INTRODUCTION
Breast cancer is the most common cancer among women worldwide.Reference Ferlay, Soerjomataram and Dikshit 1 About 1·2 million women are newly diagnosed with breast cancer annually in the world, and 521,000 women die of it. Therefore, breast cancer remains the primary cause of cancer mortality in women after lung cancer. A number of randomised controlled clinical trials have shown that breast-conserving surgery combined with postoperative radiation therapy is equivalent to Halsted radical mastectomy, making this an acceptable primary therapeutic strategy for stages I and II breast cancer.Reference Sardaro, Petruzzelli, D’Errico, Grimaldi, Pili and Portaluri 2 , Reference McLaughlin, Ochoa-Frongia, Patil, Cody and Sclafani 3 Adjuvant radiotherapy (RT) for breast cancer in breast conservation is a standard treatment used to improve local tumour control and overall survival, but at the cost of cardiac and lung toxicity and a risk of secondary breast cancer. 4 – Reference Henson, McGale, Taylor and Darby 6 Among all the organs at risk (OARs), the most vulnerable is the heart, with several studies indicating increased risk of cardiac morbidity and mortality, especially with RT treatment of left-sided breast cancer. 7 , Reference Paszat, Mackillop, Groome, Schulze and Holowaty 8 In recent times, volumetric modulated arc therapy (VMAT) has emerged as the most preferred technique over other available techniques like 3D conformal radiotherapy (3DCRT) and fixed-beam intensity-modulated radiotherapy (IMRT)Reference Teoh, Clark, Wood, Whitaker and Nisbet 9 for sites like pelvis and head and neck because of its significantly lesser treatment time and dose conformity. However, its use in treating breast cancer still remains an issue of considerable debate.Reference Zhao, He and Cheng 10 , Reference Jin, Chen, Deng, Liu, Huang and Huang 11
Traditionally, breast RT planning was done on a conventional simulator using simple tangential half beams with a wedge in place. This evolved into 3DCRT with the introduction of computed tomography (CT)-based RT planning. The major advantage of 3DCRT over the conventional technique was its ability to reduce doses to OAR through beam shaping using multileaf collimators (MLC). The introduction of IMRT brought in further improvement in breast RT techniques with better dose homogeneity to target volume and OAR sparing at the cost of low dose spilling over a large volume.Reference Donovan, Yarnold, Adams, Morgan, Warrington and Evans 12 – Reference Donovan, Bleakley and Denholm 14 In the recent past, VMAT has evolved as a much preferred RT technique over IMRT and other conventional techniques.Reference Manikandan, Sarkar, Holla, Vivek and Sujatha 15 While some institutions argue in favour of it, citing better dose distributions and improved sparing of OARs, others believe that VMAT results in larger low dose spillage and poorer organ sparing as compared with other techniques.Reference Zhao, He and Cheng 10 , Reference Badakhshi, Kaul, Nadobny, Wille, Sehouli and Budach 16 – Reference Osman, Hol, Poortmans and Essers 18 In this study, we investigated the relative merits and demerits of VMAT, 3DCRT and forward-planning IMRT (FIMRT) planning techniques in left breast RT in terms of planning target volume (PTV) dose coverage, PTV dose homogeneity and in terms of OAR dose, especially heart dose.
MATERIAL AND METHODS
Treatment plans which were generated for 20 postoperative carcinoma breast patients were included in this study. All patients underwent BCS for left-sided breast carcinoma and were staged to have stage I or II disease according to American Joint Committee on Cancer.Reference Edge and Compton 19 Patients were treated by VMAT technique employing partial tangential arcs. In all the 20 treatment plans the PTV was the breast tissue with appropriate margin as per our institutional protocol. Treatment plans which covered supraclavicular and auxiliary PTVs were not included in this study.
