INTRODUCTION
With an increasing emphasis being placed on patient-centred care in radiation therapy (RT), the usefulness of qualitative research in, for example, discovering patient perspectives and experiences (e.g. communication and information provision for patients undergoing RT)Reference Halkett, Merchant, Jiwa, Short, Arnet and Richardson1 is becoming evident. Qualitative professionally focussed research involving radiation therapists is also becoming more popular, with research into professional issues and education being prominent topics (such as investigating the perceptions of radiation therapists on reflective practice, patient care and research into advanced practice roles).Reference Cashell2–Reference Bolderston, Lewis and Chai4
Among the various qualitative methods, focus groups (FGs) are particularly useful in exploring knowledge, understanding and personal experiences in relation to specific issues.Reference Kitzinger5 They can also be used when for ethical reasons or time constraints it is not possible for the researcher to go out into ‘the field’ and engage in participant observation. Some of the ethical issues which may arise when undertaking participant observation are related to non-disclosure of the true purpose for being in the field (covert investigation). This may be warranted if the researcher does not want to reveal themselves to the community under investigation, so as not to influence their behaviour.Reference Rice and Ezzy6 FGs allow researchers to elicit both diverse or consensus responses (verbal and non-verbal) from a group of participants at the same time. This technique celebrates diversity allowing researchers to capture hitherto unknown personal attitudes, for example, investigating radiation therapists’ perceptions of the notion of fitness to practise.Reference Wright, Jolly, Schneider-Kolsky and Baird7
This paper will provide a short history of the evolution of FGs and their use in health care research generally and more specifically within RT. It will also address a range of methodological and ethical issues related to the use of FGs, such as the challenges of ensuring a safe environment for free discussion. The paper will conclude with an examination of some of the techniques used to analyse FG data for appropriate and valid evaluation of the themes raised during FG discussions.
Defining and using FGs
FG discussions provide a structured means for researchers to investigate people’s views on a particular subject within a group forum.Reference Kitzinger5 They have been used in the past to study patient, practitioner and service provider experiences of health care.Reference Coyne and Calarco8,Reference Fitzpatrick and Boulton9 The literature suggests that their use in RT research has been limited to a small number of studies, for example, an evaluation of the perception of radiation therapists into the concept of caring.Reference Bolderston, Lewis and Chai4 Anecdotal evidence suggests that smaller-scale local studies have used FGs as a means of clinical/professional governance rather than as research projects. This may be a reason for their paucity as a documented research method used for RT studies in the literature. There are, however, a number of FG studies related to oncology, which are cited in the literature. These include investigations into care of paediatric and adolescent patients, the involvement of users in service planning and investigations into the needs of patients with specific diagnoses (such as prostate cancer).Reference Earle, Davies, Greenfield, Ross and Eiser10–Reference Wallace and Storms12
FGs are defined as
...‘a research technique that collects data through the group interaction on a topic determined by the researcher… It is the researchers’ interest that provides the focus, where as the data comes from the interaction.’... p6Reference Morgan13
The emphasis of this definition lies not only with the group process but also with the interaction between participants. The dynamic interactive nature of FG discussions is one of the reasons why researchers select FGs as opposed to other qualitative methods of data collection.
When to use FG methodology
FGs are well suited for investigating complex and sensitive clinical issues such as those requiring multi-disciplinary research across a number of clinical centres. For example, they could be used across the disciplines of radiation and clinical oncology with multi-disciplinary team members. One example of a topic which could be investigated is the quality of information provided to patients about radiation-induced side effects. This could also be investigated using patients as participants to get their insight into the quality of information that is provided to them on side effects and self-care and what might be required.
