Introduction
Local anaesthetic agents can be used to anaesthetise the external ear canal and tympanic membrane during minor ear procedures, such as myringotomy and grommet insertion or intratympanic steroid injection. A variety of agents have previously been used in the out-patient setting, including injectable anaesthetic agents, topical creams and aqueous solutions.
Topical creams such as those containing lidocaine (Emla™)Reference Luotonen, Laitakari, Karjalainen and Jokinen1 and tetracaine gel (Ametop®)Reference Carrasco, Prazma and Biggers2 need to be administered under direct microscopic vision, require 20–30 minutes to have an effect and can be time-consuming to completely remove prior to the procedure.
Injectable anaesthetic agents have the benefit of working quickly, but can be painful for the patient, and may lead to swelling of the external canal, which obscures visualisation of the tympanic membrane.
Topical aqueous anaesthetic solutions are favoured by some clinicians. Phenol has been shown to be effective,Reference Sing3–Reference Syed, Rutka and Pothier5 but carries the risk of neurotoxicity leading to sensorineural hearing loss. It also causes a stinging sensation on application to the tympanic membrane and can result in chemical burns when unintentionally applied to the external auditory canal skin.
Lidocaine (Xylocaine®) spray is a rapid-acting local anaesthetic that binds reversibly to sodium channels, preventing the movement of sodium ions into the nerve fibres, resulting in depolarisation.6 It is commonly used in otorhinolaryngology for minor non-invasive procedures in the nasal cavity, pharynx and larynx. The effectiveness of Xylocaine spray as a topical anaesthetic has not previously been investigated in patients undergoing minor ear procedures.
Materials and methods
Participants undergoing grommet insertion or intratympanic steroid injection were recruited prospectively over six months in the ENT out-patient clinic at Royal Albert Edward Infirmary, Wigan, UK. The exclusion criteria were: participants aged under 18 years, pre-existing tympanic membrane perforations and significant anxiety regarding a procedure performed under local anaesthetic. All participants were verbally consented prior to the procedure, including being informed of the risk of local anaesthetic failure.
Procedural steps
The patient is asked to lie on an examination couch with the backrest elevated to 45 degrees and their head turned so their ear is facing upwards. The ear is microsuctioned to remove wax and debris from within the ear canal. Xylocaine 10 mg spray is administered into the canal under direct vision using four to five pumps of the spray via a single-use 120 mm plastic nozzle (Figure 1). Xylocaine 10 mg spray administers 10 mg of lidocaine with each depression of the nozzle, with a maximum dose of 20 depressions used per procedure.6 Cotton wool is used to occlude the lateral external ear canal. The patient is asked to lie in this position for 10 minutes. Under microscopic vision, excess anaesthetic solution and any remaining wax or debris in the canal is then microsuctioned to obtain a clear unobstructed view of the tympanic membrane prior to the desired procedure.