Patients underwent CT simulation on a 16-slice CT scanner (Light Speed; Philips Medical Systems, Amsterdam, The Netherlands) for RT planning. For easy delineation of the breast volume, a copper wire was placed encircling the complete breast volume. CT simulation was done with 3-mm slice thickness extending from hyoid bone to 8 cm below the ipsilateral intramammary fold. The contouring was done on a Monaco Sim (V5.00.02; CMS Elekta, Sunnyvale, CA, USA) contouring workstation. All patient treatments were planned using partial arc VMAT in Monaco treatment planning system (TPS) (V5.00.02; CMS Elekta) and treated on Elekta Synergy (Elekta, Crawley, UK) linear accelerator. The 3DCRT and FIMRT planning were done in CMS XIO (V5.00.01.1) (CMS Elekta) TPS. The 3DCRT planning consisted of conventional medial and tangential wedge portals with MLC field shaping conforming to the target volume. Relative beam weights and the wedge angles were iterated until a homogeneous dose distribution was obtained. In FIMRT planning, smaller supplementary MLC shaped fields were added to the primary open tangential (medial and lateral) portals. In both 3DCRT and FIMRT plans, half beams were used to avoid beam divergence into lung, except for the subfields in FIMRT. In all plans a 2-cm-wide flash margin was used to account for PTV motion due to breathing. In 3DCRT and FIMRT plans, the isocentre was placed in the mid plane of PTV in the craniocaudal direction. In the anterior–posterior direction it was judiciously placed in such a way that minimum possible lung tissue was included in the path of the beam. In the VMAT technique, dual tangential arcs were used, with the gantry traversing the arc length first in the clockwise and then in the anti-clockwise direction. The beam arrangement resembled a typical 3DCRT portal arrangement. The arc length used was 30°. Longer arc lengths were not used as they would have compromised OAR doses with negligible benefit on dose coverage and conformity.Reference Jin, Chen, Deng, Liu, Huang and Huang 11 The isocentre for these tangential arcs was chosen at the centre of the breast PTV in the craniocaudal direction and in the centre of breast tissue. Figure 1 shows the VMAT, 3DCRT and FIMRT plan for the same patient. For all the plans generated the following metrics were scored: V105%, V100%, V95%, mean dose (for PTV), V5%, V20%, D2cc and mean dose (for OARs). Besides these metrics, number of monitoring units (MUs), ratio of number of MUs to prescribed dose (IMRT factor), conformity index (CI) and homogeneity index were also scored for all the plans.
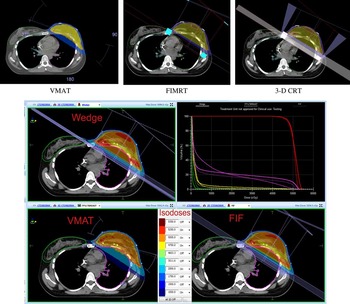
Figure 1 VMAT, FIMRT and 3DCRT dose distribution. Abbreviations: VMAT, volumetric modulated arc therapy; FIMRT, forward-planning intensity-modulated radiotherapy therapy; 3DCRT, 3D conformal radiotherapy; FIF, field-in-field technique.
RESULTS
Mean age of the patients was 48·3±11·3 years. For an experienced planner, a typical VMAT plan needed more than two optimisation runs, consuming overall planning time of 1–1·5 hours in all. In comparison, a typical 3DCRT plan took only 15 minutes and an FIMRT plan took longer time of about 1·5–2 hours.
The mean PTV volume for 20 patients was 1,074·6±405·1 cc. Table 1 shows dose–volume histogram statistics for the breast PTV for three planning techniques. Among them, the highest PTV dose coverage was observed in the 3DCRT technique with 94·1±1·8% of the breast PTV receiving 95% of the prescription dose (V95%). However, it was also observed that this technique resulted in 21·3±10% of the PTV receiving more than 105% of the prescription dose (V105%), which was highest among the three techniques. In contrast, VMAT yielded the lowest values for V95% (93·0±1·8%) and V105% (3·3±5·5%).
Table 1 Planning target volume (PTV) dose–volume parameters and their statistical significance

Notes:
a RXD stands for prescription dose.
Statistical significance was calculated for pair of <VMAT-3DCRT> and <VMAT-FIMRT>.
Abbreviations: VMAT, volumetric modulated arc therapy; MU, monitoring unit; IMRT, intensity-modulated radiotherapy; CI, conformity index; 3DCRT, 3D conformal radiotherapy; FIMRT, forward-planning intensity-modulated radiotherapy therapy.
Statistical analysis was done to check the compatibility of different plan metrics using paired sample t-test. Table 1 shows different plan metrics and the average results for the 20 cases considered and planned with three different techniques. Statistical analysis between the results for VMAT and 3DCRT plans revealed that the mean dose to PTV and PTV V95% were not significantly different between the two techniques (p=0·21). Similarly, no statistical significance was observed between the results of VMAT and FIMRT plans for these two metrics (p=0·88). However, PTV V105% was statistically different in both comparisons—between VMAT and 3DCRT (p=0·01) and between VMAT and FIMRT (p=0·01).