FGs can been used as a means of hypothesis generation and also to facilitate the interpretation of surveys.Reference Merton and Kendal14 Their use has been advocated as a preliminary stage for the development of survey tools, to ensure that the survey questions are structured in context with potential participants.Reference Cashell2,Reference Mates and Allison15 Indeed this is how we used them in our research investigating radiation therapists’ perceptions of fitness to practise.Reference Wright, Jolly, Schneider-Kolsky and Baird7 This approach allowed us access to a wide group of practitioners over a relatively short period of time and it provided a forum for participants to input their views and interact with one another. A greater amount of time would have been needed in order to undertake participant observation or individual interviews. The FG can also be used in a variety of other ways for gathering qualitative data.Reference Carey and Smith16 They can be used as a ‘stand alone’ instrument or to provide a multi-dimensional approach to data collection in the triangulation of research methods.Reference Perry, Brooks and Hamilton17,Reference Frey and Fontana18 O’Donnell et al. used a series of preliminary FGs to ensure that their survey questions (on professional behaviour and malpractice of medical practitioners) were constructed clearly, thereby reducing the chance of the participants misinterpreting the questions.Reference O’Donnell, Lutfey, Marceau and McKinlay19 There are circumstances when FG methods may not be the most suitable means with which to investigate a qualitative question. For instance, if a researcher wishes to gain in-depth insight into how individuals feel about a topic and explore on a more personal level themes which arise, or if complete privacy is required, because the informants may have information that relates to a third party’s actions. FGs would also be inappropriate if the researcher wants to establish what someone would do in a situation, rather than what they say they would do, then participant observation may be more suitable.
Differentiating between FGs and other types of qualitative group research
The participatory and interactive nature of FGs differentiates them from other research techniques, such as nominal group data collection, where the ‘group process’ is only evident in presentation of the data, which is gathered from individual interviews.Reference Stewart and Shamdasani20 FGs allow participants to refine their ideas and discuss perspectives on topics, which they may not have previously considered.Reference Morgan21 The difference between FGs and the Delphi process is that FGs do not require a consensus to be achieved within the group.Reference Butterworth and Bishop22 In this way FGs allow topics such as patient’s views on aspects of care to vary without participants feeling they need to conform to the views of the majority of the group. During FGs, the opportunity is provided to acquire the views of the participants and observe their verbal interactions, their intensity and those non-verbal cues that can never be captured by surveys. In our research into fitness to practise in RT, for example, notes were taken by an assistant documenting non-verbal cues when participants were speaking:
JRT2Q4 Pedro – ‘Uses both hands to explain to the group, looking around, is he seeking reassurance from the group or trying to engage the group?’
SRTQ1 Basil – ‘Leans forwards using hands to explain, jumps in and engages the group, uses eye contact, may be to show disagreement?’
Thus, FGs provide researchers with a deeper insight into what people think and feel about a topic.Reference Madriz23 It should be noted, however, that the setting for the implementation of FGs may be considered ‘unnatural’ and not authentic when compared to the environment in which participant observation is undertaken. This is because they are conducted outside of day-to-day ‘real life’ clinical practice and it is for this reason that FGs should not be used as a substitute for investigating ‘lived experiences’.Reference Morgan13,Reference Kidd and Parshall24 Nevertheless, FGs allow the researcher to gather data in a way in which open and frank discussions and the sharing of existing and new ideas are possible. In order to achieve this in our study, an appropriately prepared independent moderator (academic from the field of medical radiation science) facilitated the FG discussions. A pilot FG discussion was conducted to allow the moderator to familiarise themselves with the discussion points. In particular, this enabled the FG prompt questions to be tested, some of which were subsequently modified prior to conducting the FGs proper. The moderator of our FGs ensured that new ideas were explored by the whole group and that the discussion maintained its focus.
ETHICAL CONSIDERATIONS
It is imperative that researchers are cognisant of the potential ethical issues associated with the use of FGs. All research using FGs should be reviewed and approved by the institutional ethics committee (unless this technique is to be used for governance/audit, quality assurance or evaluation purposes and not intended for publication). As with all research studies, the participants should be provided with explanatory information about the nature and conduct of the research and they should consent to voluntary participation, in the knowledge that they can withdraw at anytime without any retribution if in any way they feel that they are unable to continue.