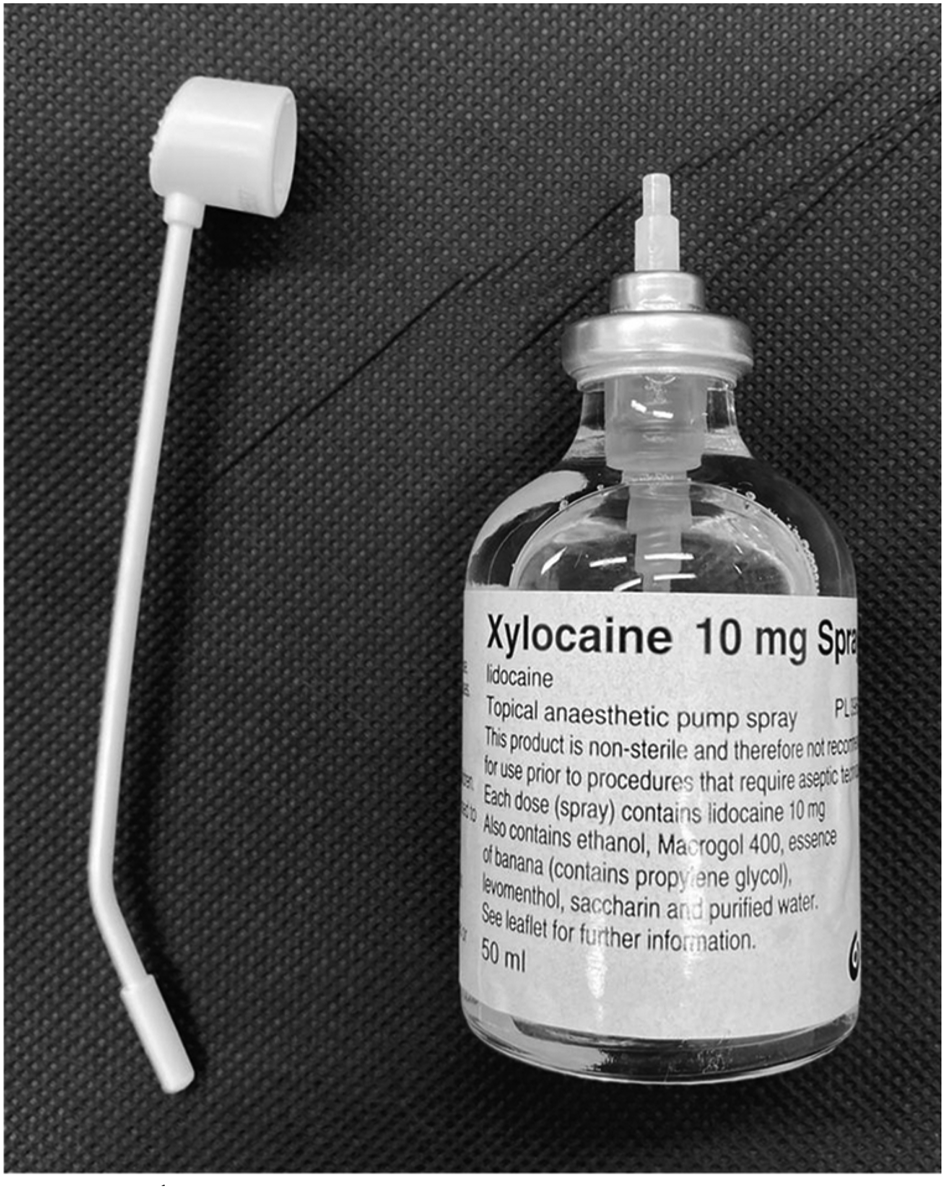
Fig. 1. Xylocaine spray with single-use 120 mm plastic nozzle.
Questionnaire
Participants were asked to complete a short questionnaire after the procedure regarding their experience. The questionnaire included three questions: (1) How painful was the procedure from 0–10? (participants rated their perceived level of pain on an 11-point visual analogue scale (VAS) with Wong-Baker Faces®); (2) Overall, how did you find the procedure? (with the possible answers being ‘pleasant’, ‘slightly unpleasant’, ‘unpleasant’ and ‘very unpleasant’; and (3) Would you undergo the procedure again? (participants answered ‘yes’ or ‘no’). The anonymised data were collated and analysed on Microsoft Excel spreadsheet software.
Results
Eighteen patients underwent out-patient local anaesthetic minor ear procedures with Xylocaine spray over a six-month period from January to July 2021. The median age of patients was 55 years (age range of 30–86 years), and 67 per cent were female. Twelve participants underwent myringotomy and grommet insertion; six participants had intratympanic steroid injections.
The median perceived level of pain measured on the VAS was 2 out of 10, with six patients (33 per cent) reporting no pain at all (Figure 2). Eight patients (44 per cent) reported their overall experience as pleasant (Figure 3), with the remainder recalling the experience as slightly unpleasant (66 per cent). None of the procedures were abandoned because of anaesthetic failure, pain or patient anxiety. All participants stated they would undergo the procedure again and there were no peri-operative complications.

Fig. 2. Post-operative scores for the question ‘how painful was the procedure from 0 to 10?’, rated using an 11-point visual analogue scale (VAS) with Wong-Baker Faces.

Fig. 3. Post-operative frequency of scores for the question ‘overall, how did you find the procedure?
Discussion
Lidocaine spray is an effective and efficient method for anaesthetising the external ear canal, and is well tolerated by patients. The aqueous solution allows for simple administration without a microscope, and ensures complete coverage of the tympanic membrane. Topical creams may form air pockets, preventing complete anaesthesia; local anaesthetic injections can be painful and lead to canal swelling. Excess aqueous solution can be rapidly removed compared to cream; cream may leave behind residue despite liberal microsuction, often obscuring an already restricted view of the tympanic membrane. The spray also helps to soften wax and debris in the canal, facilitating removal.