Doses to different OARs are presented in Table 2. Statistical significances for the different metrics were computed using paired sample t-test for the two comparisons: VMAT and 3DCRT, and VMAT and FIMRT. The lowest value of dose to 2 cc of heart volume (D2cc) was observed in the case of VMAT plan (2,764·7±766·8 cGy). FIMRT and 3DCRT delivered significantly higher D2cc dose of 3,494·8±1,419·1 and 4,337·1±1,208·9 cGy, respectively. D2cc heart dose differences between VMAT and FIMRT were 730·1±1,613·0 cGy and statistically different (p=0·02). Difference of D2cc dose between VMAT and 3DCRT was 1,572·1±1,431·6 cGy and was significantly different with p≤0·01. Mean heart doses for VMAT, 3DCRT and FIMRT were 305·5±100·9, 458·8±255·6 and 290·3±122·0 cGy, respectively, and were comparable between <VMAT-3DCRT> and <VMAT-FIMRT> and were not statistically significant (p>0·11 and 0·8, respectively).
Table 2 Statistical significance for <VMAT-3DCRT> and <VMAT-FIMRT> plan for organs at risk

Abbreviations: VMAT, volumetric modulated arc therapy; 3DCRT, 3D conformal radiotherapy; FIMRT, forward-planning intensity-modulated radiotherapy.
For the ipsilateral lung the average mean doses were 656·1±231·7, 672·9±366·6 and 522·1±277·9 cGy for VMAT, 3DCRT and FIMRT, respectively, and were found to be comparable between the techniques with p=0·86 and 0·14 for <VMAT-3DCRT> and <VMAT-3DCRT>, respectively. No significant differences were observed between the techniques for V20Gy (ipsilateral lung) with p=0·34 and 0·36 for <VMAT-3DCRT> and <VMAT-FIMRT>, respectively. V5Gy values for ipsilateral lung were 30·4±8·3, 17·7±8·2 and 14·2±6·5% for VMAT, FIMRT and 3DCRT, respectively, and statistical analysis of these values showed that they were dependent on the technique (Table 2). The mean doses for contralateral lung were 42·3±16·7, 37·4±6·6 and 25·5±5·1 cGy and for contralateral breast were 84·4±34·3, 58·8±32·2 and 70·3±77·5 cGy for VMAT, 3DCRT and FIMRT techniques, respectively. Contralateral lung mean dose for VMAT was found to be significantly different from that of 3DCRT (p=0·03), but was comparable with that of FIMRT (p=0·42). Contralateral breast mean doses were similar in all techniques. Evaluation of Radiation Therapy Oncology Group CI, heterogeneity index and homogeneity index revealed that, for all compared techniques, VMAT exhibited highest conformity (0·8±0·03), minimum heterogeneity (1·17±0·02) and minimum homogeneity (0·15±0·02). FIMRT showed intermediate CI of 0·7±0·06 and 3DCRT showed lowest CI of 0·64±0·08 (Table 1), maximum homogeneity index was observed in 3DCRT plans. Among the three techniques studied, VMAT required maximum number of MUs with a mean value of 561·3±74·9 followed by 3DCRT and FIMRT with values of 310·5±49·3 and 227·1±8·2 MU, respectively. IMRT factor for three techniques were 2·8±0·4, 1·6±0·2 and 1·1±0·0, respectively (Figure 2).

Figure 2 Comparison of different organs at risk doses between FIMRT, VMAT and 3DCRT. Panel (a) shows dose received by 2cc of heart volume; panel (b) shows % volume receiving 20Gy dose for heart and ipsilateral lung; panel (c) shows mean dose for heart and ipsilateral lung; panel (d) shows mean dose to contralateral breast and contralateral lung.
DISCUSSION
Treatment planning of breast cancer in general has always remained a challenging task. Many different techniques have been attempted but we are still seeking an ideal solution. Although the VMAT technique enjoys inherent dosimetric advantages, its use in breast planning remains a debatable topic with two diametrically opposite views—one in favour of it and another against.
Our study was designed to compare the three techniques in terms of plan quality and monitor unit efficiency. We chose left breast as the site for this purpose as it posed the maximum challenge due to the underlying anatomy, and due to the fact that associated long-term toxicities differ significantly while treating right breast cases and left breast cases.
