Introduction
A varix of the retromandibular vein can be a very rare cause of a mass in the parotid gland. We describe a case of an incidental finding of a varix of the retromandibular vein. This condition may be confused with a pleomorphic adenoma of the parotid gland on magnetic resonance imaging (MRI); we therefore highlight the importance of considering a broad differential diagnosis of a parotid mass and of always obtaining dedicated imaging of the lesion.
Case report
A 64-year-old lady presented to the ENT clinic with unilateral, left-sided tinnitus. There was no associated hearing impairment, vertigo or facial weakness. Otoscopic examination was unremarkable. Examination of the neck revealed no palpable masses or lymphadenopathy. An MRI was arranged to exclude pathology in the posterior fossa, for example, a cerebellopontine angle mass such as a vestibular schwannoma.
Magnetic resonance imaging demonstrated no abnormality within the inner ears, internal auditory meatus, cerebellopontine angles or brainstem. An incidental, well circumscribed, 2.6 cm × 2.0 cm × 3.4 cm mass was noted in the left parotid gland on the gradient echo T2 scout images (these are rapidly acquired images used to plan the diagnostic sequences) (Figure 1c). The lesion involved the superficial and deep lobe of the gland, and returned a relatively high signal on these images. It was thought likely to be an incidental finding of a left parotid pleomorphic adenoma. Cytological diagnosis was therefore considered necessary in order to inform whether the mass should be surgically removed or managed conservatively with serial scans. A malignant cytology would suggest surgical removal. As the mass was not palpable, an ultrasound-guided fine needle aspiration of the lesion was arranged.
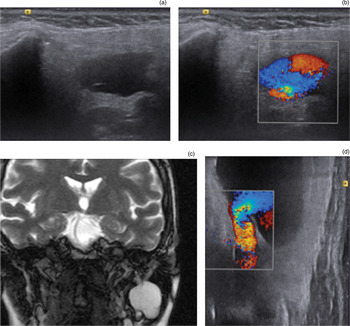
Fig. 1 (a) An axial ultrasound scan showing the varix of the retromandibular vein; (b) an axial colour Doppler ultrasound scan demonstrating the ‘yin and yang’ sign; (c) a coronal T2 magnetic resonance scout image showing a mass within the left parotid; and (d) a coronal Doppler ultrasound scan demonstrating vein outflow.
The ultrasound demonstrated an anechoic and compressible mass, which was contained entirely within the left parotid at the junction of the deep and superficial gland. The mass was in continuity with the retromandibular vein inferiorly, and both the mass and distal vein increased in size on Valsalva's manoeuvre. Doppler interrogation demonstrated a ‘yin and yang’ appearance within the sac, which is typical of an aneurysm or varix (Figure 1). There was continuous venous flow in the outflowing vein. On tracing the draining vessel inferiorly, the vein was demonstrated to be a tributary of the external jugular. It was concluded that the mass in fact represented a varix of the retromandibular vein within the parotid, and not a pleomorphic adenoma as initially presumed. Fine needle aspiration cytology was not performed.
The patient was reviewed in clinic. Re-examination demonstrated no palpable mass and no facial nerve palsy. As the lesion was asymptomatic, it was decided that no intervention or monitoring was required.
Discussion
This case demonstrates a rare cause of a parotid mass. However, this cause must be considered in order to provide an accurate diagnosis and avoid unnecessary surgical intervention.
