Introduction
Primary cardiac sarcomas (PCSs) are rare with the commonest type being angiosarcoma, and least reported are intimal sarcomas. They are locally aggressive with usually delayed presentation. Echocardiography is the main diagnostic test. Magnetic resonance imaging/computed tomography (MRI/CT) and positron emission tomography–computed tomography (PET-CT) can help in identifying the local extension and distant metastasis. Surgery with negative margins is the mainstay of treatment. Role of Adjuvant therapy has not been studied due to the rarity of the tumour. Chemotherapy regimens containing anthracyclines, ifosfamide or taxanes have been reported. Postoperative radiotherapy (RT) to a total dose of 60 Gy can be tolerated with minimal side effects.
A 59-year-old male with history of hypertension and diabetes mellitus presented to the emergency department with dizziness on exertion for 2 weeks. No history of chest pain, cough or shortness of breath. Chest radiograph was normal. Echocardiography showed ejection fraction of 65% with mild left ventricular hypertrophy. There was a right ventricular outflow tract (RVOT) mass measuring 5 × 2·5 cm protruding to the pulmonary artery (PA). Computer tomography of chest revealed large non-enhanced filling defect in the right ventricle (RV) extending to the PA. There was a small non-occluding defect in the right pulmonary artery (RPA). Cardiac MRI showed a well-defined RVOT/pulmonic valve mobile mass protruding into the main PA during systolic phase causing an occlusion (Figure 1). Patient had no abnormal signs on physical examination. He underwent resection of the RVOT and the RPA with reconstruction. Histopathology showed intimal sarcoma with positive margins throughout the myocardium. PETCT post-surgery showed no evidence of local or distant metastasis. In view of positive margin, he received adjuvant RT to the post-operative bed. Simulation was done using four-dimensional CT. The dose was 60 Gy in 30 fractions daily using 6 MV energy with intensity modulated radiotherapy (IMRT) technique. Daily cone beam CT was used for verification. Plan evaluation showed that 100% of the dose covered 94% of the planning target volume (Figure 2). Heart mean dose is 22 Gy, V30 is 30%. Left lung V20 was 28%, mean is 16 Gy. Patient tolerated treatment well with only side effect of minimal dysphagia. Echocardiography was done during middle of the treatment and showed ejection fraction of 52%. Three months post RT, patient was doing well, and CT images showed no evidence of local recurrence or distant metastasis.

Figure 1. Pre-op MRI showing the lesion (red arrow).
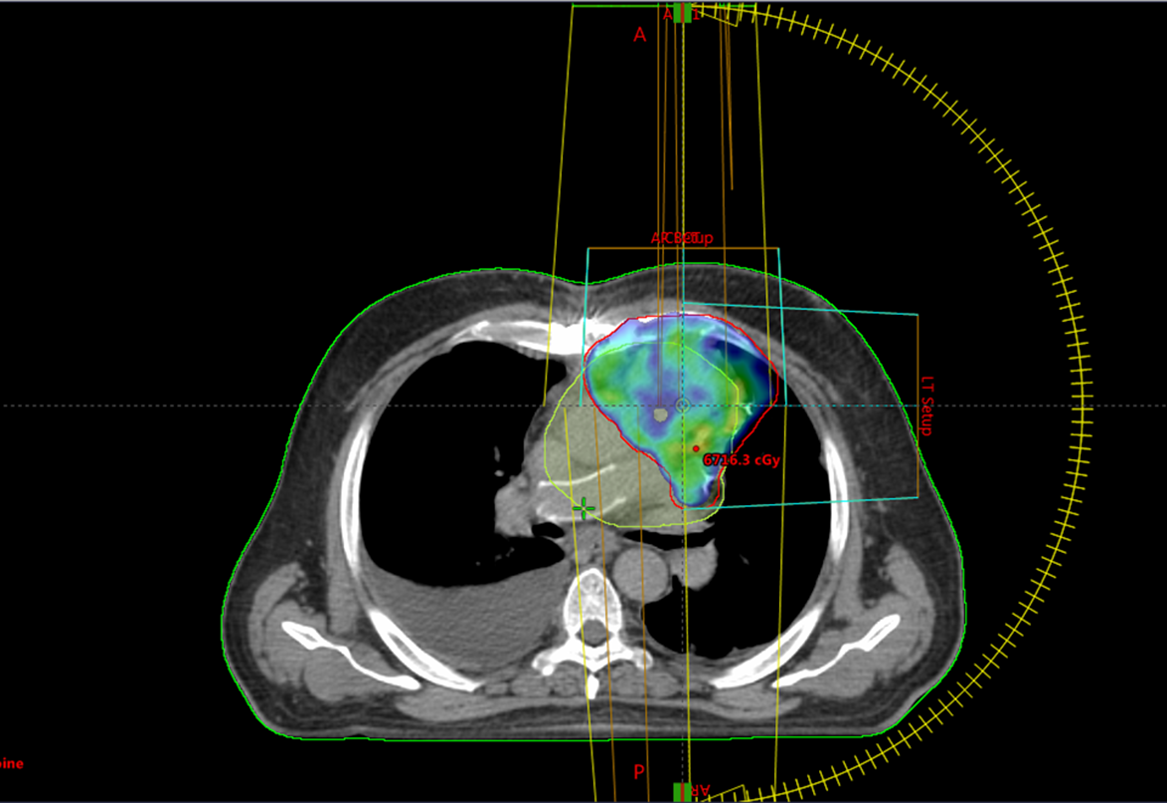
Figure 2. Axial image showing the 95% isodose line in colour wash.
