Introduction
Deep neck infections represent life-threatening conditions because of swelling in the upper respiratory tract area and swallowing pathways, and general inflammatory reactions of the organism. Typically, tonsil, salivary gland or tooth infections precede deep neck infections. However, some patients develop deep neck infections without any previous signs of infection. Furthermore, deep neck infections remain serious despite knowledge of pathophysiology and pathways of neck infections. Even the most sophisticated diagnostic tools, broad-spectrum antibiotics and surgical dexterity cannot always prevent serious complications, even death. Therapy usually requires multi-disciplinary co-operation.
Materials and methods
This study aimed to retrospectively evaluate the files of patients who were treated for deep neck infections within the ENT and dental surgery wards of hospitals in Hradec Kralove, Ostrava and Pardubice, over an 11-year period (2002–2012). All patients with fasciitis, or an abscess of deep neck tissue of tonsillar or odontogenic origin, or other aetiologies were considered. Cases of uncomplicated quinsy, lymph node abscess or post-traumatic infection were excluded.
A large number of variables were taken into account; these included demographic data, disease-related symptoms, laboratory indicators of inflammation, co-morbidities, inflammation aetiologies, extent of interfascial inflammation (assessed via imaging), nature of inflammation, microbiological findings, medical and surgical treatments, complications, and treatment outcomes.
The specific variables reviewed, which were limited by the retrospective design and data available, included: time from symptom onset to ward admission, swelling, pain, dysphagia, body temperature, laryngeal and pharyngeal swelling, dyspnoea, neck movement disturbances, trismus, earache, and dysphonia. Levels of inflammatory indicators such as leukocytes, lymphocytes, neutrophils and C-reactive protein (CRP) were also reported. Co-morbidities that could affect disease progress, particularly cardiovascular or lung disease, diabetes mellitus, hepatopathy, haematological diseases, and other serious diseases, were noted. In addition, the results of ultrasound, computed tomography (CT) and nuclear magnetic resonance examinations were reviewed by a radiologist.
Neck spaces are anatomically divided by fasciae, which influence the spreading of infection. For this reason, the extent of inflammation was evaluated based on imaging and clinical examinations. The affected areas were classified into anatomical and clinical regions, as shown in Table I.
Table I Head and neck spaces involved in deep neck infection patients
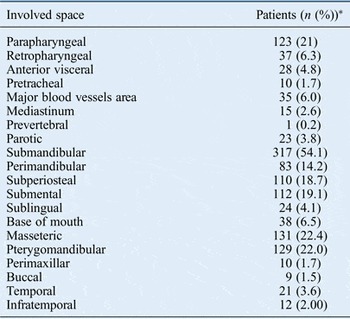
*Total n = 586
Inflammation was categorised based on whether it originated in the tonsils, teeth, major salivary glands or epiglottis. The nature of inflammation was evaluated as either an abscess or fasciitis. Microbiological analysis revealed the bacterial strains.
The treatment of deep neck infections was retrospectively assessed from disease onset to incision, and surgical approaches such as external, transoral or combined, jugular vein ligation, or tonsillectomy were included. Patients were most often treated by oral antibiotics administered prior to hospital admission; these included amoxicillin/clavulanic acid, cephalosporins, aminoglycosides, penicillin, metronidazole and vancomycin.
The incidence of serious complications during the course of the disease were also observed, particularly dyspnoea, sepsis, pneumonia, jugular vein thrombosis, mediastinitis, pleural effusion and disseminated intravascular coagulation (Table II).
Table II Life-threatening complications in deep neck infection patients

*Total n = 586
Data were obtained from all patients; those with missing data (10 per cent) were omitted. Statistical analysis was performed using the analytical software PSPP (version 8.0.4). Descriptive data are presented as numbers and percentages of cases or as medians and ranges of values. Univariate analysis was performed to determine the impact of individual factors on the incidence of life-threatening complications. A multivariate step-wise model was conducted to determinate the influence of the individual factors on each other. Fisher's exact test was used to evaluate statistical significance. These data are presented as odds ratios (with 95 per cent confidence intervals (CIs)).
Results
Demographic and clinical data
In total, 586 persons were considered retrospectively, consisting of 372 (63 per cent) males and 214 (37 per cent) females. The median average age was 40 years (range, 18–90 years). The median average time from symptom onset until admission to the ward was 4 days (range, 1–30 days).
