INTRODUCTION
For patients with early stage lung cancer who present with compromised pulmonary function or other comorbidities that preclude surgical resection, stereotactic body radiation therapy (SBRT) has demonstrated survival outcomes that are comparable with surgery.Reference Chang 1 SBRT is typically administered in five or fewer high-dose fractions that conform closely to the tumour volume. This hypofractionated dosing does, however, place patients at risk for radiation-related toxicity, most commonly pneumonitis and chest wall pain.Reference Timmerman 2 Here we report a case of unilateral vocal cord paralysis secondary to radiation-induced recurrent laryngeal nerve injury in a patient who received a single fraction of 30 Gy to the perihilar region for a metastatic recurrence at the left upper lobe of the lung.
Clinical history
A 65-year-old male was found to have a 1·9 cm left lower lobe lung mass with bilateral mediastinal lymphadenopathy after presenting to the emergency department with shortness of breath and worsening chest pain. Needle biopsy revealed non-small cell lung cancer, likely of squamous cell origin. A positron emission tomography-computed tomograpy (PET-CT) showed no evidence of metastatic disease, and the tumour was staged as T1N0M0 (stage IA). The patient had a smoking history of greater than 150 pack-years and was dependent on supplemental oxygen due to chronic obstructive pulmonary disease. Poor functional status and comorbidities rendered the patient medically inoperable and the left lower lobe mass was treated with SBRT in three fractions of 20 Gy, without heterogeneity corrections. The patient tolerated this treatment well and experienced no acute toxicity.
A follow-up computed tomograpy (CT) scan at 1 month demonstrated a second nodule in the left upper lobe. This lesion was followed over subsequent months and remained stable, until a surveillance CT scan performed at 21 months post-treatment showed further growth and increased metabolic activity. A transbronchial biopsy confirmed invasive squamous cell carcinoma. The patient then received a second SBRT treatment to address the left upper lobe lesion consisting of one single 30 Gy fraction, again without heterogeneity corrections, administered under general anaesthesia due to unrelated shoulder pain that prevented proper positioning for treatment. Again, no acute toxicity was reported. A PET-CT performed 12 months later showed a complete metabolic response to treatment.
Beginning at ~15 months after the second SBRT treatment the patient began reporting increasing voice hoarseness. Laryngoscopy revealed left-sided vocal cord paralysis and repeated follow-up imaging showed left perihilar radiation-induced pneumonitis with fibrosis (Figure 1). At this time the patient reported ongoing dysphagia and occasional aspiration with large food boluses but he declined medialisation thyroplasty in favour of speech and swallow therapy after being advised that his symptoms would likely improve gradually. Over the following 2 years he reported moderate symptomatic improvement with a combination of the aforementioned therapy and one injection laryngoplasty. His last recorded clinic follow-up was at 3 years and 5 months after the second SBRT treatment, at which time a surveillance CT confirmed stable disease. The patient expired of unrelated causes 5 years and 3 months after treatment of the left upper lobe lesion.

Figure 1 Computed tomography image at 3 years 5 months post-single dose stereotactic body radiation therapy treatment showing left upper lobe radiation-induced fibrosis and pneumonitis adjacent to the mediastinum in proximity to the path of the left recurrent laryngeal nerve.
DISCUSSION
Metastasis must be definitely excluded when new-onset neurological symptoms arise in a patient with a cancer history, as was done in this case. Damage to peripheral nerves is a serious, though uncommon, complication of radiotherapy (RT) with brachial plexopathy being the most commonly observed form.Reference Forquer 3 The exact mechanism of this toxicity remains to be confirmed; while direct nerve damage may occasionally occur, mechanical compression secondary to surrounding radiation-induced fibrosis is likely the dominant factor.Reference Chaudhry and Akhtar 4 As a result, nerve palsy tends to be a late sequela arising one or more years after treatment.
A retrospective study of 150 breast cancer patients treated with conventional RT after mastectomy revealed that 12 patients developed unilateral vocal cord paralysis, 11 of which occurred on the left side, presumably because the left recurrent laryngeal nerve descends into the thorax, unlike its counterpart on the right.Reference Johansson, Löfroth and Denekamp 5 This study also revealed that the latency period for this specific toxicity may be a decade or more, with one patient developing vocal cord paralysis 25 years after RT.
Fraction size is among the most deterministic of factors leading to radiation toxicity. In addition, recent work suggests that high-grade toxicity may occur more frequently with centrally located lesions.Reference Timmerman 2 , Reference Senthi 6 Considering these findings, the perihilar field and single 30 Gy fraction selected for this patient increase the risk of this type and grade of adverse event. The tumour was contoured with narrow margins, as demonstrated in Figure 2, but the proximity of sensitive mediastinal structures and peripheral nerves places all patients with central lung tumours at risk of toxicity.
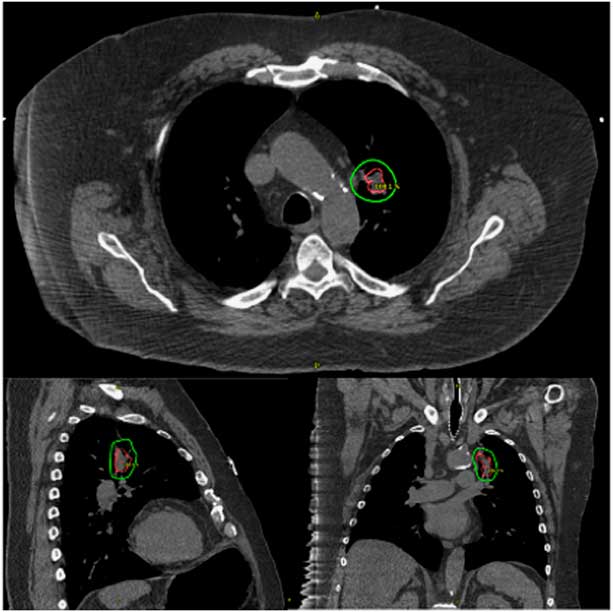
Figure 2 Planning computed tomography for the single fraction 30 Gy stereotactic body radiation therapy treatment of the left upper lobe tumour with the gross tumour volume shown in red and the 30 Gy isodose line shown in green.
Single fraction SBRT schedules have exhibited excellent local control with minimal overall toxicity, particularly if used for peripheral lung tumours.Reference Videtic 7 While the optimal single fraction dose is a topic of ongoing research, a minimum of 30 Gy is associated with significantly improved local control rates.Reference Hara 8 Ultimately, SBRT remains the leading treatment for early stage lung cancer in medically inoperable patients and preliminary results demonstrate lower rates of severe treatment-related adverse events as compared with surgery.Reference Chang 1 However, patients must be followed closely as late toxicities may develop months to years after treatment.
Acknowledgement
The authors would like to acknowledge the contributions of Dr Luqman Dad, who performed the initial evaluation of this patient.
Conflicts of Interest
None.





