Introduction
Normal speech production relies on a complex relationship between the soft palate and the nasopharynx. The production of oral sounds relies on the separation of the oral cavity from the nasal cavity, brought about by co-ordinated movements of the soft palate with the posterior and lateral nasopharyngeal walls. Similarly, elevation of the soft palate against the nasopharyngeal wall during swallowing prevents food and drink passing into the nose. Velopharyngeal inadequacy is the inability to close the velopharyngeal gap between the soft palate and the nasopharynx during speech and/or swallowing, resulting in hypernasal speech and/or airflow errors, and food and/or fluid regurgitation, respectively. Velopharyngeal insufficiency may be caused by inadequate palatal function after cleft palate repair, submucous cleft palate, velopharyngeal disproportion and neuromuscular dysfunction.
Velopharyngeal insufficiency may affect speech intelligibility: in normal English-language speech, most consonants and vowels are produced through the oral cavity, and require no or very little airflow through the nose. Velopharyngeal insufficiency is more common amongst cleft palate children, but it can also develop in those without an overt cleft defect.
Adenoids provide a cushion against which the soft palate is able to close, decreasing the distance it has to travel to effect closure. Adenoids contribute to palatal function during childhood through veloadenoidal valving, as opposed to velopharyngeal valving as seen in adults.Reference Siegel-Sadewitz and Shprintzen1 Adenoidectomy is a commonly performed ENT procedure for children with obstructive sleep apnoea, nasal obstruction and otitis media with effusion. Adenoid removal may result in velopharyngeal insufficiency due to the presence of a submucous cleft or inherent palatal weakness upon removal of the supporting tissue.
We investigated the aetiological factors that contribute to the development of velopharyngeal insufficiency in patients without a known cleft palate. We also reviewed those patients who developed velopharyngeal insufficiency following adenoidectomy in order to identify any predisposing factors in these patients.
Materials and methods
Alder Hey Children's Hospital provides a tertiary referral multidisciplinary cleft palate service covering the Northwest, North Wales and the Isle of Man. These regions collectively have a population of over 7.5 million. Patients born between 2000 and 2013 referred to the cleft service with possible velopharyngeal insufficiency were identified from the cleft unit database.