The frequency of each monitored disease symptom was variable, and included: neck swelling (n = 559; 95.4 per cent), pain (n = 571; 97.4 per cent), dysphagia (n = 426; 72.7 per cent), mean body temperature 37.4 °C (range, 36.0–40.0 °C), pharyngeal swelling (n = 154; 26.3 per cent), dyspnoea (n = 33; 5.6 per cent), neck movement disturbance (n = 38; 6.5 per cent), trismus (n = 323; 55.1 per cent), earache (n = 14; 2.4 per cent) and dysphonia (n = 33; 5.6 per cent).
Regarding the laboratory test findings, the median values at the time of admission were: leukocytes = 14.30 × 103/mm3 (range, 1.88–73.90 × 103/mm3), lymphocytes = 1.60 × 103/mm3 (range, 0.20–16.10 × 103/mm3), neutrophils = 11.7 × 103/mm3 (range, 1.00–62.30 × 103/mm3) and CRP = 169.00 mg/dl (range, 6.20–604.00 mg/dl).
Co-morbidities
The co-morbidities that may be related to deep neck infection development were: heart disease (n = 131; 23.4 per cent), pulmonary disease (n = 25; 4.3 per cent), diabetes mellitus (n = 52; 8.9 per cent), hepatopathy (n = 18; 3.0 per cent), haematological diseases (n = 17; 2.9 per cent), and renal failure and other serious diseases (n = 88; 15.0 per cent).
Imaging methods
Only a few patients underwent imaging: 91 (15.5 per cent) had ultrasound scanning, 140 (23.9 per cent) underwent CT and 4 (0.7 per cent) underwent magnetic resonance imaging. Most patients were treated for dental infections primarily by incision and drainage immediately after admission to the hospital, which is why only a small number of patients were scanned.
Regions affected by deep cervical infection and aetiology
A retrospective analysis of the medical records, operational protocols and imaging reports provided information about the neck areas affected by inflammation.
Inflammatory changes involved the following deep neck spaces: parapharyngeal (n = 123; 21 per cent), retropharyngeal (n = 37; 6.3 per cent), anterior visceral (n = 28; 4.8 per cent), pretracheal (n = 10; 1.7 per cent), major blood vessels areas (n = 35; 6.0 per cent), mediastinum (n = 15; 2.6 per cent), prevertebral (n = 1; 0.2 per cent), parotic (n = 23; 3.8 per cent), submandibular (n = 317; 54.1 per cent), perimandibular (n = 83; 14.2 per cent), subperiosteal (n = 110; 18.7 per cent), submental (n = 112; 19.1 per cent), sublingual (n = 24; 4.1 per cent), base of the mouth (n = 38; 6.5 per cent), masseter muscle (n = 131; 22.4 per cent), pterygomandibular (n = 129; 22.0 per cent), parotideomasseteric (n = 29; 5.0 per cent), perimaxillar (n = 10; 1.7 per cent), buccal (n = 9; 1.5 per cent), temporal (n = 21; 3.6 per cent) and infratemporal (n = 12; 2.00 per cent) (Table I).
The origins of the infections were located within: the tonsils (n = 31; 5.29 per cent), teeth (n = 485; 82.8 per cent), major salivary glands (n = 12; 1.1 per cent) and epiglottis (n = 3; 0.5 per cent). The analysis failed to find origins in the other cases.
Microbiology
The identified microbes and percentage occurrences are shown in Table III.
Table III Microbial strains isolated from deep neck infection patients

*Total n = 586
Treatment
Antibiotic treatment was commenced in all cases as monotherapy or combination therapy. The antibiotics used were as follows: amoxicillin/clavulanic acid (n = 361; 61.60 per cent), cephalosporins (n = 60; 10.24 per cent), penicillin (n = 27; 4.61 per cent), aminoglycosides (n = 46; 7.85 per cent), metronidazole (n = 54; 9.22 per cent), vancomycin (n = 13; 2.22 per cent) and others (n = 230; 39.25 per cent).
