Introduction
The last three decades have seen a rapid growth in the practice of controlled organ donation after circulatory determination of death (cDCDD).Reference Smith, Dominguez-Gil, Greer, Manara and Souter 1 cDCDD is endorsed by the World Health Organization and its increasingly widespread use has offered a welcome expansion of the donor pool.Reference Morrissey and Monaco 2 Yet, despite growing acceptance and implementation of cDCDD in many jurisdictions, ethical controversy surrounding aspects of the practice remains present in the medical and bioethical literature.Reference Kirby 3 Points of dispute are reflected in variation in protocol worldwide.Reference Jericho 4 While authoritative bodies and expert panels endorse cDCDD, 5 these consensus statements often do not engage substantively with prominent debates in the ethical literature.Reference Joffe, Carcillo, Anton, deCaen, Han, Bell and Maffei 6 As a result, the myriad nuanced points of ethical contention may fail to penetrate, or be appreciated within, policy and practice. The increasingly vast literature on the ethics of cDCDD makes it difficult for stakeholders, the public, and particularly clinicians to keep up to date on the various conceptual and ethical issues associated with this practice. This may lead to moral distress among clinicians performing cDCDD,Reference Steinbrook 7 the avoidance of practicing cDCDD so as to obviate these controversies, or, potentially, unethical practice. It is critical that stakeholders are sufficiently aware of, and engaged with, the breadth of ethical views and considerations related to the practice, regardless of their currency in the donation and transplant community. For these reasons, this review offers a synthesis of the prominent conceptual and ethical issues surrounding cDCDD. While it is not feasible in a single article to provide a comprehensive accounting of all ethical issues, arguments, and considerations related to cDCDD, let alone to do justice to their many nuances, we believe that this review serves as a vital resource which maps the contours of this ethical terrain, and which signals to those working in this area the prominent locations where further nuance and discussion can be found.
Before proceeding, it is worth noting that the exercise of synthesizing ethical issues, arguments, and considerations can appear to present a phenomenon in a negative light. In other words, by identifying and discussing numerous ethical worries, one may get the sense that a practice is unethical, or that a practice like cDCDD is without ethical merit. This is not our intention. This scoping review is part of Neurological Physiology After Removal of Therapy (NeuPaRT), an interdisciplinary project exploring brain function at the end of life that will contribute to a clearer understanding of the physiological process of death in cDCDD. The goal of this review is not to criticize cDCDD, but instead to offer a neutral resource which enables stakeholders to familiarize themselves with its ethical landscape. We outline commonly discussed ethical issues bearing on cDCDD, identify key themes, concepts, and arguments, and provide an overview of notable debates. Importantly, since a number of conceptual ambiguities and empirical uncertainties bear on cDCDD, we seek to furthermore to distinguish between those issues that are resolvable through empirical study, those that are subject to resolution through normative argument, and those that are subject to ongoing disagreement given intractable metaphysical commitments. Progress can be made on the first two sets of issues, but the third will always present tensions, no matter how much empirical data or cogent ethical argument we produce. We conclude that while some ethical debates concerning cDCDD may be resolved through further empirical research and ethical dialogue, others will not be. The plurality of viewpoints surrounding some issues is a result of longstanding debates on the metaphysics of death and inherently value-laden judgements concerning the legitimate scope of medical practice. Further dialogue, public engagement, empirical study, and ethical analysis are required as cDCDD continues to advance and grow in complexity.
cDCDD: A Brief Introduction
Controlled organ donation after circulatory determination of death — sometimes referred to as donation after cardiac death, donation after circulatory death, or non-heart-beating organ donation — refers to the recovery of transplantable organs after death is determined based on circulatory criteria (as opposed to death determination based on neurological criteria). Donation after circulatory determination of death is “controlled” when the timing, location and manner of withdrawal of life-sustaining measures are planned and supervised; donation after circulatory determination of death is “uncontrolled” when circulatory arrest is unplanned, typically occurring outside of a hospital setting. cDCDD is therefore generally performed with patients dependent on life-sustaining treatments within an intensive care unit who do not meet criteria for neurological death but who are expected to die within a short period after treatment withdrawal.
Controlled organ donation after circulatory determination of death — sometimes referred to as donation after cardiac death, donation after circulatory death, or non-heart-beating organ donation — refers to the recovery of transplantable organs after death is determined based on circulatory criteria (as opposed to death determination based on neurological criteria). Donation after circulatory determination of death is “controlled” when the timing, location and manner of withdrawal of life-sustaining measures are planned and supervised; donation after circulatory determination of death is “uncontrolled” when circulatory arrest is unplanned, typically occurring outside of a hospital setting.
Protocols mandate that discussion regarding surrogate consent for cDCDD can only occur following consent to withdrawal of life-sustaining measures. After surrogate consent for cDCDD is obtained, life-sustaining measures are continued during donor workup and until such time as suitable recipients are identified and an organ recovery team is assembled. Depending on the protocol, withdrawal of life sustaining measures commonly occurs in either the intensive care unit or the operating room.Reference Aulisio, Devita and Luebke 8 The process involves protocolized removal of life sustaining treatments combined with the administration of pain and anxiety relieving medications. Antemortem interventions such as the administration of heparin, steroids, antibiotics, and/or cannulation of femoral vessels to facilitate post-mortem mechanical reperfusion of organs are performed in some jurisdictions in order to promote organ viability.Reference Dalle Ave, Shaw and Bernat 9 A specified number of attending physicians who are not part of the transplant team determine death after a “no-touch” period following asystole. The transplant team commences organ recovery only after the elapse of the no-touch period. In some protocols, in situ post-mortem normothermic regional perfusion is initiated after declaration of death to reverse ischemic organ damage and enable organ graft optimization prior to transplantation. 10
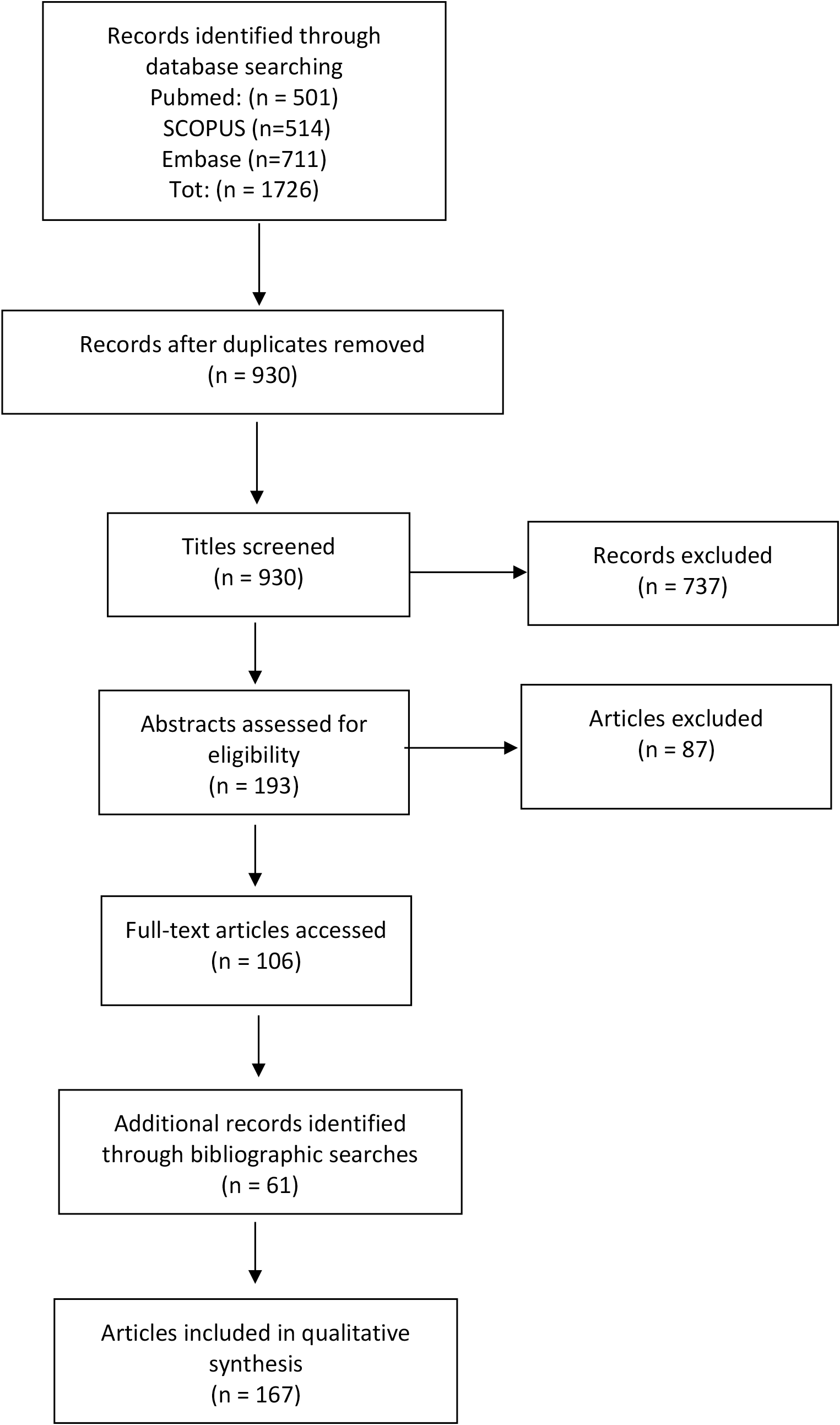
cDCDD differs markedly from donation after neurological determination of death (DNDD) insofar as time constraints are of paramount concern. In DNDD, determination of death does not require removal of life support, which ensures that organs receive appropriate blood flow and oxygen levels until they are removed for transplantation. In contrast, in cDCDD, withdrawal of life support to enable circulatory arrest and death determination leads to progressive reduction of blood pressure and oxygen levels that contribute to organ injury via ischemia. If this process takes too long, organs can be irreversibly injured and become unsuitable for transplantation. The need to minimize warm ischemic time and the need to ensure the death of the donor before organ recovery commences leads to inevitable tension between these two objectives. [Fig. 1]

Figure 1
Method
Scoping reviews generally aim to map evidence-based literature with a view to examining its extent and range, or to identify existing research gaps.Reference O’Malley and Arksey 11 A scoping review of ethics literature — in which study designs, outcome measures, or intervention types are commonly not germane to findings — calls for some modification to protocol. This scoping review was undertaken according to a schema adapted from the methodological framework of Arksey and O’Malley (2005): 12 (i) identification of the research question(s); (ii) determination and implementation of search strategy; (iii) a two stage screening process for article selection; (iv) a grouping of key concepts, concerns and arguments by theme and summarization of findings.