Patients are referred from doctors in either primary or secondary care, or from community speech and language therapists. Initially, these patients are reviewed by the cleft unit speech and language therapists. A thorough consultation will then take place, and a diagnosis of velopharyngeal insufficiency will be considered or excluded. Patients who need further assessment and/or consideration for surgery are referred to the cleft surgeon.
A retrospective electronic case note review of these patients was undertaken. The data collected were analysed in order to identify any patterns in patients diagnosed with velopharyngeal insufficiency, especially in those who developed it following adenoidectomy. The data were scrutinised using quantitative analysis.
No ethical approval was needed for this study, as advised by the local research department.
Results
The database identified 159 patients who were referred to cleft services with a potential diagnosis of non-cleft velopharyngeal insufficiency. Figure 1 summarises our findings.
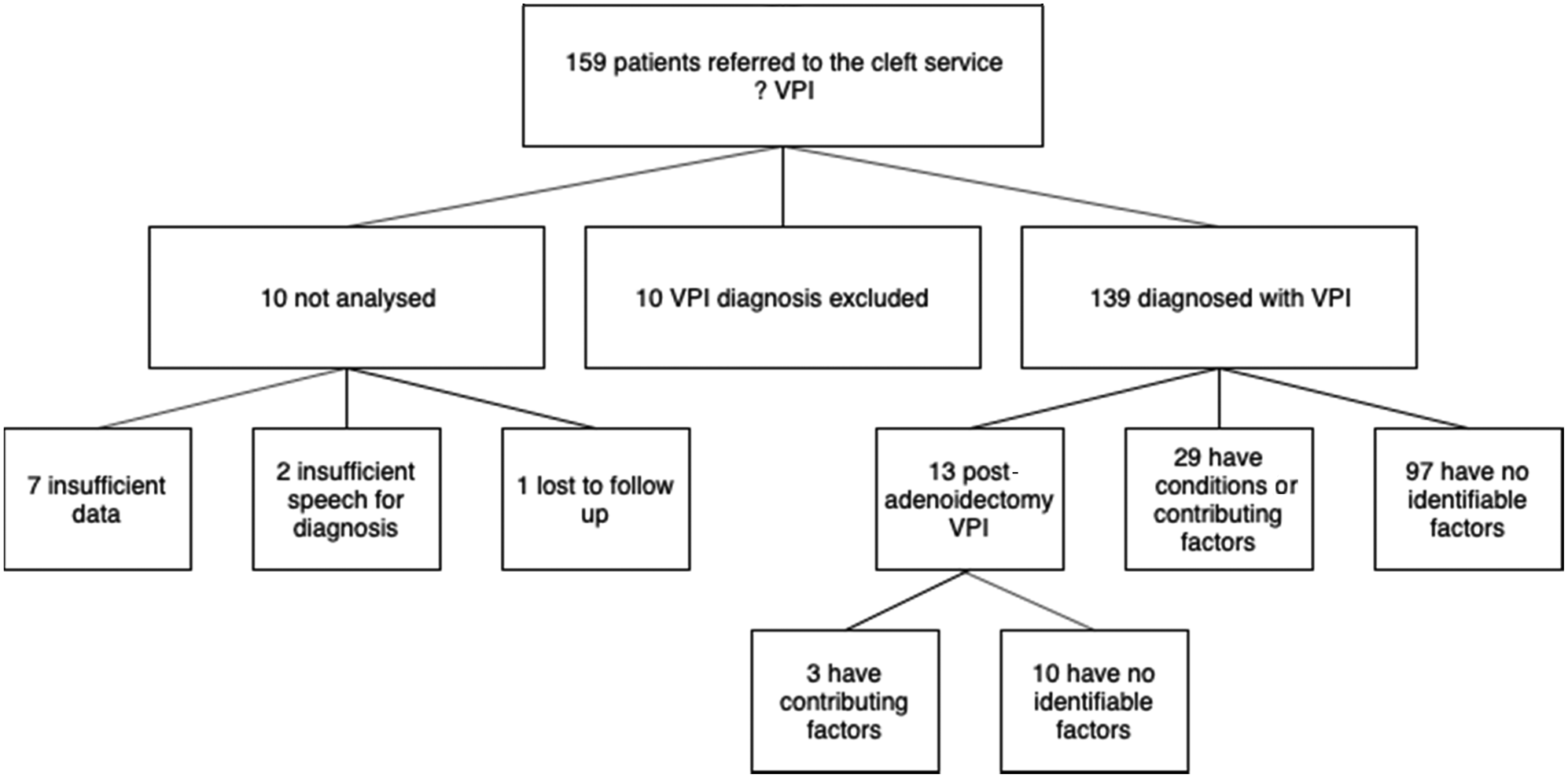
Fig. 1. Summary of 159 non-cleft patients analysed from our centre database. VPI = velopharyngeal insufficiency
A total of 139 patients were diagnosed with velopharyngeal insufficiency. Thirteen patients were diagnosed with velopharyngeal insufficiency following adenoidectomy. One of these patients had an undiagnosed submucous cleft palate. Table 1 summarises the identifiable factors and conditions that contributed or may have contributed to the development of velopharyngeal insufficiency.
Table 1. Factors potentially contributing to velopharyngeal insufficiency development, for all patients
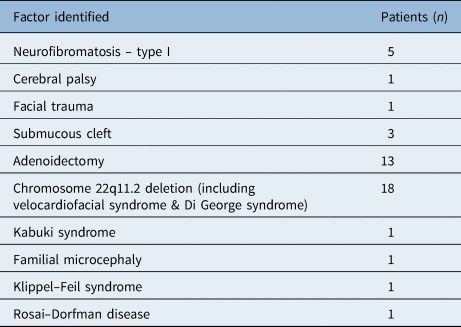
A total of 123 patients required surgical intervention following the diagnosis of velopharyngeal insufficiency. Of the 13 children diagnosed with velopharyngeal insufficiency following adenoidectomy, 11 (85 per cent) needed surgical treatment. Table 2 indicates conditions that are likely to precipitate velopharyngeal insufficiency following adenoidectomy or adenotonsillectomy.
Table 2. Factors contributing to velopharyngeal insufficiency development following adenoidectomy

Discussion
In 1953, CalnanReference Calnan2 first highlighted the risk of hypernasal speech as a complication following adenoidectomy. Velopharyngeal insufficiency is a rare complication of adenoidectomy that can result in substantial morbidity.
Eighty-five per cent of all post-adenoidectomy velopharyngeal insufficiencies in our cohort required surgical intervention. Surgery for velopharyngeal insufficiency took place following a thorough assessment by the speech therapists when conservative management was deemed inappropriate. The surgery was tailored to the anatomical deficiency indicated by the instrumental evaluation of velopharyngeal function. The surgery was successful in improving the symptoms of velopharyngeal insufficiency in all cases.
