with unfamiliar implements simply reflect poor recognition? To assess this, we differentiated tasks where patients failed to show any sign of recognizing the target object when it was presented in isolation (e.g., when gesturing; N = 10), from those tasks where patients demonstrated knowledge (N = 35). We found no effect of task type on the proportion of tasks where target omissions occurred (recognized tasks, 20/35; unrecognized tasks, 8/10; Fisher exact probability = 0.27).
Because not all patients had the same list of final tasks with unrecognized objects removed, we computed the percentage of object omissions over the total number of tasks retained for each patient. The patients were still more likely to omit the unfamiliar objects than their familiar counterparts, even with tasks with unrecognized objects removed [t(4) = 4.95; p = .008; Figure 5].
The percentage of tasks where omissions were made to target objects on tasks selected on the basis of the unfamiliar object being recognized when presented in isolation.
The recognized unusual objects also led to an increase in the total errors committed relative to when familiar objects were used [t(4) = 6.71; p = .003]. When target object errors (omission and misuse) were taken out, the difference in total errors with unfamiliar relative to familiar targets was borderline significant [t(4) = 2.75; p = −.052; see Figure 6 for the profile of object errors]. There was again no significant difference between the percentage of A2 steps completed when unfamiliar objects were and were not present, using tasks with recognized objects [t(4) = 1.56; p = .194].

Profile of patients' errors in tasks where the unfamiliar implement was recognized when shown in isolation.
One possibility why the number of A2 steps did not differ across the conditions and groups is that the patients completed the tasks by means other than using the unfamiliar implement. For example, the patients omitted the unusual teapot and made tea directly in the mug. Among the 9 everyday actions, 11 target steps were identified where use of the target object was called for. We assessed the proportional use of target objects, relative to the adoption of other steps to complete the task, for the patients and controls. Figure 7 illustrates the three possible responses to the target steps (when target objects need to be used) by patients and controls. There was no significant difference across the two groups in the distribution of the three types of responses when familiar target was presented [χ2(2) = 4.83; p = .09]. However, in the presence of unfamiliar target objects, the two groups behaved differently [χ2(2) = 18.67; p < .001].