Suitability of the discussion topic for FG methods
The research question should be thoroughly considered to ensure its suitability for discussion in a group environment.Reference Smith25 It is acceptable for topics to be controversial and sensitive in nature as long as the discussion is moderated appropriately and complete anonymity of cases or incidents is maintained throughout the entire discussion. Some topics might be considered sensitive in nature and ethics committees may be wary of approving FGs as the method to collect data on these topics. This may be due to perceived risks in relation to confidentiality or the potential of the related discussions to cause harm or distress to participants. Examples of discussion topics that might be considered sensitive are those associated with children or other vulnerable members of the community. In our study, these were topics relating to personal emotional experiences and those which had potential medico-legal ramifications. These included asking practitioners what they would do if they discovered a colleague was under the influence of alcohol while at work/instructing a student incorrectly/discussing patient details over a social networking site. The potential outcomes of discussing these types of topics needed to be carefully considered because of the potential for participants to disclose their experiences of less than optimal practice (which may have compromised the integrity and reputation of colleagues). On a number of occasions in our FGs, specific examples of unprofessional practice which participants had observed first hand were discussed. For instance, the following example was the first of a ‘snowball’ of other examples of unprofessional practice in RT:
‘people who just, routinely forget to put a piece of shielding in and say, oh yep, she’s right, it doesn’t really matter and the, the old standby where some people just throw away the line “oh it’s only palliative”, which just makes my blood boil.’ SRT-2 Towser
In this FG, once one practitioner had been ‘brave’ enough to speak out and express their emotion and views, others then felt less inhibited and more comfortable doing the same. Although there are challenges associated with sensitive topics being discussed in the group environment, the advantages are that having the support of other participants may encourage those who might not usually divulge experiences to do so. In some cases, when medico-legal issues are discussed in FGs, mandatory reporting regulations may mean that confidentiality post-discussion cannot be guaranteed. This is because there are ethical dilemmas related to the disclosure of potentially harmful information, such as illegal behaviour or behaviour that would signal intervention of a regulatory body (such as inappropriate relations with a patient) or discussion about actions which may have been harmful to others.Reference Minichiello, Sullivan, Greenwood and Axford26,Reference Smith27 Reporting regulations in different countries and perhaps states within countries may, however, vary in their policy relating to this type of disclosure. It is therefore important to prepare the participants for this eventuality. This should be done in the first instance in the written participant information which participants receive prior to agreeing to be involved in the study and again at the start of the FG discussion verbally.
It should be highlighted, however, that with the use of a skilled moderator to facilitate the discussion, sensitive topics can be discussed in the FG environment. This is illustrated in research undertaken on the topic of parents’ end-of-life decisions in childhood cancer.Reference Tomlinson, Capra and Gammon11 This study investigated the process involved when parents of children with terminal cancer have to decide between cytotoxic chemotherapy and supportive care alone. The secondary purpose of this study was to ask participants their views on the appropriateness a series of questions which were going to be used in a subsequent survey, related to end-of-life decisions. The results from this FG led to changes in the design of the subsequent study.
Incentives to participate in FGs
The issue of whether participants should be offered incentives, such as payment for being involved in research is contentious. Payment should not be seen as an ‘inducement’ or reward and, indeed, should only cover travel expenses and costs for inconvenience.Reference Minichiello, Sullivan, Greenwood and Axford26 It is however possible to offer motivational incentives, such as altruistic appeal (for the good of the profession).Reference Morgan28 In our use of FGs, participation was linked via the professional body to the professions’ Continuing Professional Development programme. In this way, credit was given to the radiation therapists for participating, as this was seen as an activity by which they were engaging in critical reflection and analysis of practice. It was also hoped that this strategy would stimulate participation rates. Incentives, such as refreshments, were also used which aided the socialisation of the participants immediately prior to the FG discussion (allowed participants to familiarise themselves with the environment and meet the other members of the group). It is suggested in the literature that in order to increase the chance that interested participants will attend the FG, the researcher needs to keep in close contact with them in the time frame between initial recruitment and conduct of the FG.Reference Morgan21
PRACTICAL CONSIDERATIONS
Participant selection issues
Ensuring that you have the appropriate participants for FGs is paramount to their success. An appropriate sampling technique which provides the researcher with participants who have the desired characteristics for the discussion is important from an ethical and practical perspective.Reference Sarantakos29 Purposive Sampling is the most common sampling technique used in FG research.Reference Miles and Huberman30 This sampling technique allows for participants to be chosen by virtue of their knowledge and understanding on a topic and what they can potentially contribute to the discussion.Reference Curtis and Redmond31 This has been advocated because it generates rich sources of data as participants are informed about the subject and the emphasis is placed on the level of understanding which the participant has on the topic under investigation.Reference Howatson-Jones32,Reference MacDougall and Fudge33 When ‘Purposive Sampling’ is used, the discussion groups are more likely to be consistent in their composition (homogenous), thus the potential for sampling bias and power differentials between participants which may cause ethical issues is reduced.Reference Krueger and Casey34
The effect of familiarity between participants and the facilitator
In a small profession, such as RT, it is likely that if FGs are conducted the participants may know each other. This may affect how comfortable participants feel discussing certain issues. We attempted to overcome this in our research by placing a statement advising participants that they should not disclose any of the information which had been discussed in the FG with anyone outside it. We also highlighted that anonymity of participants in all publications would be ensured (pseudonyms were used for reporting of data).