(i) Identifying and Narrowing the Research Questions
The purpose of this review was broad in scope: to identify all important normative issues, concepts and arguments related to the practice of cDCDD. Preparatory background reading and discussion revealed that a number of these issues derive from conceptual ambiguities and empirical uncertainties that bear on cDCDD. The research was thus refined to comprise three questions:
-
• What are the ethical issues and arguments bearing on cDCDD?
-
• What debated or ambiguous concepts underlie these ethical arguments?
-
• What empirical uncertainties underlie these ethical issues?
(ii) Determining and Implementing Search Strategy
Three bibliographic databases were used in the literature search: PubMed, Embase, and SCOPUS. Search strings were developed through an iterative process that evolved as common or recurring themes, concepts and issues became apparent.[Appendix 1] This iterative process was necessary considering the broad scope of the review. 13 To limit the search results to publications that had bearing on substantive ethical and conceptual issues, it was decided that searches of article titles, keywords, and abstracts would be limited to those that included (i) one of the terms currently or previously used to describe cDCDD and (ii) at least one keyword the authors determined was relevant to the review in light of evolving awareness of key issues.[Appendix 2] Search strings were applied to each database in accordance with their specific format requirements using Boolean operators “AND” and “OR” between and within groupings (i) and (ii). No date limits were applied. The initial search was undertaken May 15, 2019 and repeated December 15, 2019 to identify and include recent publications. A hand search of bibliographies was undertaken after article selection to identify publications that did not appear in the database search but which were deemed relevant to the review.
(iii) Screening
The literature search identified 1,726 citations of possible relevance (PubMed n= 501; Scopus n=514; Embase n=711). After screening for duplicates using EndNote X9 functions (n=796) a total of 930 remained. Inclusion and exclusion criteria were developed post hoc following preparatory background reading. 14 [Appendix 3] Screening for relevance was undertaken in two phases: (a) an initial screening of titles to identify those that were evidently clinical in focus or clearly did not promise to meet inclusion criteria; (b) a review of abstracts for possible inclusion. In order to provide background on existing practice, a sample of consensus statements and/or protocol guidelines was selected even if these did not engage substantively with ethical or conceptual issues (n=8). In phase (b) a total of 106 publications were selected for analysis out of a possible 193 selected during phase (a). A further 61 articles were identified through hand searching of bibliographies of included articles and selected for review because of either reoccurring citation or obvious relevance, bringing the total number of selected publications to 167. [Fig. 2]

Figure 2
(iv) Analysis and Summary
During review of the 167 selected publications key themes corresponding to ethical concerns emerged. These later informed the analytical groupings described in our summary. The themes identified were:
-
1. Interpretations of “irreversibility”
-
2. Death determination
-
3. Dead donor rule
-
4. Potential harms versus benefits to donors
-
5. Conflicts of interest
-
6. Public trust [Fig. 3]
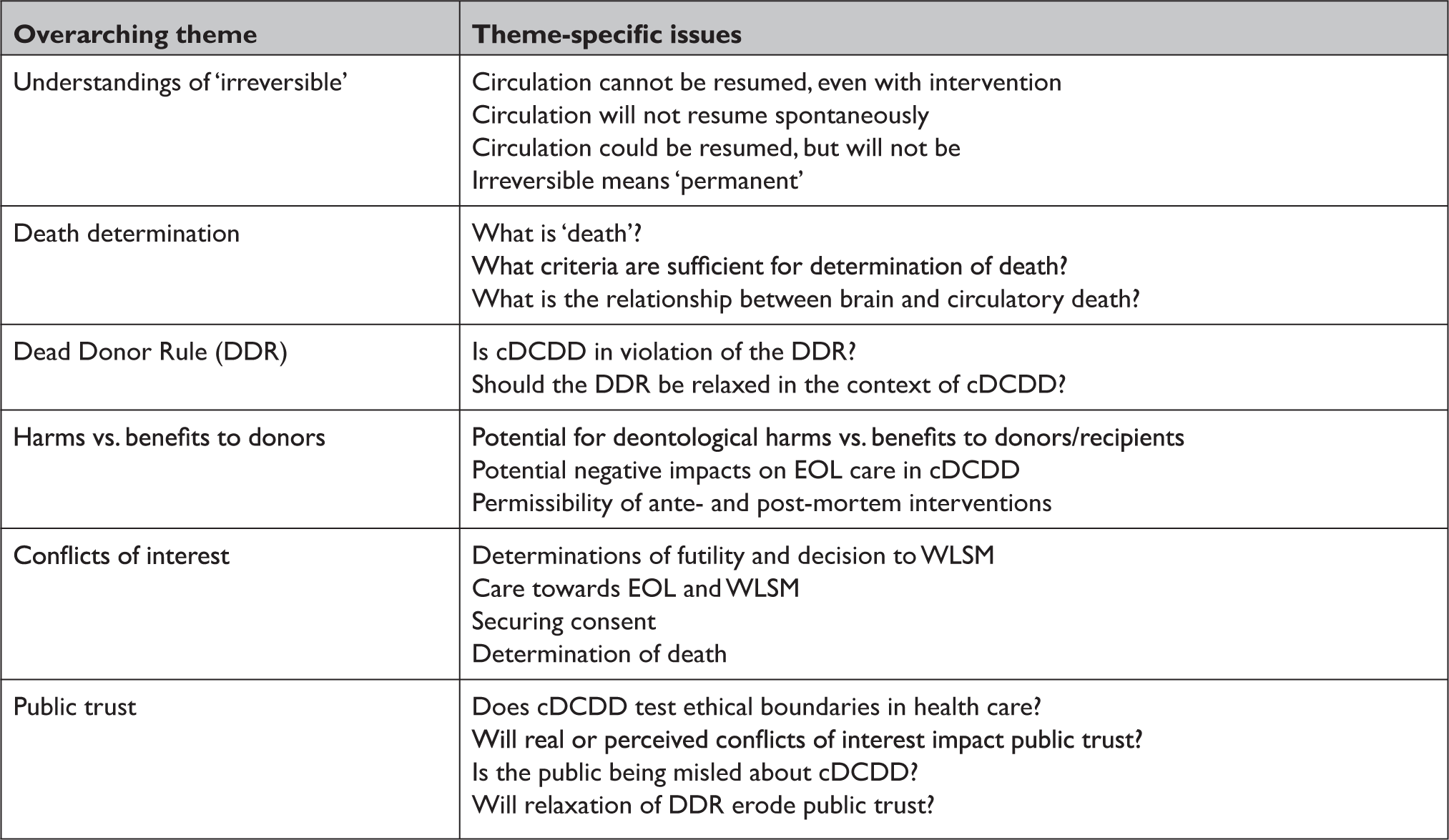
Figure 3
Where there was significant overlap in subject matter it was decided to group arguments, concepts and concerns under the overarching theme considered most relevant. Publications were reviewed, and their substantive comments and arguments recorded under the appropriate theme. In keeping with Arksey and O’Malley’s (2005) methodological approach, we did not attempt to assess the quality of articles reviewed. 15 The information collected was then synthesized into the narrative account below. The flow of our summary of findings reflects an ascending order of more to less foundational concepts and arguments. This bottom-up ordering is reflective of the fact that many of the ethical issues surrounding cDCDD emerge from disagreement on the conceptualization of fundamental terms. Where necessary, key concepts, concerns, and arguments that apply to more than one theme are repeated in the summary to make clear their connection to the overarching theme being discussed.
