Introduction
Myeloid sarcoma and acute fulminant invasive fungal sinusitis are distinct but equally fatal diseases and require different treatment. Coexistence of these two conditions in the sinonasal cavity is exceedingly rare and can present a diagnostic challenge, as either one could be masked by the other due to their similar clinical features. This diagnostic dilemma may lead to delayed or missed diagnosis, with rapid progression and death. To the best of our knowledge, the coexistence of these two distinct conditions has not been previously reported in the relevant literature.
We report a case of concurrent sinonasal myeloid sarcoma and acute fulminant invasive fungal sinusitis with rapid intracranial and orbital invasion in a patient with relapsed acute myeloid leukaemia.
Case report
A 73-year-old man was diagnosed with acute myeloid leukaemia (M6 according to the French-American-British classification) in March 2009. Cytogenetic analysis of the bone marrow revealed a normal karyotype. On molecular analysis, mutations of the nucleophosmin gene (NPM1) and the fms-like tyrosine kinase 3 gene (FLT3) were not detected. Induction chemotherapy with idarubicin and cytarabine was administered, and complete remission was attained.
However, the patient relapsed in February 2010, with bone marrow aspirate showing 15 per cent blasts. He received two courses of azacytidine as salvage therapy.
In June 2010, he began suffering from an intermittent, dull pain in the left temporal and orbital regions. Sinus computed tomography (CT) showed only an increased soft tissue density in the left ethmoid sinus (Figure 1), and a tentative diagnosis of ethmoid sinusitis was made. Antibiotics and anti-inflammatory drugs provided relief from pain.

Fig. 1 Initial axial sinus computed tomography scan showing a localised lesion in the left ethmoid sinus (arrow).
However, one month later the patient developed a gradually progressive, dull pain in the left eye. Proptosis and blurred vision were observed in this eye. A second sinus CT (Figure 2a and 2b) showed heterogeneous enhancement of both ethmoid sinuses, intracranial extension to both frontal bases, and bony destruction of both cribriform plates (more significant on the left side). Left orbital invasion involving the left superior and medial rectus muscles was also identified. Endoscopic rhinoscopy (Figure 2c) revealed white discoloration of the mucosa and necrotic tissue in the left nasal cavity, mainly on the posterosuperior nasal septum.
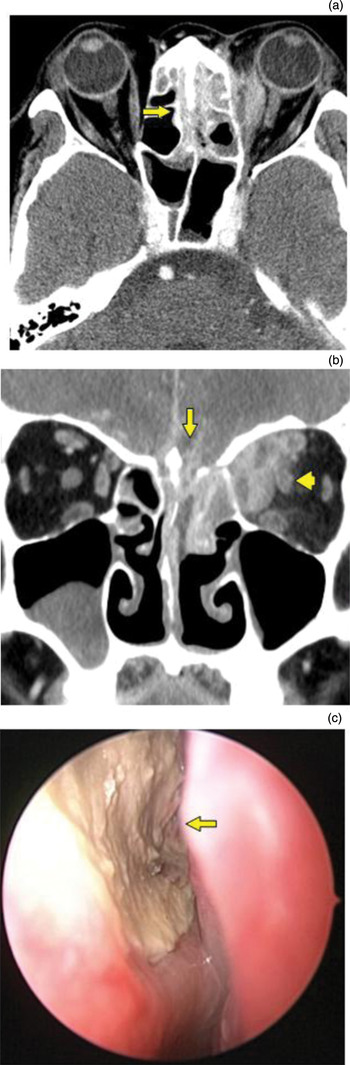
Fig. 2 (a) Repeated axial sinus computed tomography (CT) scan showing an extensive mass with invasion of both ethmoid sinuses (arrow). (b) Coronal sinus CT scan showing intracranial extension to both frontal bases, with bony destruction of both cribriform plates (arrow), together with left orbital invasion involving the left superior and medial rectus muscles (arrowhead). (c) Endoscopic rhinoscopy view showing oedematous mucosa and gangrenous necrosis of the left sinonasal cavity, mainly on the posterosuperior nasal septum (arrow).
Endoscopic debridement was performed under a provisional diagnosis of acute fulminant invasive fungal sinusitis. Further debridement of necrotic tissue revealed gangrenous necrosis of the mucoperiosteum with destruction of adjacent bony structures in the left sinonasal cavity. Erosion of the lamina papyracea and ethmoid roof was also observed on the left side.
Histopathological analysis of the necrotic tissue (Figure 3a) demonstrated colonies of fungal hyphae which were reactive to periodic acid-Schiff staining and were septated with predominant acute angle branching. Fungal culture yielded aspergillus species. The histopathological and endoscopic findings indicated the presence of acute fulminant invasive fungal sinusitis. Curiously, infiltration of leukaemic cells was also observed in the necrotic tissue (Figure 3b). Upon immunohistochemical analysis, the cells were noted to be positive for myeloperoxidase and cluster of differentiation 117 protein (Figure 3c) but negative for cluster of differentiation 34 protein. These findings were consistent with myeloid sarcoma.

Fig. 3 Photomicrographs showing: (a) septated fungal hyphae with predominant acute angle branching, reactive for periodic acid-Schiff staining (×200); (b) infiltration of leukaemic cells (H&E; ×200); and (c) leukaemic cells positive for cluster of differentiation 117 protein immunostaining (×200).