The results of our study clearly demonstrate that fewer MUs are required in 3DCRT and FIMRT as compared with VMAT. However, results are in favour of VMAT technique when doses to OARs are considered. After an extensive literature survey we could not discover any paper which substantiates this result.Reference Zhao, He and Cheng 10 , Reference Jin, Chen, Deng, Liu, Huang and Huang 11 , Reference Badakhshi, Kaul, Nadobny, Wille, Sehouli and Budach 16 – Reference Osman, Hol, Poortmans and Essers 18 VMAT technique consistently scored lower values for all the evaluated parameters for the heart (D2cc, V20Gy, V30Gy and V40Gy) except for its mean dose. VMAT plans were preferable over other plans in terms of PTV highest conformity and lowest heterogeneity. Both FIMRT and VMAT techniques produced comparable plans in terms of PTV coverage and OAR doses except for the heart. However, FIMRT is a labour-intensive technique requiring longer treatment planning time. Besides, the outcome of FIMRT plan strongly depends on the personal expertise of the planning physicist or the planning dosimetrist. On the other hand, VMAT plans were relatively simpler to generate facilitated by readily available standard templates from plan library, requiring only minimal changes during the optimisation depending on the individual patient anatomy.
Heart and left anterior descending artery are the most vulnerable organ in left breast treatment. Until the 1950s, the heart was not exposed to high doses of radiation as the techniques were limited to using orthovoltage X-rays having very limited penetration capability. However, the advent of megavoltage techniques in clinical practice during the late 1950s changed the scenario resulting in higher cardiac doses and substantial increase in cardiac toxicities as recorded in the 1960s.Reference Stewart and Fajardo 20
The severity of the problem associated with RT-induced cardiac toxicity did not become widely recognised until the 1990s, when randomised trials in early-stage breast cancer established that adverse cardiac effects completely overshadowed the survival benefits achieved with RT. 21 Rutqvist et al.Reference Rutqvist, Lax, Fornander and Johansson 22 demonstrated from a clinical trial in the 1970s that the risk of death in women from ischaemic heart disease, who had received left wide-tangential field irradiation, was 3·2 times greater (p<0·05) than the risk in non-irradiated controls. More recent publications report that rates of major coronary events increase linearly with the mean dose to the heart by 7·4%/Gy, with no apparent threshold.Reference Darby, Ewertz and McGale 5 No threshold indicates the advantage for the patient to achieve as low as possible heart dose. Reduction of heart dose is strongly dependent on the beam arrangement. Zhao et al.Reference Zhao, He and Cheng 10 compared dosimetric characteristics between two-field IMRT, four-field IMRT, single arc VMAT and tangential arc VMAT concluding that the two-field IMRT was superior in all dosimetric aspects. The disadvantage in their study was that they used an arc length of 40° for their dual arc VMAT fields possibly resulting in the increased low dose spillage to the ipsilateral lung and cardiac dose significantly observed in their study. We premised that the VMAT arc length needed an optimisation.
Jin et al.Reference Jin, Chen, Deng, Liu, Huang and Huang 11 compared different techniques in treating small-sized left breast, using conventional tangential field arrangement, field-in-field technique, tangential IMRT technique, multi-beam IMRT technique and VMAT technique. They concluded that tangential IMRT technique was the preferable technique over others and VMAT should not be used for small-sized left breast treatment. Although they have not mentioned the arc lengths they used in their VMAT planning, it was obvious from their figure that the lengths were suboptimal. Contrary to their claim, a two-field IMRT beam arrangement cannot produce any significant fluence modulation to reduce the heart or ipsilateral lung dose appreciably.
One common underlying observation from all investigators is the reported advantage of using tangential field arrangement. This emphasises that the preferred beam arrangement for treating breast should be classical tangential type. Any other beam arrangement will certainly deteriorate the plan quality. However, it is also known that VMAT technique is capable of better PTV coverage. In our study, we tried to gain from both the worlds: using classical tangential field arrangement and at the same time using VMAT fields albeit with arc length limited to 30°. In a separate study, we have demonstrated how we arrived at 30° as the most optimal arc span (under peer review in another journal).
CONCLUSION
For the left breast irradiation we compared three different planning techniques, namely, 3DCRT, FIMRT and VMAT, in terms of dose coverage to PTV, dose to OARs and total number of monitor units required. Based on our results, we conclude that among the three techniques, VMAT plans with limited arc lengths will result in minimum possible heart doses and should be the choice of technique for the left breast irradiation. Even though the VMAT technique required more MUs as compared with the other two techniques, it is still preferable as the treatment delivery time is very short.
Acknowledgement
The authors thank Sonal Goswami for her support in preparations during the study.