Results and Discussion
I. Timing of Death: When is Cessation of Circulatory Function “Irreversible”?
The criteria for determination of death in cDCDD require simultaneous and irreversible unresponsiveness, apnea, and absent circulation. 16 As Youngner and Arnold (2001) note, “[i]rreversibility remains an essential, but undefined element in the definition and determination of death.”Reference Youngner and Arnold 17 The problem of how to interpret “irreversible” is widely debated in the cDCDD ethical literature. While one might argue that this is primarily a clinical issue, conceptual interpretations of “irreversible” are relevant to the ethics of cDCDD in light of the dead donor rule (DDR) — the ethical imperative that donors be deceased before organ recovery commences. The question of whether cDCDD is in violation of the DDR is perhaps the overriding ethical concern attending the practice. Yet, as discussed below, the purported ambiguity of the term “irreversible” drives many of the other controversies that arise in discussions of cDCDD. Two main questions concerning the criterion of irreversibility arise, the answer to the second contingent on the answer to the first. First, how should we interpret the term “irreversible”? Second, what length of no-touch time is sufficient to ensure irreversibility? Answers to these questions determine whether cDCDD is thought to be in violation of the DDR.Reference Robertson and Bell 18
There are several ways that “irreversible” can be interpreted. We group these into four non-mutually exclusive views, each with its own justification. Some authors combine two or more of these views in defense of their understanding of irreversibility.
i) Circulation Cannot be Resumed, Even with Intervention
This is the strictest interpretation of “irreversible.” Those who read the term in this way sometimes use it as a premise in an argument that suggests cDCDD often violates the DDR. Perhaps the best exposition of this view comes from Marquis,Reference Marquis 19 but it is voiced by many.Reference Menikoff 20 For these authors, “irreversible” just means “cannot be reversed.” This accords with a metaphysical view of biological death as the unalterable cessation of bodily function. Therefore, on this view, cDCDD may violate the dead donor rule when circulation has not irreversibly stopped at the point of organ recovery. In many instances, it could be resumed with medical intervention. Conceptual concerns stemming from this reading of irreversibility are exacerbated by the increasing use of recovered donor hearts: the restoration of heart function in recipients appears to confound the requirement that circulation cease irreversibly.Reference Veatch and Perspective 21 However, this worry is circumvented by emphasizing cessation of circulation in the donor as opposed to heart function, or by emphasizing the importance of cessation of circulation to the donor’s brain. 22
ii) Circulation Will Not Resume Spontaneously
Advocates of this reading argue that our understanding of “irreversible” should at minimum preclude the possibility of the spontaneous resumption of circulation, referred to as autoresuscitation. This in mind, many argue that the only ethically relevant concern regarding understandings of “irreversible” is whether autoresuscitation is possible after a required no-touch period.Reference Doig and Rocker 23 While suggestions for this period have run as low as 75 seconds,Reference Boucek, Mashburn, Dunn, Frizell, Edwards, Pietra and Campbell 24 most consensus statements endorse a specific no-touch period within the range of 2-5 minutes in order to preclude autoresuscitation. 25 However, some authors have worried that these guidelines are based on insufficient data and therefore we cannot exclude the possibility.Reference Rady, Verheijde, McGregor and Commentary 26 Additionally, some suggest that autoresuscitation may be underreported and thus assessment of its probability is not properly informed.Reference Jolliffe 27 The likelihood of autoresuscitation appears to be an unresolved empirical question.Reference Bernat 28 Previous investigations on the incidence of autoresuscitation in the context of donation have found little evidence that it occurs outside of the context of uncontrolled donation after circulatory determination of death and concomitant attempts at cardio-pulmonary resuscitation.Reference Hornby, Hornby and Shemie 29 That said, skeptics may note that these findings do not prove that autoresuscitation cannot occur beyond the 5 minute benchmark espoused in many jurisdictions. Thus, advocates of this understanding of “irreversible” seek to exclude the possibility of autoresuscitation while continuing to debate the appropriate length of no-touch time. Further empirical study will help to resolve debate surrounding this reading of irreversible.Reference Dhanani, Hornby and van Beinum 30
iii) Circulation Could be Resumed but Will Not Be - Based on a Morally Justified Decision
This understanding of “irreversible” is sometimes called a “decisional” 31 view or an “appeal to a norm.” 32 Under this view, determinations of death should not be divorced from context. If a no-cardiopulmonary resuscitation or “do not resuscitate” order has been signed, and if patients or surrogates have consented to WLSM and donation, then the mere possibility of resuscitation with medical intervention is of little or no moral importance. Restoration of function would be ethically inappropriate. This means that the view is partly, and explicitly, normative. 33 In this sense, “‘irreversible’ […] is best understood not as an ontological or epistemic term, but as an ethical one.”Reference Tomlinson 34 Or, we might add, a legal one. Thus, as Shemie argues, “… the issue is not whether the body or brain circulation and function can be resumed (because it can), but rather, whether it will be.”Reference Shemie 35 The outcome of this view is similar to that of (ii) because it does not necessitate a no-touch period beyond that required to preclude autoresuscitation.
iv) “Irreversible” Just Means “Permanent”
This view is almost indistinguishable from (iii) but merits its own category insofar as its defense sometimes relies on a standard of medical practice.Reference Bernat 36 Advocates of this view hold “permanence” has always been the medical standard for declaration of death in clinical settings. As such, its application in the context of cDCDD is warranted. Like (iii), this reading holds that there is a meaningful distinction between “irreversible” (“cannot be restored”) and “permanent” (“will not be restored”). 37 Since cDCDD donors or their surrogates have determined that resuscitative efforts will not be undertaken, the permanence criterion allows for declaration of death before “irreversibility” in its strictest sense obtains.Reference Ave, Sulmasy and Bernat 38 Since permanence inevitably leads to strict irreversibility, the former is a plausible proxy for the latter. 39
Discussion
The problem with these varied understandings, note Aulisio, Devita, and Luebke, is that the “[s]atisfaction conditions for each of these notions of irreversibility are not co-extensive.” 40 That is, a single set of clinical criteria will not satisfy all interpretations. Nonetheless, the prevailing view in the donation community holds that “permanent” is a reasonable interpretation of “irreversible,” and as such a 5-minute no-touch period is a reasonable safeguard against the possibility of autoresuscitation.Reference Shemie, Hornby and Baker 41 Consensus statements from professional and regulatory bodies endorse these conclusions. 42 That said, the issue of how to interpret “irreversible” is far from resolved in the ethics literature. We contend that disagreement in this domain is explained by metaphysical disagreements about the definition of death and, hence, appropriate criteria for its determination. The crux of the matter is when the term “deceased” can be used to denote a body. As will be seen below, given that there is no consensus on the definition of death, prospects for a universally endorsed resolution to the debate on the interpretation of irreversibility appear dim. However, increasing consensus regarding its interpretation in the medical community suggests that this issue is primarily of concern to bioethicists.
II. Understandings of “Death” and Criteria for its Determination
This theme in the literature underscores how the practice of cDCDD is plagued by ambiguities in the concept of “death,” ambiguities which parallel and inform debates around irreversibility. Unless there is greater clarity on both the definition of death and criteria for its determination, concern will remain that cDCDD violates the DDR.Reference Rodriguez-Arias, Smith and Lazar 43 In this context, there are three areas of disagreement.
(A) How Should “Death” be Understood?
Although this question points to an enormous body of philosophical literature that is beyond the scope of this review, it bears on criteria for determinations of death and thus merits brief discussion. Youngner notes that any understanding of death must have three components: “a concept or definition of what it means to die, operational criteria for determining that death has occurred, and specific medical tests showing whether or not the criteria have been fulfilled.”Reference Youngner 44 Considerable confusion surrounds the conceptual side of this triangle.Reference Youngner, Arnold and DeVita 45 This is problematic, because the criteria for the determination of death will vary according to our conception of death. That is, the architecture of the conceptualization is hierarchical. A given concept suggests certain criteria which entail specific medical tests. Most conceptions of death focus on the loss of the integrative unity of bodily functions rather than the loss of function in its constituent parts. 46 Beyond this, scholars who discuss criteria for determinations of death can be categorized as falling (very generally) into two camps, each of which understands death somewhat differently:
(i) Those who hold that death is strictly an ontological category. This is the “classical”Reference Bell 47 conception of death, sometimes called “biological death.” 48 This understanding corresponds to the common-sense view of death as the unalterable cessation of bodily functions. This view is consonant with a strict interpretation of “irreversible.”