A PubMed search was performed using the following combinations of terms: ‘retromandibular’, ‘vein’ and ‘varix’; ‘retromandibular’ and ‘varix’; ‘parotid’ and ‘varix’; ‘parotid’ and ‘vein’; ‘venous’, ‘aneurysm’ and ‘parotid’; and ‘venous’, ‘ectasia’ and ‘parotid’. Venous anomalies of the parotid gland are very rare, and there were no previous reports of an incidental parotid varix being detected on MRI. The differential diagnosis of venous anomalies of the parotid gland included varices,Reference Jahnke1 haemangioma,Reference Lacomme and Massat2, Reference Dempsey and Murley3 venous aneurysms,Reference Strome4, Reference Jensen and Reingold5 venous ectasiaReference Schulman, Carothers and Gould6, Reference Manni, Merx, van den Broek and Thijssen7 and venous malformations.Reference Saeed, Kolhe, Smith and Murray8
In the case reported here, the parotid lesion was found incidentally on the periphery of scout imaging performed for another indication. However, the cases reported in the literature primarily described how a clinically apparent venous mass of the parotid gland may be clinically differentiated from other causes of masses in the parotid region. For instance, the ‘turkey wattle’ sign, which describes enlargement of a facial mass on dependency of the head, is thought to be pathognomonic of venous anomalies or haemangiomas.Reference Patey9 Although it is a specific clinical sign, a review of this sign suggests that it is frequently not present,Reference Saeed, Kolhe, Smith and Murray8 which is corroborated by the findings in the present case. Vascular masses can also be enlarged by the Valsalva manoeuvre, they are easily compressible, and do not have a palpable bruit or thrill.Reference Schulman, Carothers and Gould6
Imaging modalities used in previous cases of venous malformations include ultrasonography,Reference Jensen and Reingold5, Reference Manni, Merx, van den Broek and Thijssen7 computed tomography (CT),Reference Manni, Merx, van den Broek and Thijssen7 venographyReference Schulman, Carothers and Gould6, Reference Manni, Merx, van den Broek and Thijssen7 and MRI.Reference Saeed, Kolhe, Smith and Murray8 Ultrasound has been reported to reveal no specific diagnostic features in the case of venous ectasia,Reference Manni, Merx, van den Broek and Thijssen7 and a venous aneurysm was incorrectly thought to be a parotid gland tumour using this technique.Reference Jensen and Reingold5 However, Doppler ultrasound and the Valsalva manoeuvre were not used in either of these two cases. In another case report, non-contrast CT was not useful in defining venous ectasia; the technique simply demonstrated lateral displacement of the parotid.Reference Manni, Merx, van den Broek and Thijssen7 Venography was useful in defining the anatomy of the venous anomaly in that case; however, it is a more invasive procedure. In another study, MRI was able to demonstrate a discrete mass with adjacent dilated vessels, which is consistent with other reports identifying venous malformations.Reference Saeed, Kolhe, Smith and Murray8 The definitive diagnosis in these cases involved surgical resection and histology, rather than imaging. However, imaging techniques have improved since these reports. In addition, there were no previous reports of MRI used in the identification of a parotid varix, or of the use of Doppler ultrasound.
• Venous abnormalities in the parotid region are extremely rare
• Misdiagnosis has previously led to unnecessary surgical resection
• Appropriate radiological investigation allows early diagnosis and prevents unnecessary invasive procedures
In reporting this case, we have highlighted that MRI is very sensitive at demonstrating incidental abnormal findings in the periphery of the field of view. However, without dedicated imaging, the specificity for characterising the abnormality is not sufficient. In this case, the confusion in preliminary diagnosis was due to the fact that flowing blood returns a high signal on scout gradient echo images which mimics the signal of a pleomorphic adenoma, whereas diagnostic MRI sequences of the neck would have used spin echo sequences where a flow void is likely to have been confirmed. If dedicated imaging had not been performed, this could have led to unnecessary surgery to remove the lesion.
We have shown that Doppler ultrasound combined with the Valsalva manoeuvre during imaging is sufficient to differentiate a retromandibular varix of the parotid from a pleomorphic adenoma, which to our knowledge, has not been previously reported.
Conclusion
A retromandibular varix of the parotid gland is a rare differential diagnosis that must be considered for a mass in the parotid gland. The number of incidental findings (‘incidentaloma’) is rising with the increasing availability and use of radiological investigations. It is important that any incidental finding is assessed with the appropriate modality of investigation to ensure accurate diagnosis and subsequent management.