The velopharyngeal insufficiency incidence quoted over the years has remained similar, and ranges from 1 in 1500 to 1 in 10 000.Reference Gibb3,Reference Witzel, Rich, Margar-Bacal and Cox4 In our non-cleft population, adenoidectomy was not an uncommon cause for velopharyngeal insufficiency (1 in 10 children who developed velopharyngeal insufficiency had undergone adenoidectomy). Hospital Episode Statistics data recorded 7593 adenoidectomies in England in the year 2005–2006.Reference Lowe, Brown and Yung5 If we assume proportionally that around 1000 adenoidectomies were performed in the population area included in our study in one year, the number of adenoidectomies which resulted in velopharyngeal insufficiency over the study time frame is very small. The implications for the consent process are, nonetheless, important.
Only 3 of the 13 children who developed velopharyngeal insufficiency following adenoidectomy had an identifiable contributing factor. One of the post-adenoidectomy velopharyngeal insufficiency children had a submucous cleft palate that was not diagnosed at the time of surgery. This was diagnosed at the centre, but it was not clear how clinically apparent it was. A total adenoidectomy was performed in this patient. The other two patients with the condition had already been diagnosed at the time of referral. It was not clear from the operative notes whether a total or partial adenoidectomy was performed.
Submucous cleft palate is a condition well recognised by ENT surgeons, with the typical appearance of a bifid uvula, a midline lucency of the soft palate and notching of the hard palate.Reference Calnan2 The palatal hypofunction that results from the associated muscular abnormalities is known to carry a high risk of velopharyngeal insufficiency should an adenoidectomy be performed.Reference Saunders, Hartley, Sell and Sommerlad6 An occult submucous cleft is a less well-recognised anatomical anomaly. It involves abnormality of the structure and function of the palatal musculature, but is not always detectable on oral examination. A nasendoscopic examination may help in identifying certain signs such as absence of the usual convex appearance of the superior surface of the soft palate, or even a midline groove – the so-called ‘seagull sign’ – due to absence of the muscularis uvulae.Reference Tweedie, Skilbeck, Wyatt and Cochrane7 However, the bulky adenoids may prevent visualisation of the aforementioned signs during nasopharyngoscopy.
The diagnosis of velopharyngeal insufficiency requires a thorough assessment by a specialised multidisciplinary team of speech and language therapists and cleft surgeons. Following perceptual speech assessment, plain lateral view videofluoroscopy is the normal standard in our cleft unit. Depending on the findings, a modified Towne's view can also be used. Our radiologists estimate an average radiation dose of 20–25 mGy/m2. Nasopharyngoscopy is frequently used by the specialists during the velopharyngeal insufficiency assessment and when planning for surgery. A study by Ysunza et al.Reference Ysunza, Bloom, Chaiyasate, Rontal, VanHulle and Shaheen8 concluded that a combination of multiplanar videofluoroscopy and flexible nasopharyngoscopy is a highly reliable procedure for assessing velopharyngeal closure, and to surgically and successfully correct velopharyngeal insufficiency.
The database does not include the diagnostic modalities for the genetic abnormalities that feature in patients’ background. Liverpool Women's Hospital provides a regional genetics service that covers the same area as the population of this study. Common diagnostic procedures include targeted fluorescence in situ hybridisation testing, which is considered an excellent diagnostic procedure for patients with clinical suspicion of 22q11.2 deletion, and array comparative genomic hybridisation, which is an indirect whole genome study.
Two of the children who underwent adenoidectomy and later developed velopharyngeal insufficiency had syndromes: one had velocardiofacial syndrome and the other had neurofibromatosis. The syndromes in both these children were established prior to the adenoidectomy procedure. Children with velocardiofacial syndrome have a poor muscular tone of the velopharynx, which predisposes them to develop velopharyngeal insufficiency. Other syndromes in our cohort of children diagnosed with velopharyngeal insufficiency were: Klippel–Feil syndrome, Kabuki syndrome and neurofibromatosis. Vertebral anomalies, anal atresia, tracheoesophageal fistula and renal anomalies (‘VATER’) syndrome and Turner syndrome have also been mentioned in other studies.Reference Goudy, Ingraham and Canady9 It has been shown that velopharyngeal insufficiency following adenoidectomy can occur in patients with an undiagnosed craniofacial syndrome; hence, some authors have highlighted the importance of genetic screening in such patients. Perkins et al.Reference Perkins, Sie and Gray10 showed that the 22q11 deletion test is beneficial in diagnosing patients with genotypic, but not phenotypic, velocardiofacial syndrome, in their study population of patients without cleft palate who developed velopharyngeal insufficiency following adenoidectomy.