The effects of familiarity between participants (participants knowing each other prior to the FG discussion) may be potentially restrictive in terms of the flow of the discussion. Also, if participants knew each other prior to the FG, there may have been the chance that they would agree prior to participating not to discuss certain issues.Reference Curtis and Redmond35 If participants are not strangers, the usual secure environment of the FG which allows respect for personal views is compromised and familiarity between participants may to some extent inhibit freedom of speech and opinion.Reference Folch-Lyon, de la Macorra and Schearer36,Reference Saint-Germain, Bassford and Montano37 For example, if a group of radiation therapists who know each other agree before a FG to direct the discussion in a certain way then this would challenge the FG facilitator to elicit honest responses. In order to minimise this in our research, where many of the participants were colleagues, the identities of the participants were not disclosed before the actual FG took place. This was done to minimise the chance of participants entering into discussions with others who were in the same FG as them prior to the event. However, this is not always possible as some participants may collude to attend the same FG together anyway. In our FGs, familiarity between some of the participants in the same group (some participants were work colleagues) helped ‘break the ice’ and potentially made participants feel more comfortable.
In addition to familiarity between participants within the groups, there is also the issue of familiarity of the researcher/FG facilitator with the participants. When undertaking FGs within a relatively small professional group, such as in RT, it is likely that the researcher will be known to the participants. This may introduce a potential power differential between the participants and the researcher, which may be counter-productive and result in certain aspects being omitted from the discussion because of who the facilitator is. In order to eliminate this issue, researchers can use an independent experienced FG facilitator from a related Medical Radiation Science profession (so they have insight into the use of RT and professional jargon and understand some of the issues in the profession that may have arisen in the FG discussion). In our study this reduced the likelihood that the participants would feel obliged to respond in the way they thought would be expected by the researcher. Nevertheless, in some studies it could be advantageous for the participants to know the facilitator, for example, when patients are involved in sharing their experiences on aspects related to their diagnosis as this may be considered a safer environment in which to discuss issues.
The effect of power differentials
Interaction between participants during FG discussions is crucial for their success.Reference Puchta and Potter38 The extent to which the participants of a group contribute to a discussion may be determined by the characteristics of the other members of that group.Reference Fitzpatrick and Boulton9 In order to maximise the success of the FG discussion, it is therefore recommended that the groups are organised to minimise any potential barriers, thus eliminating any power differentials.Reference Ruff, Alexander and McKie39 When undertaking FGs with patients, it may be necessary to use a specific illness as a means of grouping participants together; for example, a FG on the needs of men with prostate cancer.Reference Wallace and Storms12 This is because participants with similar backgrounds and experiences (homogeneous groups) feel more comfortable sharing their views with other group members.Reference Morgan, Stewart, Tudiver, Bass, Dunn and Norton40,Reference Lederman41
If, for instance, a study is being undertaken on members of the RT profession or radiation oncologists, then participants could be grouped according to area of expertise or seniority/promotional level. The latter was done in our study in the hope that it would allow participants to speak freely without their superiors listening. If the groups had comprised a combination of senior staff and recently qualified staff, for example, it may have made the more junior participants uncomfortable sharing their true feelings in the presence of authority figures, particularly when the topic was related to professionalism (fitness to practise). Feedback from our FGs demonstrated that 20 out of the 21 participants felt able to disclose their opinions freely
‘everyone had a say, as much as they wanted.’ SRT-Bobbie
‘I felt comfortable and free to express my opinions.’ SRT-Ryan
‘The group allowed the atmosphere so that I could contribute all that I needed to.’ JRT-Katherine
The participant who indicated that they felt unable to be as open as they would have liked, felt overpowered by a dominant member of their FG. This experience highlights the importance of preparing the moderator to manage situations such as this and ensuring equal participation of all FG members.