(ii) Those who hold that death is admittedly a distinguishable ontological category, but “nonetheless, philosophy, religion, psychology, politics and even economics play major roles in how individuals and groups interpret the biological facts.” 49 In this way, “death” is both a biological and social phenomenon insofar as factors external to biology have some bearing on what “death” is thought to be, or at least when it can be declared. 50 There are compelling social and cultural reasons for why it can be declared before “biological death” obtains.Reference Huddle, Schwartz, Bailey and Bos 51 This view is consonant with less restrictive interpretations of “irreversible.”
The view of death adopted in a given jurisdiction has important social ramifications. For example, it is important to know when to sign a death certificate, when the rights of a person cease to be, and when to enact the provisions of a will. Yet, because of time constraints inherent in cDCDD, the need for specificity with regard to the concept-dependent criteria for determination of death is acute. Minimizing ischemia time while ensuring accurate death determination is paramount.
Despite disagreement over how death should be conceptualized there is general agreement in the literature that death is a process, not a singular event occurring at a determinable moment in time.Reference Shemie and Gardiner 52 This observation of indeterminacy features in arguments which conclude that determinations of death, proclaimed at a point in time, have always been discretionary. 53 If determinations of death have always been the result of social consensus, it seems that no amount of scientific evidence will resolve the debates:
For all medical diagnoses except death, we believe that greater scientific knowledge will bring increasing clarity about how to make the diagnoses with ever higher levels of precision. In the case of death, however, our uncertainty is not related to the state of our scientific knowledge, but rather to different and incompatible understandings about the meaning of death.Reference Truog and Robinson 54
Since unequivocal criteria for determinations of biological death are difficult to apply in the time-sensitive cDCDD context, some argue that we should be satisfied with social consensus and clinical practice standards for determining death.Reference Bernat 55 With that said, the various “incompatible understandings of the meaning of death” employed in the context of organ donation raise worries that “death” — long thought to be a strictly ontological category — has been manipulated for utilitarian reasons with a view to increasing the organ donor pool.Reference Arnold and Youngner 56
(B) What Criteria are Sufficient for Determinations of Death in cDCDD?
Answering this question requires that one first decide how we should understand “death.” Given disagreement on how to define death in this context, it is no surprise that there is also disagreement on how criteria for determinations of death in cDCDD should be constructed. It is at the level of criteria that most debates around death occur.Reference Dubois 57 Here again the controversy surrounding the legitimacy of circulatory criteria for determination of death centers around the above-mentioned “irreversibility” debate and its attendant problems (sec. I). While there are strict (though somewhat variable) criteria for brain death, inconstancy in cDCDD protocols suggests that there is no comparable consensus on interpretations of the criteria for circulatory death.Reference DeVita 58
The main concern over the determination of death based on circulatory criteria is that the required no-touch period may be insufficient to ensure “death” or irreversibility. As noted (sec. I), many authors worry that the 2-5 minute wait period is arbitrary or based on insufficient data. 59 For some, this means that circulatory death criteria do not actually describe death.Reference Truog and Halpern 60 While others argue that somewhere within 2-5 minutes is sufficient, 61 the (remote) possibility of autoresuscitation, as well as the potential for resuscitation with medical intervention, suggests that these authors are operating with a different conception of death (clinical death relying on “permanence”) than those who worry that the no-touch period is insufficient (biological death relying on a strict interpretation of “irreversible”).
In some jurisdictions, another concern relating to circulatory death criteria is that “[t]he post-mortem use of [normothermic regional perfusion] may retroactively invalidate the preceding death declaration by negating the necessary condition of permanent cessation of circulation.” 62 In other words, the use of medical technologies such as normothermic regional perfusion can retroactively negate the justification for the determination of death by restoring circulation to the body. 63 Of perhaps greater concern is the risk of reperfusion to the brain and the consequent possibility of reanimation. 64 In this way, the introduction of new technologies can confound death determination. 65 Given these issues, there are three options: admit that criteria for circulatory death are flawed and revise them to accommodate objections; relax or abandon the DDR so as to avoid these objections; or circumscribe the use of normothermic regional perfusion in this context. As discussed below, given an apparent reluctance to abandon established criteria for death and the arguably inviolate tenets of the DDR, the permissibility of normothermic regional perfusion is a controversial issue in cDCDD.
(C) What is the Relationship Between Circulatory Death and Brain Death?
The relationship between the two established standards for declaration of death — neurological criteria and circulatory criteria — is unclear. While some argue that the two corresponding sets of criteria point to a co-extensive concept of death, this conclusion is not obvious. According to Youngner, Arnold, and DeVita, 66 there are two ways that the relationship between circulatory and brain death can be understood:
i) Circulatory and brain functions are jointly necessary and interdependent; each is equally essential for life, so the loss of just one will mean the loss of life. There are simply two ways to establish the same phenomenon: death. Death is the loss of integrated functioning of bodily systems. The loss of either brain or circulatory function therefore leads to death. 67
ii) Circulatory death is a proxy for brain death, which is what really matters. Circulatory death is just the usual way of determining brain death.Reference Menikoff 68 Since the brain cannot survive without circulation, it is reasonable to assume that circulatory death leads rapidly to brain death.Reference Bernat, Capron, Bleck, Blosser, Bratton, Childress and DeVita 69 The necessary and sufficient condition for life is brain function.
Both of these views lead to conceptual and ethical worries. Opponents of (i) argue that the two established sets of criteria for determining death point to different kinds of death, something that should not be possible for a univocal phenomenon. 70 While expert bodies and the oft-cited American Uniform Declaration of Death Act maintain that the criteria point to the same phenomenon, many are not convinced that they do. For example, a minority of critics hold that “brain death is incoherent in that it fails to correspond to any biological or philosophical understanding of death.” 71 This is because the body often retains some integrative unity after brain death, albeit with mechanical intervention.Reference Shewmon 72 More germane to cDCDD, the brain may retain some function after circulatory death for an unknown period of time. 73 Perhaps more to the point, cessation of brain function following circulatory arrest may not be irreversible. 74
There is growing consensus that (ii) is correct.Reference Manara 75 As Dalle Ave and Bernat argue, “[t]hrough the pathway of circulatory cessation, the fundamental criterion of death is also the brain criterion.” 76 Cessation of circulation is thus a proxy for brain death. This raises problems on two fronts. First, since the temporal relationship between cessation of circulation and brain death is uncertain,Reference Rady, Verheijde and McGregor 77 some scholars worry that circulatory death criteria do not, in fact, ensure brain death in the context of cDCDD (at least not within the 2-5 minute no-touch period). 78 If circulatory death is a proxy for brain death, and if brain death is what really matters, then a donor is not known to be dead at the point of organ recovery without confirming brain death, and nor is it certain that brain function has been irreversibly lost. Second, with the growing use of thoracic normothermic regional perfusion in some jurisdictions, fears that reperfusion of the brain could reanimate the donor and negate the justification for determination of death threaten to render impracticable the use of circulatory criteria as a proxy for brain death.Reference Dejohn and Zwischenberger 79 These observations lead to suggestions that both sets of criteria need to be met in declarations of death in cDCDD. 80
Discussion
There is some agreement in the literature that understandings of death are justifiably based on biology, culture, medical practice, and social norms, and therefore criteria for its determination are not restrictively tied to the ontological category of death. This observation helps to explain the consensus that has emerged around the interpretation of “irreversible” as “permanent.” Yet it also demonstrates how incompatible understandings of death may result in morally and metaphysically defensible yet contrary viewpoints concerning when exactly death can be declared. For this reason, disagreements about definitions of death are likely to remain unresolved. Because of the hierarchical relationship between concepts and criteria, universal consensus on interpretation of the criteria for determinations of death is similarly, and consequently, unlikely. However, the physiological (and temporal) relationship between circulatory death and brain death can be clarified with further empirical research. This may go some way towards illuminating socio-cultural understandings of when it is justifiable to declare death. We contend that much of the disagreement surrounding cDCDD is at root a debate about the definition of death. This has implications for the question of whether cDCDD can be said to violate the DDR.
There is some agreement in the literature that understandings of death are justifiably based on biology, culture, medical practice, and social norms, and therefore criteria for its determination are not restrictively tied to the ontological category of death. This observation helps to explain the consensus that has emerged around the interpretation of “irreversible” as “permanent.”
III. The Dead Donor Rule (DDR) and cDCDD
At minimum, the DDR holds that (a) no patient should be killed by organ recovery and (b) patients must be dead before organs are recovered. 81 This is consistent with the injunction that physicians do no harm to their patients. Although most authors do not discuss the foundations of the DDR explicitly, there are several that can be identified in the literature.