The patient's clinical picture, imaging features, surgical findings, and histopathological and immunohistochemical evidence suggested the coexistence of sinonasal myeloid sarcoma and acute fulminant invasive fungal sinusitis, with intracranial and orbital invasion.
Following surgical debridement, the patient gained significant relief from the dull pain in his left temporal and orbital regions. We initiated intravenous administration of liposomal amphotericin B (4 mg/kg/day) for acute fulminant invasive fungal sinusitis, and radiotherapy for sinonasal myeloid sarcoma.
Three weeks after surgery, repeated fungal culture revealed negative findings.
Unfortunately, two months after surgery the patient expired due to a new episode of neutropenic fever and septic shock.
Discussion
Myeloid sarcoma is an extramedullary solid tumour composed of immature myeloid cells. This tumour is also known as chloroma and granulocytic sarcoma.Reference Jo, Chi and Cho1, Reference Pileri, Ascani, Cox, Campidelli, Bacci and Piccioli2 Myeloid sarcoma is associated with acute myeloid leukaemia, and it can occur during either leukaemia remission or relapse,Reference Pileri, Ascani, Cox, Campidelli, Bacci and Piccioli2 as noted in our patient. Myeloid sarcoma occurs in only 3–9 per cent of all acute myeloid leukaemia cases and is more common in children.Reference Ferri, Minotto, Ianniello, Cavaleri, Armato and Capuzzo3 Although myeloid sarcoma may occur in any organ, the head and neck region accounts for only 12 per cent of cases;Reference Neiman, Barcos, Berard, Bonner, Mann and Rydell4 the most commonly involved sites in this region are the soft palate, nasopharynx and orbit.Reference Ferri, Minotto, Ianniello, Cavaleri, Armato and Capuzzo3 Involvement of the sinonasal cavity is exceedingly rare, with only a few reported cases.Reference Jo, Chi and Cho1, Reference Ferri, Minotto, Ianniello, Cavaleri, Armato and Capuzzo3, Reference Prades, Alaani, Mosnier, Dumollard and Martin5, Reference Gorman, Ahmed, Pallera and Samant6 Histopathological and immunohistochemical analysis is required for definitive diagnosis. On immunohistochemical analysis, the cells stain positive for myeloperoxidase and cluster of differentiation 117 protein, but negative for cluster of differentiation 34 protein. Treatment involves local surgical extirpation, radiotherapy and chemotherapy.Reference Sarvis and Auge7
Acute fulminant invasive fungal sinusitis results from the rapid spread of fungi from the nasal and sinus mucosa by way of vascular invasion into the orbit, vessels and parenchyma of the brain.Reference Epstein and Kern8
Cases of concurrent acute fulminant invasive fungal sinusitis and myeloid sarcoma within the sinonasal cavity are extremely uncommon. The combined destructive effect of the two diseases may lead to rapid progression and death. In our case, we observed rapid progression from a localised sinonasal lesion to an extensive intracranial mass, within one month. Additionally, the diagnostic challenge came not only from the rarity of both diseases in a patient with relapsed acute myeloid leukaemia, but from their coexistence in the sinonasal cavity. This is because the clinical presentations of both diseases are quite similar, and thus either one could be masked by the other. For example, either disease could manifest as symptoms and signs caused by a mass effect on adjacent vital structures, such as headache, blurred vision and proptosis.
• An extremely rare case of coexisting sinonasal myeloid sarcoma and acute fulminant invasive fungal sinusitis in a relapsed acute myeloid leukaemia patient is presented
• Delayed or missed diagnosis of either condition may be fatal
• The possibility of their coexistence in the sinonasal cavity must be considered in patients with a sinonasal lesion and haematological malignancy
• Timely, appropriate treatment can save lives
The sinus CT may show destruction of surrounding bony structures, including sinuses, lamina papyracea and skull base.Reference Gorman, Ahmed, Pallera and Samant6 Most importantly, endoscopic rhinoscopy reveals gangrenous necrosis of the mucoperiosteum in acute fulminant invasive fungal sinusitis, while a homogeneous, solid sinonasal tumour may be observed in myeloid sarcoma.Reference Jo, Chi and Cho1, Reference Ferri, Minotto, Ianniello, Cavaleri, Armato and Capuzzo3, Reference Prades, Alaani, Mosnier, Dumollard and Martin5, Reference Gorman, Ahmed, Pallera and Samant6, Reference Epstein and Kern8 These endoscopic features are sufficiently distinctive to enable a straightforward diagnosis of acute fulminant invasive fungal sinusitis. Under the circumstances, concomitant myeloid sarcoma could be missed due to masking by the acute fulminant invasive fungal sinusitis. Furthermore, an existing diagnostic label may even hinder the clinician's ability to re-evaluate and reorganise the full spectrum of disease.
In the presented case, the initial diagnosis of acute fulminant invasive fungal sinusitis (as evidenced by the imaging and endoscopic findings) provided a clear explanation for the presenting symptoms and was considered reasonable, as fungal infections are common complications in immunocompromised patients. Delayed diagnosis and treatment of myeloid sarcoma can have fatal consequences. Fortunately, this type of oversight was narrowly avoided in the presented case, through histopathological recognition and prompt treatment of the patient's unusual comorbidity.
Conclusion
The coexistence of myeloid sarcoma and acute fulminant invasive fungal sinusitis in the sinonasal cavity can present a diagnostic dilemma. Timely recognition of this rare comorbid condition is warranted, as application of appropriate treatment can save lives.