The effect heterogeneity
In contrast to the commonly held view that homogenous groups are most effective, group heterogeneity has been favoured to widen the scope of the discussion.Reference Lederman41 Thus, depending on the research question, participants of various rank/seniority could all be allocated to the same group to stimulate ideas.Reference Vaughn, Shay Schum and Sinagub42 This may resemble more closely a realistic workplace environment and as such may be of use given the shift towards multi-disciplinary teams working across professional boundaries, with shared accountability and decision-making in health care.Reference Atkins43 With a heterogeneous group, there is a greater chance of spontaneity in the responses and openness of discussion because there is not as much commitment to the group from the participants.Reference Reed and Payton44 This may be a challenge in RT, however, because radiation therapists continue to be viewed as technicians, and in some respects to hold a non-professional status.Reference Sim and Radloff45
ANALYSING DATA FROM Focus Groups
When analysing qualitative data, there are a series of recommended steps. These include: identification of key themes (immediately after the FGs have been conducted), data transcription, participant checking of the transcripts (for accuracy), coding of the data (including splitting and splicing) and an independent check of the coding.Reference Dey46 The way in which these are undertaken may vary depending on the methodological research framework which guides data collection and analysis.
Thus, in the case of our FG research, the key ideas were identified with the moderator the day after each FG had been conducted.47 Audio tapes and notes of what transpired in the FG discussion were transcribed and reviewed three times. This allowed us to generate a series of ‘big picture’ ideas. After the transcripts had been checked by the researcher, they were sent to participants for verification to minimise misinterpretation.Reference Lincoln and Guba48
We found it useful to use a qualitative data analysis package (NVivo8) to assist in organisation and coding of the data. Additional notes documenting body language and on non-verbal cues were imported into the program for ease of reference during coding. Using an electronic data analysis package facilitated the coding process, but did not replace the need to unitise the data and develop the codes.
Transcripts from our study were coded initially for content and then re-coded using annotations linked to text in order to analyse the nature of individual responses and participant interaction data. Stevens suggests a series of prompts to stimulate questioning of the data which include consideration of a number of aspects, such as dominance of viewpoint, group adherence to the topic, common experiences and contraindications in the discussion.Reference Stevens49 We also created summary documents for each FG during analysis of the transcripts, which contained general ideas and comments relating to words used, their context, internal consistency, frequency and extensiveness, intensity and specificity.Reference Krueger and Casey34
Coding the data
Coding of the data entails gathering related data together into categories and assigning each category a title/code. Dey provides a useful series of steps with which one can analyse the data and suggests that the starting point in data analysis can be a conceptual framework from which preliminary codes can be discerned.Reference Dey46 In the research that we undertook investigating fitness to practise in RT, we found it useful to devise a conceptual framework. This was developed from a review of the literature which we undertook prior to conducting the research. Our initial conceptual framework was a diagrammatic representation of key ideas on the topic (Figure 1) and there were a great number of ‘raw’ concepts, which had yet to be refined. Not all qualitative researchers favour utilising a conceptual framework in this manner; for example, grounded theorists commence with carte blanche and allow the themes to emerge as analysis of the data takes place.Reference Glaser50
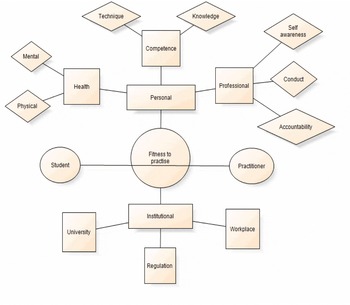
Figure 1. Conceptual framework: A FG study into fitness to practise in RT.