Benefits of the surgery must outweigh the potential risk of developing velopharyngeal insufficiency when considering adenoidectomy in children with predisposing factors. Obstructive sleep apnoea is one indication that can necessitate adenoidectomy, even in patients with a cleft palate. Sleep-related breathing abnormalities may be associated with deleterious effects, including impaired daytime psychomotor performance, enuresis, hyperactivity and poor sleep quality.Reference Ali, Pitson and Stradling11 Untreated chronic mouth breathing in children might lead to unfavourable developmental changes in the craniofacial complex that predispose them to obstructive sleep apnoea in adulthood. Adenoidectomy should be carried out to correct persistent nasal obstruction early in life, even if, as in most cases, the adenoid is expected to spontaneously involute.Reference Guilleminault12,Reference Finkelstein, Wexler, Berger, Nachmany, Shapiro-Feinberg and Ophir13
The adenoidectomy technique can be quite important, especially in children where adenoidectomy may lead to the development of velopharyngeal insufficiency. Partial adenoidectomy has gained momentum over the years in many centres following its advocated use in children with known cleft palate. Tweedie et al.Reference Tweedie, Skilbeck, Wyatt and Cochrane7 showed no new onset or worsening of existing velopharyngeal insufficiency in children with known cleft palate who underwent suction diathermy partial adenoidectomy. Murray et al.Reference Murray, Fitzpatrick and Guarisco14 noted the benefits of the microdebrider in attaining precision when performing partial adenoidectomy. In our centre, the Coblator® with indirect visualisation is used. Fifty to 80 per cent of the superior adenoid is usually removed during the partial adenoidectomy, with the inferior part left intact. This can be further tailored to the anatomy of individual patients – for example, more tissue needs to be left behind if the palate is short. The principle in all partial adenoidectomy techniques is adenoid visualisation, to allow the surgeon to plan, with precision, the amount and site of adenoid tissue left behind.
Seventy-seven per cent of the patients who developed velopharyngeal insufficiency following adenoidectomy did not have any identifiable predisposing factors. This study indicates that whilst a few cases may be potentially predictable, most are not. It is therefore essential to mention this complication during the consent process, as, although it is rare, this complication is associated with significant morbidity. The 2015 Montgomery versus Lanarkshire Health Board case highlighted the crucial importance of informing patients of all risks, despite their low frequency or their perceived significance by the doctor.
• Velopharyngeal insufficiency carries substantial morbidity and may require surgical intervention
• This disorder can occur in children with no known cleft palate, and a range of conditions may contribute to its development
• Adenoidectomy, a common ENT procedure in children, can precipitate velopharyngeal insufficiency
• This study found no identifiable contributing factors in most children who developed velopharyngeal insufficiency following adenoidectomy
• It is important to consider velopharyngeal insufficiency as a complication when contemplating and consenting for adenoidectomy
It is important for the ENT surgeon to be aware of the services available for potential referrals when velopharyngeal insufficiency following adenoidectomy is suspected. It is, however, equally important to emphasise that spontaneous improvement in hypernasal speech may occur a significant length of time after adenoidectomy. That being the case, the true incidence of velopharyngeal insufficiency may well be underestimated, considering that patients who have symptoms may not seek further assistance, especially when these symptoms improve. DonnellyReference Donnelly15 suggests that it can take up to a year for the spontaneous resolution of hypernasality. Witzel et al.Reference Witzel, Rich, Margar-Bacal and Cox4 recommend that surgery is not considered for at least a year if the patient shows continuous improvement.
Conclusion
Velopharyngeal insufficiency is a serious albeit uncommon complication following adenoidectomy. The presence of a submucous cleft palate and syndromic aetiologies such as velocardiofacial syndrome should alert the surgeon to the potential development of velopharyngeal insufficiency following adenoid removal. It is, however, difficult to predict which patients will develop velopharyngeal insufficiency following this ENT procedure in the absence of background predisposing factors. We could not identify a predisposing aetiology in 77 per cent of children who developed velopharyngeal insufficiency following adenoidectomy.
Whilst there is undeniable evidence for thorough history-taking and examination, as well as appropriate surgical technique, we feel it is essential that in children without a known cleft palate, the risk of velopharyngeal insufficiency following adenoidectomy is clearly explained during the consent process. Hypernasality following adenoidectomy can resolve spontaneously or with further surgery. Follow up of these patients over at least a year is important to check on the progress of this symptom.
Competing interests
None declared