Primary cardiac tumours are extremely rare with an incidence of 0·001–0·03% in autopsy series. Reference Butany, Naseemuddin and Nair1 A quarter of these tumours are malignant, of which sarcomas are the most common. PCSs represent around 1% of all soft tissue sarcomas, and the median age at presentation is 39–44 years. Reference Gupta2
Angiosarcomas, undifferentiated sarcomas, and undifferentiated pleomorphic sarcomas are the most common types, Reference Butany, Naseemuddin and Nair1 and the least reported are intimal sarcomas. Reference Ibrahim, Luk and Singhal3 The latest arise usually from the large vessels such as pulmonary trunk. PCSs are locally aggressive with usually delayed presentation that may lead to myocardial infiltration, outflow obstruction and distant metastasis.
Echocardiography is the main diagnostic test. Features suggestive of malignancy are broad-based atrial masses in non-septal locations and extension into the pulmonary vein. Reference Kim, Beak and Kim4 MRI, CT and PET can identify the local extension and distant metastasis. Up to 80% of patients have distant metastasis at the time of diagnosis. Reference Devbhandari, Meraj, Jones, Kadir and Bridgewater5
Surgery with negative margins is associated with increased survival and is the mainstay of therapy; however, it is difficult to achieve because of the limited amount of myocardium. It is associated with acceptable mortality, and patients with a radical resection at the first surgery had a longer median survival (MS) of 17–24 months compared with patients with a partial resection with MS of 6–10 months. Reference Pacini, Careddu and Pantaleo6,Reference Simpson, Kumar and Okuno7 Adjuvant chemotherapy and RT are widely used in soft tissue sarcomas of the extremities, improving survival, and could be considered for PCS. A retrospective chart review of 12 patients with PCS who had local excision with post-operative therapy showed improvement in the OS compared with surgery alone. Reference Wu, Million, Moding, Scott, Berry and Ganjoo8 Chemotherapy regimens containing anthracyclines, ifosfamide or taxanes have been reported. Reference Schur, Hamacher and Brodowicz9
Role of adjuvant RT is not clear due to the rarity of the tumour. In a retrospective study of the French Sarcoma Group, RT was associated with improved (PFS) on multivariate analysis. Chemotherapy was significantly associated with better OS only in non-operated patients but not in operated patients. Reference Isambert, Ray-Coquard and Italiano10 Adjuvant RT is usually indicated in cases of close or positive margins or large, high-grade tumours. It has been used in some patients with cardiac sarcomas, but its efficacy has not yet been studied. Another retrospective analysis with eight patients diagnosed with PCS including three intimal sarcomas treated with resection followed by adjuvant RT to a mean dose of 60 Gy showed that MS is 24 months with the documented side effects of dizziness and fatigue. Reference Moeri-Schimmel, Pras, Desar, Krol and Braam11 It is important to realise that with the new RT technologies, for example, IMRT, organs at risk and part of the non-involved heart could be spared. The consequence of the inclusion of the heart in a radiation field is acute and chronic radiation-induced heart disease (RIHD). In a retrospective study to evaluate the short- and long-term clinical and echocardiography changes in patients with cardiac sarcomas treated with IMRT, 20 patients with PCS were treated with IMRT with mean follow-up of 31 months. At the end of RT, 3 patients had atrial fibrillation (AF), which was cardioverted with amiodarone, and one had acute pericarditis, treated with non-steroidal anti-inflammatory drugs for 1 week. Long-term therapy was not needed. The left ventricular ejection fraction (LVEF) was 52–70%, decreased by −1% to −10% in ten patients. Reference Lestuzzi, Cosei and Ravasel12
There is no consensus about the RT dose; however, it could be extrapolated from non-cardiac sarcomas. In a recent series done by the French Sarcoma Group, the dosimetry data of 12 patients were analysed. It showed that a regimen of 45 Gy in 1·8 Gy per fraction to a pre-operative volume with an additional dose of 14 Gy in 7 fractions on residual disease is a reasonable dose. Reference Thariat, Clement-Colmou and Vogin13
Conclusion
PCS is a rare malignancy. It has a dismal prognosis. The mainstay treatment is surgical excision. Post-operative RT using IMRT has a role in improving local control and PFS. A dose of 60 Gy is tolerated with minimal toxicities.
Acknowledgements
None.
Financial Support
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Conflicts of Interest
None.