The first phase of transcript analysis is the carving of the data into small units (phrases, sentences and short paragraphs) and assigning them a relevant code. Asking the following questions facilitates the process of coding: What is going on here? Why is this being done? What if something changed? What category does this incident indicate?Reference Strauss51 An example of the initial codes that were created in our first phase of analysis for our research into fitness to practise can be seen in Figure 2. Some of the categories from the initial conceptual framework have been utilised, other themes have been disregarded and there were also new categories created from the data. The categories in Figure 2 were then re-analysed and spliced together to form four main themes, as can be seen in Figure 3, namely: determinants, definitions, regulation and environment for fitness to practise. It is also useful when creating the codes to include a short description of their defining properties, so that the researcher can be reminded of the inclusion criteria for each category.
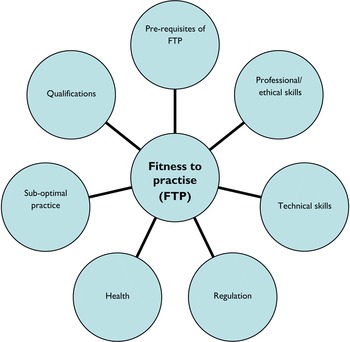
Figure 2. Categories which were developed during initial coding of data from a FG study into fitness to practise in RT.

Figure 3. Final key themes developed after further analysis of codes from a FG study into fitness to practise in RT.
During the next phase of data analysis, each category is then further refined via a process termed splitting, which results in a series of sub-categories of the initial codes.Reference Dey46 We achieved this in our study by concentrating on each code individually and analysing its data. This allowed us to create sub-categories (Figure 4) for the code entitled ‘Determinants of fitness to practise’. With this particular category, there were a plethora of sub-categories, some of which contained only a small number of data units (e.g. the categories of mental health, physical health and self awareness). At this stage, these were considered significant enough to have their own unique codes. However, after further analysis these were spliced together (combined and re-identified by a different code) to form one single code ‘Impairment’. This linking process involves re-reading the transcripts, analysing the units of data with an emphasis on making substantive connections between them, which should be conceptually and empirically based.Reference Dey46Figures 5a,b and 6 demonstrate the outcome of the splicing process for the category ‘Determinants of fitness to practise’.

Figure 4. Initial splitting of a category (determinants of fitness to practise) into nine sub-categories.

Figure 5. (a,b) Examples of splicing categories from the determinants of fitness to practise in RT, creating more inclusive themes.

Figure 6. Spliced categories forming consolidated themes for determinants of fitness to practice.
Content analysis can also be undertaken during data analysis, where frequencies of word occurrence and unitised codes are recorded.Reference Stewart and Shamdasani52 A verification of coding should be undertaken by a second independent researcher who confirms the themes and the codes, which they have been assigned in order to ensure consistency.
If investigators recruit enough participants, then data analysis can be undertaken in conjunction with data collection. In this case, the researchers continue to run their study until saturation of the data occurs. When using FGs, this would be the point where similar themes keep arising from each discussion and no new ones emerge. At this stage, the researcher can be confident that they have captured enough information to assist them in answering their research question. In the case of our research, the number of participants we recruited did not enable us to continue until we could be confident of data saturation, and as such, although data were analysed after each FG, it was not possible to continue conducting them until no new themes emerged.
CONCLUSION
This paper has provided an overview of some of the ethical and practical aspects associated with using FGs in RT. Although this tool is becoming more popular in health care research, including clinical oncology, it has had limited application to date in RT research. FGs are particularly useful for gaining the views of a number of patients or practitioners at one time in an interactive environment. Within the FG environment, the participants have the opportunity to share and elaborate on ideas without needing to reach a consensus. Data acquired from FGs is multi-faceted with verbal and non-verbal cues being recorded for analysis. There are however a number of issues associated with their use, such as the appropriateness of the topic for group discussion, potential power differentials within the group, the effect of group homogeneity/heterogeneity and maintenance of anonymity. Ultimately, it is vital that the researcher ensures that FGs are the appropriate choice for the research question. We found FGs to be a valuable tool in triangulation of our research into fitness to practise in RT. The use of FGs facilitated the collection of preliminary data, which was then used to develop questions for subsequent research.
ACKNOWLEDGEMENTS
The authors would like to thank Dr Margaret Bearman for her advice in the initial stages of writing this article.