Proportions of target steps missed, target steps completed with alternative means without using the target object, and target steps completed with the target objects, by the patients and controls.
Patients were less likely than controls to use unfamiliar target objects to complete steps [χ2(1) = 16.94; p < .001], and they were significantly more likely to use alternative means to complete the task (without using the target) when the unfamiliar rather than the familiar implement was present [χ2(1) = 15.45; p < .001]. Consequently, there was no difference in the rate of target step omission across the two groups even when the unusual implement was present [χ2(1) = 0.98; p = .32].
DISCUSSION
Task Schema
Our data indicate that brain lesioned patients were more likely than controls to be affected when an unfamiliar implement was present in the context of a familiar task. The patients tended not to use the unfamiliar implement, and, although they typically completed the A2 steps for the task, the patients tended to make more errors across the task when the unfamiliar implement was present. This finding held even when the patients could name and make correct gestures to the unfamiliar objects in isolation. These results held across the patients, and they occurred even though the controls only carried out the more difficult 2 × 3 tasks (as did the two least impaired patients). That the patients also tended to be better at gesturing to individual unfamiliar objects, compared with naming them, may be because the lower visual familiarity of these items affected name retrieval more than object comprehension (see Humphreys et al., 1997), or because gestures could be supported by object affordances (Humphreys & Riddoch, 2003). In either case, the failure to use the objects in the task context suggests that the context had a specific effect, overriding the information otherwise available from the individual stimuli [We note that the patients tended to be better at naming and gesturing to the nontarget objects than the target objects used in the tasks. However, no attempt was made to control the familiarity of the target and nontarget objects, and many of the nontarget objects were more familiar than even the familiar targets (e.g., cup, spoon, milk, vs. teapot). This result is of tangential interest here, given that the study was designed to contrast performance with specific, familiar and unfamiliar target objects].
These findings suggest that, in the brain lesioned patients, there were biases from schema for how familiar objects are used together in a task, leading to omissions of the unfamiliar objects in the task. The result was not confined to the patients with frontal lesions, and we propose that it reflects a more general tendency when brain damage reduces the resources present to support weak bottom-up activation from the (unfamiliar) objects. This would follow if the patients have reduced activation within the networks supporting task schema and the networks supporting associations between individual objects and actions. Under these circumstances, patients may devote their limited resource to schema-based activity and less to weak bottom-up activity from unfamiliar implements, leading to omissions with the unfamiliar objects. Consistent with the argument that the failures to use unfamiliar objects reflect a general reduction in resources, we also found that errors tended to increase even when actions involving the target were not considered, suggesting that the presence of the unfamiliar implement led to increased overall demands, perhaps on how to link the unfamiliar objects with the task schema. With fewer resources to meet these demands, the patients generally generated an increased number of errors.
These data support the argument for task schema playing a determining role in everyday tasks (Cooper, 2002; Cooper et al., 2005). Given that the patients were able to demonstrate how to use many of the unusual implements when presented in isolation, we would expect the unusual implements still to be used if the patients were generating actions “on the fly” on the basis of the individual objects present (cf. Joe et al., 2002). It might be argued that the unfamiliar implements would create some on-line planning difficulties and that this was a critical factor. Against this, though, the patients showed no hesitation in using the isolated unfamiliar objects, and there was no apparent impairment in planning actions under this condition. Rather than this, we propose that top-down activation from task schema led to differential activation favoring familiar over unfamiliar object representations. If the task schema led the patients to devote their limited cognitive resources to objects usually used in the tasks, then this may lead to the exclusion of actions with the unfamiliar objects—a process we label as “schema completion.” It may also be that the patients were less able than controls to generate similar levels of activation from the unfamiliar objects, perhaps because the controls specifically attended to these stimuli based on a supervisory attentional system (cf. Norman & Shallice, 1986), that monitors any mismatch between top-down and bottom-up information. We note that error monitoring will decrease in patients with fewer attentional resources. The net result is that there is a selective increase in target omission errors on trials where the unfamiliar objects were present, for the patients.
Additional Effects of Unfamiliar Implements
In addition to affecting actions to the target objects themselves, the unfamiliar items also influenced errors on other steps in the tasks—the presence of unfamiliar implements induced sequence errors, perseverations, and addition errors (Figure 6). It is difficult to judge the extent to which these extra errors were caused by general difficulties introduced by having the unfamiliar implements present, or whether the effects are due to the omissions of steps using the unfamiliar objects and to attempts to by-pass their omission (e.g., by continuing to use one of the objects present).
Effects From Impaired Task Schema
The present data are also of interest because one of the patients reported here, FK, has been reported as having impaired task schema. For example, FK is poor at generating and ordering the steps making up everyday tasks, a problem that is amenable to remediation by training him with new verbal schema for tasks (Bickerton et al., 2006). Nevertheless, we suggest that any residual schema can still influence his performance, when the objects to be used are unfamiliar. Evidence for effects of a residual schema in FK's case has also been reported previously by Humphreys and Forde (1998). They gave FK verbal instructions for action, which could contravene standard ways of using the objects (e.g., “put the saucer on the cup”). Despite being able to repeat the instructions, FK made many reversal errors in which objects were used in the “standard” manner (e.g., putting the cup on the saucer). We interpret both these previous results and the present results as indicating that schema have not been obliterated, so they still exert some influence on FK's performance. This residual activation is sufficient to override weak input, from individual objects, that does not match the schema knowledge that remains present.
Effects of Personal Familiarity
The present work may also relate to the effects of “personal familiarity” with objects on object use. Patients with semantic dementia may continue to name and use personally familiar objects appropriately (Funnell, 2001; Graham et al., 1999; Snowden et al., 1994), and it is possible that this generalizes beyond the use of single objects to multiple objects in learned (and thus task-appropriate) sequences (Funnell, 2001; Riddoch et al., 2002). In such cases, it has been argued that frequent use of objects can maintain their representations, and possibly also representations for the use of objects in a multiple-object sequence, through episodic memory, even when semantic knowledge of the objects is degenerated. It should be noted that none of our patients suffered from semantic dementia, and all showed a relatively good ability to gesture to the individual unfamiliar objects. This last finding indicates that the failure to use the objects in the context of the tasks does not reflect a poor ability to act to the objects per se, but rather the effects of “schema completion.” Hence, even if the task schema for the patients were maintained by episodic updating (cf. Funnell, 2001), we would still need to suppose that the patients allocated more attentional weight to the schema than to the individual unfamiliar objects, to explain the lack of use of these objects in the task context.
Limitations
One possible limitation of the study is that the patients who performed the 2 × 3 versions of the tasks acted first with the unfamiliar implements before being tested with the familiar implements. This extra practice on the tasks could have improved performance when familiar objects were used. Against this, there were no effects of practice when the repeated versions of the tasks with familiar and unfamiliar implements were compared with the first administration of the tasks. Also, the patients who undertook the 2 × 3 tasks did not differ qualitatively from the patients who undertook the individual tasks, where performance with familiar and unfamiliar implements was tested in a random order. We conclude that practice was not a critical factor.
CONCLUSIONS
The present results match previous single case studies where it has been demonstrated that patients can have intact access to semantic information for single objects and yet mis-use the objects in the context of a task (Buxbaum et al., 1997; Forde & Humphreys, 2000, 2002). Our data suggest that this may be a more general phenomenon, which can be induced in patients under conditions where there is reduced bottom-up activation from unfamiliar objects. In the previous single cases, there may be chronically reduced activation coming from an object recognition system to a representation of the objects in the context of the task, due to attentional weight being devoted to the task schema (cf. Cooper, 2002; Cooper et al., 2005). Our work shows that this may also be manipulated experimentally, by varying object familiarity.
ACKNOWLEDGMENTS
This work was supported by grants from the MRC and the Stroke Association, United Kingdom. We thank all the patients for their kind participation.
APPENDIX 1: TASKS AND OBJECTS USED IN THE STUDY

APPENDIX 2: “NORMATIVE” STEPS REQUIRED FOR THE TASK (AS PRODUCED BY THE CONTROL PARTICIPANTS)

APPENDIX 3: DEFINITIONS OF ERRORS USED FOR SCORING