Most agree that the primary reason for the DDR is to protect patients from harm and exploitation.Reference Gardiner and Sparrow 82 This motivation is therefore deontological: using patients as a mere means would demonstrate disrespect for persons. As Robertson states, “[t]he dead donor rule is a centerpiece of the social order’s commitment to respect for persons and human life.” 83 Other authors add that there is also a consequentialist motivation for the DDR insofar as it protects physicians from criminal charges and preserves public trust in organ donation schemes and physicians.Reference Miller, Truog and Brock 84 Although different motivations are emphasized by different authors, it is arguable that respect for persons is the fundamental principle underlying the DDR. However, disagreements discussed in the foregoing sections opens the door to debates concerning whether cDCDD sometimes violates the DDR. Given controversies over interpretations of “irreversible,” criteria for determination of death, as well as debates on the need for the DDR in light of evolving societal norms, two important questions arise regarding the DDR and its bearing on cDCDD.
(A) Is cDCDD in Violation of the DDR?
This question highlights how the debates discussed thus far are not disparate themes; they are ineluctably intertwined. Whether or not the DDR is thought to be violated in cDCDD depends on one’s positions with respect to understandings of “death” and the interpretation of “irreversibility.” As Truog and Robinson argue, the DDR “depends on a coherent definition of death, yet this definition has proven elusive.” 85
A vocal minority of authors assert that the DDR is violated in cDCDD.Reference Miller and Truog 86 The main reason for this worry stems from the way that death is declared. This is because, once again, it is not clear that a 2-5 minute no-touch period is sufficient to preclude the possibility of auto-resuscitation, and, second, it is not certain that donors meet the irreversibility criterion at the time that organs are recovered (when interpreted in the strict sense of cannot be reversed) (see sec. I). If donors are not certainly dead, it is arguable that organ recovery is sometimes the cause of death. 87 Similarly, if one holds that criteria for circulatory determination of death do not actually describe death, then the DDR is potentially violated in cDCDD. 88 For example, uncertainties regarding the physiological and temporal relationship between circulatory cessation and cessation of brain activity casts doubt on the vital state of donors, at least for those who worry that the bifurcation between brain and circulatory death is confused. 89 Furthermore, when thoracic normothermic regional perfusion is used in cDCDD protocols, the possibility of restoration of circulation to the brain means that criteria used to determine death could be invalidated. 90 Therefore, patients cannot reliably be declared dead. If they are not dead, then the DDR is violated during recovery. If this is so, since the DDR is inviolable, cDCDD is unethical.
(B) Should the DDR be Relaxed or Abandoned?
It is important to note that while most authors consider any violation of the DDR unethical, others suggest that violation of the DDR is not inherently so, and may be justifiable given informed consent. 91 Intractable debates concerning the DDR in this context have led some to propose that it should be relaxed or abandoned altogether. Critics argue that blind adherence to the DDR has led to insupportable revisions to the concept of death and that we must face the fact that, since medical practice may already violate the DDR, it could be time to do away with it in circumscribed areas. 92 Adherence to the DDR obscures what is really at issue: how can we maintain respect for persons while respecting the wishes of patients to donate? 93 Or, for those who contend that cDCDD donors are not dead, when is it permissible to retrieve organs from the dying? 94 Some suggest that the DDR can — and should — be supplanted by other ethical principles that could govern cDCDD, such as non-maleficence and respect for autonomy. 95 After all, they argue, denial of a patient’s desire to donate based on an arbitrary rule amounts to an act of disrespect. Waiting until donors are dead may impact the chances of organ graft, and surely a patient desiring to donate would prefer not only to preserve the donation opportunity, but also to bequeath organs that have suffered minimal ischemic damage.Reference Halpern and Truog 96
Defenders of the DDR muster consequentialist arguments in its support. These authors worry that cDCDD without the DDR would: erode public trust in organ donation schemes and physicians;Reference Lyon 97 distort the therapeutic doctor-patient relationship;Reference Potts and Evans 98 cause dignitary harms to donors; 99 lead to a slippery slope whereby patients are routinely killed for organs;Reference Burdick 100 or erode widely endorsed societal values. 101
Discussion
Ultimately, universal consensus on whether the DDR is respected in cDCDD is lacking, though the widespread practice of cDCDD suggests that this is not a reflection of the views of the donation and transplant community. Those who argue that the DDR is not violated generally rely on the permanence criterion for irreversibility. Those who argue that it is violated generally interpret the irreversibility criterion strictly. This lack of consensus is once again best explained by the reasonable moral and metaphysical disagreement concerning death and criteria for its determination. However, the debate concerning the relaxation of the DDR is less fractured. Despite occasional calls for doing away with the DDR in the context of cDCDD, it seems that most authors are not ready to countenance this option. Ultimately, “[…]the symbolic costs of relaxing the dead donor rule appear to be too great to be tolerated.”Reference Bernat 102
IV. Tensions Between Potential Harms and the Benefits of cDCDD
Discussion of the DDR draws attention to the potential harms to which, some argue, donors are susceptible in cDCDD. Since the principle of non-maleficence guides medical practice, the possibility of harm needs attention when assessing the ethical propriety of cDCDD. In this context, the root issue concerning purported harm to donors is to what extent donor care can or should be altered in the interest of promoting both donors’ autonomous wishes to donate and the interests of organ recipients. In this area there are three main areas of concern. Since cDCDD protocols vary widely, not all of these concerns apply to every form.
(A) The Potential for Deontological Harms to Donors vs. Promotion of Autonomous Wishes
To cause a deontological harm is to fail to treat a person with the respect they deserve, whether or not that person perceives it. The deontological foundation of the DDR leads some to argue that the DDR is not just a prohibition against killing. It has two components: “a prohibition on killing and a prohibition on using living patients solely as a means to an end.” 103 The latter injunction expands the purview of the DDR to include issues that arise prior to a donor’s death.
A minority of authors suggest that the practice of cDCDD could express disrespect for persons. The worry is that patients may be instrumentalized or considered as a mere means to an end — organ procurement.Reference Simon, Schears, Padela and Goldstein 104 To treat someone as a mere means rather than an end is to cause them a deontological harm through instrumentalization. The use of antemortem interventions and the prolongation of life sustaining measures during workup and until such time as an organ recovery team has been readied is presented as putative evidence that patients are instrumentalized. The overarching concern is that practices that are not in the medical interest of the donor suggest that the patient is being treated as a mere means to organ procurement.Reference Bastami, Krones and Biller-Andorno 105 Seen this way, note Gardiner and Sparrow, “the DDR is breached whenever procedures to harvest vital organs are initiated while the patient is still alive.”Reference Cooper 106 This arguably results in a loss of dignity in the dying process.
Despite this concern, many respond to the above worries by noting that the deontological basis of the DDR does not require that donors can never be used as a means, but rather that they never be used solely as a means. Since respect for human dignity and autonomy underlie the deontological aspect of the DDR, if a patient has an expressed wish to donate then antemortem interventions and the prolongation of life sustaining therapies serve in reality to promote the interests of donors: “[t]o fulfill someone’s wishes, and most especially those pertaining to personal core values, is to properly give respect to that individual’s (prior) autonomy.”Reference Price and Samanta 107 Supporters of cDCDD argue that dissenters mischaracterize the attitudes of clinicians and interpret “best interests” too narrowly. 108 In fact, they argue, to deny the opportunity to donate is to deny concrete benefits to donors. 109 This response echoes debates concerning the DDR. While it may not be in the donor’s best medical interest to be subject to antemortem interventions and prolongation of life-sustaining measures, “[s]uch acts may be justified through their promotion of the donor’s legitimate interests in what becomes of their bodies after death.” 110 Donors have concrete interests in the success of transplant and may wish to leave a legacy. Benefits to donors, their families and recipients should not be discounted. To deny an autonomous wish to donate on the grounds that it causes a dignitary harm is, paradoxically, to deny that the donor has the dignity that attends personal autonomy.