Depending on the area of application, anaesthesia from Xylocaine spray usually occurs within 1–5 minutes and is intended for use on mucous membranes during minor dental or aerodigestive tract procedures.6 Despite aqueous local anaesthetic solutions normally being poorly absorbed through skin, it has been suggested the solution is effective on the tympanic membrane as the skin is very thin.Reference Lim, Alatsatianos and Wardrop7 In this study, the spray was administered 10 minutes before starting the procedure to ensure maximal effect; however, perhaps 5 minutes would be adequate in future trials. This short time to effect compared to topical creams improves efficiency in a busy clinic, especially in departments with limited microscope or treatment room availability.
Phenol aqueous solution is applied directly to the tympanic membrane with a wax curette or similar instrument. It causes a partial thickness chemical burn, leading to the necrosis of sensory nerve endings and instant anaesthesia.Reference Syed, Rutka and Pothier5 This comes with a theoretical risk of membrane perforation, although one large study found the risk to be 0.017 per cent,Reference Sing3 with other series reporting no perforations.Reference Robertson, Whitwell and Osborne4,Reference Syed, Rutka and Pothier5 Precision is required to avoid touching the external canal skin, which can cause burns; therefore, the appropriate selection of co-operative patients is essential. There are concerns about long-term damage to the tympanic membrane, with reports of an inflammatory response lasting up to five months.Reference Schmidt and Hellstrom8 More practically, phenol is not readily available in ENT departments in the UK because of its neurotoxic potential to cause sensorineural hearing loss. The concentration of the solution is also not standardised, and varies from 20 to 90 per cent in the literature, which is a potential barrier to more widespread popularity.Reference Sing3–Reference Syed, Rutka and Pothier5 In contrast, Xylocaine spray is available in most ENT departments with a standard concentration, and does not require instrument application.
The use of Co-Phenylcaine™ spray has been reported for minor ear procedures and has similar advantages to the use of Xylocaine spray described in this study. However, the effectiveness of Co-Phenylcaine to anaesthetise the tympanic membrane is based on anecdotal evidence and has not been validated in a group of patients.Reference Lim, Alatsatianos and Wardrop7
The current study used an 11-point VAS to determine the perceived level of pain, which is a validated and reliable tool for measuring pain intensity.Reference Jensen and McFarland9 A median score of 2 out of 10 during the procedure confirms that the technique was well tolerated, with 100 per cent of patients stating they would undergo the procedure again. Patient selection for procedures under local anaesthetic is important, and a comprehensive explanation of the steps involved is key, to ensure co-operation and reduce anxiety.
This study involved only a small sample size; the effectiveness of Xylocaine spray should be further evaluated in a larger group of patients. The frequencies of long-term complications and perforations were not assessed. However, phenol has a very low perforation risk of 0.017 per centReference Sing3 and works by causing a partial thickness burn; lidocaine functions solely by blocking sodium channels and therefore the risk may be even lower. One advantage of the local cauterisation caused by phenol is reduced bleeding, comparable to the effect of adrenaline within Co-Phenylcaine. Nevertheless, this study observed minimal bleeding with Xylocaine spray and all procedures were successfully completed.
• Injectable anaesthetic agents, topical creams and aqueous solutions have been used for local anaesthesia of the tympanic membrane
• Grommet insertion and intratympanic steroid injection can be performed on adults with local anaesthetic in out-patient clinics
• Topical creams take 20–30 minutes to work, and injectable agents can be painful and cause canal swelling
• Xylocaine spray works in 1–5 minutes and is easily microsuctioned
• Prospective analysis revealed that Xylocaine spray is safe, effective and well tolerated by patients for minor ear procedures in clinic
The overall patient experience was reported as either pleasant or slightly unpleasant. It was somewhat surprising that 44 per cent described a minor ear procedure as pleasant; this was perhaps partly because of the welcoming and reassuring nature of our clinical team, in addition to the effectiveness of Xylocaine spray.
Conclusion
Xylocaine spray is a safe and effective method for anaesthetising the tympanic membrane during minor ear procedures. It is simple to administer and can be easily microsuctioned to obtain an unobstructed view of the tympanic membrane. The technique is well tolerated by patients and can help improve efficiency in busy out-patient departments.
Competing interests
None declared