While the foregoing argument has many proponents, doubt remains over whether donors’ autonomous interest in donation really can justify antemortem interventions which were never anticipated by the donor. A prominent source of worry is how prior consent to organ donation may not entail consent to the interventions associated with cDCDD. The public’s lack of awareness of cDCDD protocol, and the lack of detailed information relayed through generic donation consent processes, suggests that potential donors are not always fully informed about what they are consenting to. 111 Donors may object to procedures that have the potential to instrumentalize them or cause psychological distress to their loved ones. As Gardiner and Sparrow note, “there is a certain amount of intellectual strain involved in thinking of premortem interventions in the care of a patient designed to facilitate [cDCDD] as motivated by a concern for the best interests of the donor.” 112 While antemortem interventions may promote an autonomous wish to donate organs, critics worry that this may come at the cost of causing deontological harm. This stimulates proposals for specific informed surrogate consent to each antemortem procedure employed in a given cDCDD protocol.Reference Ave and Shaw 113
(B) The Possible Negative Impacts on Care Towards End of Life in cDCDD vs. the Option of cDCDD as a Component of High-Quality End of Life Care
While cDCDD may not cause deontological harms, there is a distinct concern that, since care towards end of life in some jurisdictions proceeds differently in cDCDD than it does in non-donation scenarios, cDCDD protocols may worsen the experience for donors, if they retain conscious awareness, or their families. 114 Differences in care may include the performance of antemortem investigations and interventions intended to improve organ graft and function, 115 the necessity of withdrawing life sustaining measures in the operating room, 116 or the prolongation of these measures during donor workup. 117 Some critics describe cDCDD as “an antithesis of quality end-of-life care, when health care teams await at the bedside for death and then rapidly procure organs in a race against ischemic time.” 118 For others, cDCDD is “a stage-managed affair, lacking in all human dignity.” 119 There is, then, a real concern in some quarters that donor and family experience towards end of life in cDCDD may be negatively impacted.Reference Fox 120
cDCDD, say some, risks a deterioration in care prior to withdrawal of life-sustaining measures (WLSM). 121 In addition to the view that the use of some antemortem interventions could conceivably cause physical harm to donors (see below), a minority of authors have speculated that care may suffer if health care providers consider a patient primarily as a means to donation. 122 More notably, there remains a distinct worry that physicians may be reluctant to provide sufficient comfort care after WLSM to avoid accusations of violating the DDR.Reference Bell 123 Furthermore, since time pressures are inherent in cDCDD, there is speculation that the manner of WLSM — which may be chosen to expedite death — can cause greater discomfort than in non-cDCDD (e.g., rapid extubation). 124
The view that cDCDD risks a deterioration in end of life care is counterbalanced by the widespread sentiment that the option of organ donation is an important component of high-quality end-of-life care.Reference Solomon 125 The prevailing view is that cDCDD protocols do not result in a deterioration in care prior to and after WLSM. Indeed, most established guidelines emphasize that care should be altered as little as possible when facilitating organ donation. 126
In addition to discussion of potential harms to donors, some authors note that cDCDD protocols may harm families insofar as their experience of the dying process could be negatively impacted. 127 Of particular concern are those cDCDD protocols which require death in the operating room, where families are separated from dying donors. 128 This is arguably not a component of high-quality end-of-life care. While some respond by asking why death in the intensive care unit is any better, 129 separation of families from loved ones may cause unavoidable distress. The fact that donors are sometimes returned to the intensive care unit if death does not occur in the proscribed time frame (usually 60-120 minutes) means that an already traumatic experience for families could be exacerbated. Predicting time to death is very difficult, and there is evidence that unsuccessful donation can harm families.Reference Taylor, Buffington, Scalea, Fost, Croes, Mezrich and Schwarze 130 At the root of many worries surrounding care in cDCDD is the fact that families sometimes do not understand the (emotionally painful) trade-offs required for cDCDD.Reference Bernat and Robbins 131
In general, responses to concerns about the potential deterioration of care towards end-of-life and harms to families in cDCDD contend that these worries are overblown, out of touch with the realities of clinical practice, or even cavalier towards the wishes of both donors and families. Families and donors often derive comfort from the knowledge that a death was given meaning through organ donation. 132 In this sense, organ donation is an important aspect of end-of-life care for many. Furthermore, denying a patient’s expressed wish to donate on the basis of worries like the above can be described as paternalistic.Reference Murphy, Manara, Bell and Smith 133 As Gardiner and Riley concede, “[t]o watch as a wish to donate goes unfulfilled is a strong argument against all [of these] concerns.” 134 Given appropriate training, resources and guiding moral principles, end of life in cDCDD can be just as dignified as in non-donation scenarios. 135 One way to overcome the above worries is to ensure that end of life in cDCDD adheres as closely as possible to a standard end of life protocol, 136 and that palliation proceeds as it would in any other case. 137 This imperative is widely accepted and endorsed in the donation and transplant community. Quality of care, it is thought, should not be affected by the exigencies of cDCDD.Reference Mandell and Hendrickse 138
(C) The Ethical Permissibility of Antemortem and Postmortem Interventions
The most prominent debate surrounding the potential for harms in cDCDD concerns the ethical permissibility of antemortem and postmortem interventions designed to improve organ graft and function in recipients. The ethical literature is split on the question of whether antemortem interventions should be allowed, especially antemortem cannulation in anticipation of post-mortem normothermic regional perfusion. 139 There is no consensus in the broader literature, 140 although consensus statements from expert panels in a number of jurisdictions endorse some or all of these procedures. 141 Many consider postmortem mechanical reperfusion to be impermissible because of the danger of brain reperfusion and the consequent potential for reanimation, but again, there is at present no consensus. 142
Those who argue that we should be wary of antemortem interventions muster three main arguments. First, (i), these interventions provide no medical benefit to donors and can be highly invasive; thus, they are arguably not in the patient’s best interest. 143 This concern is exacerbated by the fact that consent to organ donation may not entail informed consent to invasive antemortem interventions. 144 Second, (ii), certain invasive interventions can conceivably cause physical (and deontological) harm to donors. 145 Since these practices arguably transgress the principle of non-maleficence, vocal critics argue that “[p]rocedures that can only cause harm to a patient without providing any benefit are unethical and the person performing them is no longer practicing medicine.” 146 Third, (iii), some worry that antemortem interventions (such as the use of heparin) can actually hasten death, which, if true, can evidently be construed as a harm.Reference Rady, Verheijde and McGregor 147
In response, those who advocate for the permissibility of antemortem interventions argue correspondingly that (i) we can construe best interests broadly such that antemortem interventions are, in fact, of benefit to donors insofar as they serve to promote their autonomous decision to donate organs.Reference Zeiler, Furberg, Tufveson and Welin 148 (ii) Building on the response to (i), while it is possible that these interventions can cause harm, there is in fact little evidence that they do. 149 Furthermore, informed consent and the doctrine of double-effect can justify their use, 150 though the applicability of this latter doctrine is highly contested. 151 Finally, (iii) the possibility that antemortem interventions can hasten death is remote, and thus not of great concern. 152
Some authors regard postmortem mechanical reperfusion to be impermissible. The main concern with reperfusion is that it risks restoring brain function. 153 The use of aortic occlusion balloons or clamps on the aorta and great vessels arising from the aortic arch to restrict blood flow to the brain promises to minimize chances of such occurrences,Reference Perez-Villares, Rubio, Del Rio and Minambres 154 yet some argue that it does so at the risk of conceptually undermining the justification for the determination of death. That is, employing aortic clamps or occlusion balloons “demonstrates that the loss of all brain functions in these protocols cannot be considered irreversible, and that permanent loss is not a valid surrogate for irreversible loss.” 155 Further empirical research can help to establish the risks associated with this practice, though its conceptual ramifications will continue to be debated.
Discussion
Inherent in cDCDD protocols are several important objectives: care for a dying donor and the promotion of their interest in donation on one hand, and the recovery of viable organs for transplantation into a waiting recipient on the other. Sometimes these objectives are thought to be at odds. More often, they are thought to converge.Reference Lesieur, Genteuil and Leloup 156 Greater clarity on the risks associated with antemortem interventions will inform debates on their ethical permissibility. That said, the tension inherent in this debate raises an important ethical question: when is it permissible to alter care for the donor in the interests of donation? Or, how can interventions that are not in the best medical interests of a dying patient be undertaken in an ethical way? Conflicting views on these issues betray deeper disagreements about the legitimate scope of medical practice and the interpretation of the moral principles which guide it. While some argue that potentially harmful interventions should be prohibited, others plausibly respond that their prohibition would unjustifiably encroach on individuals’ autonomous interests in seeing their organs successfully transplanted. Since these are value-laden assessments, moral debate is likely to continue.
V. Potential Conflicts of Interest in cDCDD
The tension between the duty of care to the donor and the desire to procure viable organs for waiting recipients is at the root of putative conflicts of interest that some argue can arise in cDCDD. Conflicts of interest, both personal and institutional, are a pressing issue in cDCDD in part because “[t]he ambit of interests extends beyond the donor, to the donor’s family, the recipient, transplant professionals, institutions, and society generally; and they involve issues such as priority setting, resource allocation, and so on.”Reference Daar 157 Real or perceived conflicts of interest in cDCDD could result in unethical practices or an erosion of public trust in organ donation schemes. The need to identify and address conflicts of interest is widely discussed in the literature on cDCDD. There is widespread agreement that conflicts of interest could arise in cDCDD, but whether these conflicts of interest do arise, or whether they undermine the practice, continues to be debated.
Conflicts of interest can arise at both the personal and institutional level.Reference Frader 158 Personal conflicts of interest involve decision-making at the level of the bedside; institutional conflicts of interest may impact wider policies and protocols. 159 It is argued that conflicts of interest can arise at every step of the cDCDD process.Reference Devictor 160 We list these concerns below before considering generic responses and mitigation strategies.
(A) Determinations of Futility and WLSM
With respect to identifying candidates for donation, notes Doig, “there is an inherent conflict of interest for physicians caring for these and other individuals in the ICU who might also be candidates for [cDCDD]: attempts to preserve the life of a patient might limit or preclude these same individuals from being organ donors.”Reference Doig 161 Some worry that early or erroneous determinations of treatment futility could occur if health care providers are (consciously or unconsciously) motivated by the desire to procure organs from critically ill patients. 162 While others respond that the risk of premature or biased determinations of futility can be overcome with robust guidelines that are already largely in place, 163 detractors point out that determinations of futility are never certain, and that unconscious bias is possible.Reference Overby, Weinstein and Fiester 164 Furthermore, in the unlikely event of physicians seeking primarily to secure organs to reduce shortages rather than ensuring the best possible care for patients, it is conceivable that not all treatments options will be explored prior to determinations of futility or WLSM. 165
(B) Care Towards End of life and WLSM
As noted above (sec. IV), a minority of authors worry that care towards end of life may suffer if patients are considered mere means to organ donation. As Rady, Verheijde, and McGregor argue, “the care of the dying patient [may be] guided by a team whose primary interest is the preservation of organs until procurement has been accomplished.” 166 This could affect the type and quality of care towards end of life. 167 The use of antemortem interventions (with the goal of improved organ graft and function) that are not in the patient’s best medical interest (and may also expedite death) raise worries that care towards end of life may be compromised by conflicts of interest. 168 For instance, say some, antemortem interventions are in the interest of recipients, not the medical interests of dying patients. For those who take this narrow view of “best interests,” this tension epitomizes the conflicts of interest attendant on cDCDD. Additionally, some argue that the timing, location and manner of WLSM may be affected by conflicts of interest in cDCDD, thus undermining the quality of end of life care. 169 In the past, variability in end of life ICU practice raised worries that conflicts of interest were of more than theoretical concern. 170 Standardized protocol and emerging consensus surrounding guidelines seem to have alleviated these apprehensions.
(C) Securing Consent
There is wide variation in procedures for consent among organ donation organizations, transplant centers, and hospitals.Reference Hardart, Labriola, Prager and Morris 171 Some critics worry that “[t]he conflict of interest and self-serving bias of [organ procurement organizations] can limit the exchange of information with surrogates and violate the standards for true informed consent.” 172 Likelihood of consent may be higher when both the putative trade-offs in end of life care and the nature of antemortem interventions required for cDCDD are not fully understood by donors or surrogates, and this may be one motivation for a lack of transparency. 173 As noted above, some authors emphasize that, given the public’s limited understanding of cDCDD, prior consent to organ donation does not entail consent to antemortem interventions. 174 Donors and surrogates may not be fully informed of the putative risks of these interventions when consenting to donation. 175 In addition, there are legal concerns in some jurisdictions surrounding the legitimacy of surrogate decision-makers consenting to antemortem interventions. 176 Furthermore, it is likely that surrogates and donors are not aware of the controversies surrounding determinations of death, the possibility of reanimation through reperfusion, and the practice of cDCDD more generally while consenting to donation. 177 Again, this may violate the requirements for valid informed consent.
(D) Determination of Death
Although conflicts of interest in the determination of death are rarely explicitly spelled out in the literature, it is reasonable to assume that they can occur given the time pressures that are inherent in cDCDD. 178 For example, from an institutional perspective it is expedient to adopt a weak construal of irreversibility and a shorter no-touch period in the interest of recovering viable organs. Institutions may be motivated by utilitarian rationales to adopt perspectives on these debates that are amenable to their organ procurement goals.
Discussion
Despite the many potential conflicts of interest in cDCDD, the vast majority of authors argue that these can be mitigated or eliminated. 179 Indeed, this is one area where there seems to be uncharacteristically strong consensus. The primary objective of clinical medicine is the care of patients. As such, the mitigation of conflicts that may undermine this objective is of paramount importance. This will help to ensure that medical practice does not stray beyond its morally sacrosanct boundaries.
Conflict of interest mitigation strategies are noted in all reviewed consensus statements on cDCDD. 180 The most commonly proposed is the separation of care and organ recovery teams. Since unseparated teams may be influenced by conflicts of interest, those that care for dying patients and those that secure consent or recover organs for transplantation must be strictly separated. Separation of teams will address both real and perceived conflicts of interest in cDCDD. 181 Guidelines emphasize that decisions regarding withdrawal of life sustaining measures must precede any discussion of organ donation. In addition, clear protocols for cDCDD will lessen the chances of conflicted decision-making. 182 Potential conflicts of interest should be disclosed in order that surrogates can make informed decisions on donation. 183 Finally, fully informed consent requires transparency. Surrogates must consent to each aspect of cDCDD: withdrawal of life sustaining measures, donation, and antemortem interventions. 184
A few dissenters take issue with the view that a mandated separation of teams will effectively eliminate all conflicts of interest. While possible in theory, they argue, such separation is difficult in practice. 185 These objections notwithstanding, the prevailing view is that conflicts of interest are manageable.
VI. cDCDD and the Preservation of Public Trust
Public trust in physicians is essential for the practice of medicine. Trust is especially important in the context of organ donation and cDCDD. Patients and their surrogates need to be confident that physicians will always put patient interests first, that donors will not be killed for their organs, and that cDCDD rests on firm empirical and ethical foundations.Reference Bernat 186 This is in the interest of donors, recipients, families, health care providers, and the public. Preserving public trust in organ donation schemes is also essential to promoting recruitment in these schemes. As Gallagher, Skaro, and Abecassis argue, “[u]ltimately, defining what is ethically acceptable must be balanced with maintaining the public trust, which is sacrosanct in the field of transplantation.”Reference Gallagher, Skaro and Abecassis 187 Some have argued that the practice of cDCDD might inflame public anxieties about medicine insofar as it tests societal boundaries of ethically acceptable practices in health care to such a degree that it could erode trust in both physicians and organ donation schemes. 188 This is why some consider public trust to be the “major issue” in cDCDD. 189 We outline these concerns before considering responses.
In this context, many worries relating to public trust arise. It is arguable that all of the controversies surrounding cDCDD raised in the foregoing could undermine public trust. Indeed, many arguments have the following form: “the concern we have raised regarding X is worrisome; disclosure of the uncertainty and debate around X will thus erode public trust.” These arguments involve speculation on empirical consequences that may obtain in the future. Since the suggested consequences are empirical in nature, disagreement in this area could be informed by further study of public attitudes towards the various aspects of cDCDD.
(A) Does the Practice of cDCDD Test (or Transgress) Society’s Ethical Boundaries?
Answers to this question draw on more focused debates in the literature on cDCDD. The question’s answer is contingent on one’s position with respect to these narrower debates, as well as one’s views on how the ethical principles guiding medical practice should be interpreted. Most arguments concluding “yes” take the following form: “concern X is a problem; X means that we are transgressing ethical principle Y; once made aware of X, the public will lose trust in physicians and organ donation schemes because it espouses Y.” As such, a few examples will suffice.
If one thinks that the risk of hastening death by way of antemortem interventions is non-negligible, one might contend that doctors are sometimes killing patients — something that could stoke public fears of patients being killed for organs. 190 Killing patients distorts the nature of the doctor-patient relationship and thus runs the risk of eroding public trust. 191 A similar argument can be made if one thinks that cDCDD donors are not actually dead when organs are retrieved. The public may react negatively if it believed that organs were being taken from the living, for doing so would represent a violation of the DDR. Similarly, suggestions that “irreversible” loss of brain function could be restored after circulatory determination of death could lead to “public uncertainty and the possibility … of derailing the transplant programme in general.” 192 Finally, if one contends that cDCDD causes deontological harms to donors 193 then public trust could be impacted insofar as the practice may be perceived to undermine society’s commitment to the inherent worth of all persons.
(B) Will Real or Perceived Conflicts of Interest Erode Public Trust?
Some authors suggest that public perception of conflicted decision-making at any stage of cDCDD would erode trust in organ donation schemes and physicians. Here again the arguments take a similar form: “because of the conflict of interest we have identified, public trust may be eroded.” For example, “[…a]ny doubt over decisions to withdraw life-sustaining treatment would be a potential disaster for any [DCDD] programme.” 194
Responses to these concerns piggy-back on those that respond to the worry that conflicts of interest jeopardize the ethical permissibility of cDCDD. First, perceptions of impropriety will be alleviated by separation of teams. 195 Second, clear protocols for cDCDD will mitigate the chances of conflicted decision-making. 196 Finally, all potential conflicts of interest must be transparently voiced to promote confidence in the medical profession. 197
(C) Is the Public Being Deceived When it Comes to cDCDD?
A minority of critical authors worry that the public is being misled about the practice of cDCDD. There is a concern that a weakening of public trust may result from wider awareness of this purported deception. This debate focuses on the contentious criteria for determination of death employed in cDCDD. Death, say some, is a concept that is being gerrymandered in order to increase the pool of eligible organ donors. 198 Physicians, institutions and organ procurement organizations are practicing “deception” when it comes to cDCDD: donors are not dead. 199 Falsely claiming that sound science underlies criteria for determination of death is dishonest. 200 The arguably misleading language used to describe the vital states of cDCDD donors leads the public to falsely believe that donation only ever takes place after death has been unequivocally determined. 201
(D) Will the Proposed Relaxation of the DDR Erode Public Trust?
Perhaps the most prominent debate surrounding public trust concerns the possible impacts resulting from something that has not even happened: the relaxation of the DDR. This debate is stimulated by proposals to abandon the DDR in order to facilitate cDCDD and avoid conceptual turmoil. 202 As previously noted, these proposals stem from the belief that the DDR is already violated, 203 that blind allegiance to the rule obscures what is really at issue, 204 and that this allegiance requires indefensible revisions of the concept of death. 205 Despite these arguments, the vast majority of authors suggest that relaxing DDR will lead to an erosion of public trust in cDCDD. 206 Maintaining the DDR is essential to reassure the public of the primacy of patient interests. 207 Proponents of jettisoning the rule argue that such slippery-slope rejoinders are not based on any firm evidence; in fact, available evidence suggests that the public will not be unduly concerned with a loosening of the DDR.Reference Halpern 208 Yet despite proposals for relaxing the DDR, 209 the prevailing view is that it should not be abandoned.
Discussion
Given the concerns regarding the possible impact of cDCDD practice on public trust, there is consensus that full transparency and consultation with the public are essential for determining the ethical appropriateness of the various elements of cDCDD protocol.Reference Ball, Parsons-Leigh and Sibbald 210 All controversies in the literature must be presented to the public. As Vincent and Brimioulle argue, “[w]ith the sensitive nature of all organ donations, [DCDD] must be considered and discussed openly and honestly to avert raising unnecessary concern or suspicion among the public.”Reference Vincent and Brimioulle 211 Feedback from the public must be considered when designing cDCDD protocols. 212 Clear, standardized protocols help to preserve public trust in organ donation schemes. 213 It is only through public education, debate, feedback, and endorsement that public trust in cDCDD can be ensured. This strategy respects our contention that many of the most important controversies in cDCDD arise from inherently debatable conceptions of death and similarly arguable moral positions on the legitimate scope of medical practice and the principles which guide it. Socially acceptable answers to these debates are one way to ensure that cDCDD rests on firm ethical foundations. However, the consensus on the need for transparency and public feedback evident in academic literature seems not to have translated into robust and effective public education and engagement on the part of transplant organizations. 214 This dissonance is surprising, leading some to worry that a failure to engage robustly with the public is part of a utilitarian-informed “masking strategy” which serves to promote cDCDD at the cost of transparency and a fully informed public. 215
Conclusion
Our overview of the ethical controversies surrounding cDCDD identified emerging agreement in the donation and transplant community on suitable interpretations of the criteria for determinations of death in the context of cDCDD, 216 as well as on the measures necessary to mitigate conflicts of interest in practice. 217 Other issues, especially among bioethicists, remain fractured. There is concern from small but vocal camps which argue that donors can be harmed in cDCDD, that the practice violates the DDR, and that cDCDD will lead to an erosion of public trust in organ donation schemes. That said, the increasingly widespread use of cDCDD suggests that the donation and transplant community considers these issues resolvable through iterative analysis and dialogue. Perhaps the most interesting finding of this review concerns the apparent bifurcation between two categories of issues: the normative/philosophical and the empirical. Our discussion suggests that this cleavage is somewhat artificial, for it illustrates how cDCDD operates at the intersection of science, medicine, law, social science, and philosophy in such a way that insights from each field are required for its ongoing development.
Some of the debates highlighted above are eminently suitable for resolution through empirical research. For example, further data will inform debates on the incidence of autoresuscitation and, consequently, the appropriate no-touch period required following asystole. The uncertain relationship between brain activity and circulatory death will likewise be informed through empirical research. Our prospective study, Neurological Physiology After Removal of Therapy (NeuPART), promises to illuminate the physiological and temporal relationship between neurological and circulatory activity during and after end of life by measuring cortical function using electroencephalogram, cerebral blood flow using transcranial Doppler, and brainstem function using evoked potentials. 218 Other areas amenable to empirical resolution include the risk of harm from antemortem interventions, the likelihood of reanimation through postmortem reperfusion in conjunction with procedures to prevent blood flow to the brain, and the potential impacts of cDCDD on both donor families and public trust.
However, it is clear from our overview of ethical concerns surrounding cDCDD that most debates cannot be resolved through empirical research alone. Prominent issues discussed above point to ongoing disagreement around fundamental moral and metaphysical questions. What is death? What are its indicators? How should we construe “harm”? When can care be altered in the interest of donation? And just what exactly does the DDR prohibit? Since work in a number of fields is required to resolve these issues, progress will only be made with advances in each. Ultimately, the plurality of viewpoints found in the literature is a natural result of not only empirical uncertainties, but also complex debates concerning the metaphysics of death and value-laden judgements concerning the legitimate scope of medical practice. Since moral and metaphysical positions are inherently debatable, we do not foresee the imminent emergence of universal agreement on the propriety of all aspects of cDCDD. Given the dilemmas attending moral and metaphysical debate, it is possible that variation in cDCDD protocol and practice is not just to be expected, but also embraced. If this important and promising form of organ donation is to continue to develop and expand, protocols may have to be adapted to local moral, social and cultural perspectives. While some of the issues discussed in this review are empirically tractable, some of the most contentious are not. This means that any socially acceptable form of cDCDD must emerge from public engagement if it is to reflect societal perspectives on death and the boundaries of medical practice. Further dialogue, public feedback, and analysis are required as cDCDD advances and becomes even more widely used as a means to expand the donor pool.
Note
Charles Weijer receives consulting income from Cardialen, Eli Lilly & Company, and Research Trial Institute (RTI) International. This research was funded by the New Frontiers in Research Fund (grant number: NFRFE-2019-00759). Dr. Slessarev reports funding from Lawson Health Research Institute and from Trillium Gift of Life Network during the course of the study. Dr. Grofton reports grants from the government of Canada and from the Canadian Institutes of Health Research during the course of this study. The remaining authors have no conflicts of interest to disclose.
Appendix 1
PubMED
((“DCD” OR “donation after circulatory death” OR “non-heart-beating organ donation” OR “donation after cardiac death” OR “donation after cardiocirculatory death”) AND (trust OR ethic* OR harm* OR irreversible OR irreversibility OR permanence OR permanent OR “dead donor rule” OR “conflict? of interest” OR consent))
SCOPUS
(TITLE-ABS-KEY (“DCD” OR “donation after circulatory death” OR “non-heart-beating organ donation” OR “donation after cardiac death” OR “donation after cardiocirculatory death”) AND TITLE-ABS-KEY (ethic*) OR TITLE-ABS-KEY (harm*) OR TITLE-ABS-KEY (trust) OR TITLE-ABS-KEY (irreversibility) OR TITLE-ABS-KEY (irreversible) OR TITLE-ABS-KEY (permanence) OR TITLE-ABS-KEY (permanent) OR TITLE-ABS-KEY (“dead donor rule”) OR TITLE-ABS-KEY (“conflict* of interest”) OR TITLE-ABS-KEY (consent)) AND PUBYEAR < 2020
Embase
(“DCD” OR “donation after circulatory death” OR “non-heart-beating organ donation” OR “donation after cardiac death” OR “donation after cardiocirculatory death”) AND (trust OR ethic* OR harm* OR irreversible OR irreversibility OR permanence OR permanent OR “dead donor rule” OR “conflict? of interest” OR consent)
Appendix 2
Donation after circulatory death; non-heart-beating organ donation; donation after cardiac death; donation after cardiocirculatory death
Trust; ethic*; harm*; irreversible; irreversibility; permanence; permanent; dead donor rule; conflict* of interest; consent
Appendix 3
Inclusion criteria. The article, editorial or commentary was included if: the abstract and/or article was accessible through Western University library catalogue/subscribed databases; published in English; explicitly engaged in an analysis or description of at least one issue, concept or argument bearing on the ethics of cDCDD.
Exclusion criteria. Articles were excluded if they were: primarily clinical in focus; primarily legal in focus; primarily religious in focus; a case report; focused only on uDCDD; reported findings on surveys of attitudes towards cDCDD; reported findings on animal studies; discussed issues around cDCDD specific to one country; focused on pediatric cDCDD; focused on cDCDD in the context of specific underlying illnesses. Exceptions were made for articles which were discussed or cited extensively in numerous publications.