All patients included in the study were treated surgically. However, the extent of the surgery was considered on an individual basis. The median time from hospital admission until incision was 1 day (range, 0–10 days). Surgical approaches were as follows: external (n = 500; 85.32 per cent), transoral (n = 111; 18.94 per cent), combined (n = 22; 3.75 per cent), internal jugular vein ligation (n = 4; 0.68 per cent), tonsillectomy (n = 16; 2.73 per cent), and other treatments including tooth extraction, abscess puncture and tracheostomy (n = 224; 38.23 per cent).
Complications
Important factors considered by the authors to be life-threatening were observed during the course of hospital stay. Life-threatening complications affected a total of 60 patients (10.2 per cent). Complications included dyspnoea (n = 13; 2.22 per cent), sepsis (n = 15; 2.56 per cent), mediastinitis (n = 16; 2.73 per cent), pneumonia (n = 7; 1.19 per cent), internal jugular vein thrombosis (n = 4, 0.68 per cent), pleural effusion (n = 2; 0.34 per cent) and death (n = 3; 0.51 per cent) (Table II).
Predictors of complications
Univariate logistical regression analysis was focused on factors associated with life-threatening complications. In this simple model, single variables were tested. Odds ratios (with 95 per cent CIs) were calculated to represent the probability that the complication will occur. All factors were statistically tested with a clear target, to reveal those with an odds ratio of more than 1 and statistically significant (p < 0.05).
Life-threatening complications were more likely to occur in patients with the following symptoms: pharyngeal swelling (odds ratio = 2.88 (95 per cent CI = 1.47–5.64); p = 0.003), dyspnoea (10.13 (4.45–23.10); p < 0.001), neck movement disturbance (18.25 (8.39–39.73); p < 0.001) and dysphonia (14.33 (6.38–32.18); p < 0.001). Co-morbidities that could affect disease progress were: cardiovascular illnesses (2.39 (1.20–4.74); p = 0.015) and pulmonary disease (5.40 (2.01–14.48); p = 0.003). The incidence of life-threatening complications was associated with involvement of the following anatomical locations: parapharyngeal (5.75 (2.90–11.41); p < 0.001), anterior visceral (7.30 (2.96–17.97); p < 0.001), pretracheal (10.97 (2.95–40.78) (p = 0.002), temporal (6.89 (2.50–18.99); p = 0.001) and parotic (3.38 (1.09–10.51); p = 0.050). The tonsils as the origin of infection were a unique predictor of complications (6.31 (2.60–15.32); p < 0.001), and complications were more likely in patients with fasciitis (8.30 (3.80–18.12); p < 0.001). The presence of fungal infections, especially Candida albicans (14.15 (5.76–34.77); p < 0.001), was a significant predictor of complications. From these findings, it is clear that the factors associated with the incidence of life-threatening complications are numerous, as illustrated in Table IV.
Table IV Statistically significant univariate model predictors of life-threatening complications*

* In deep neck infection patients. CI = confidence interval
In order to evaluate the strength of the individual factors identified, we used the multivariate step-wise model, which takes into account the influence of the individual variables on each other. The number of significant factors was considerably reduced, and included: involvement of the retropharyngeal space (odds ratio = 3.46 (95 per cent CI = 1.47–8.14); p = 0.005) and major blood vessels area (3.71 (1.45– 9.50); p = 0.006), and the presence of C albicans in cultures (13.32 (4.68–37.90); p < 0.001).
Discussion
The male-to-female ratio of 2:1 and the median age of 40 years correspond to the published figures.Reference Boscolo-Rizzo, Stellin, Muzzi, Mantovani, Fuson and Lupato 1 , Reference Matzelle, Heard, Khong, Riley and Eakins 2 The reason for the higher incidence in males is unclear. Patients aged less than 18 years were excluded because the majority suffered from a lymph node abscess. However, deep cervical infections have been documented in children (79 patients with an average age of 7.3 years), most of whom were toddlers.Reference Raffaldi, Scolfaro, Garazzino, Peradotto, Calitri and Tovo 3 , Reference Garca, Budak, Demir, Cankaya and Kiroglu 4
Co-morbidities play a considerable role in deep neck infection development because of their negative effect on the immune system. In a retrospective analysis of 439 deep neck infection patients with a CRP level higher than 100 mg/l, the presence of co-morbidities was considered predictive of life-threatening complications.Reference Wang, Tai, Kuo and Chien 5 A meta-analysis of 20 studies revealed that diabetics with a deep neck infection more often had multi-space involvement, frequently associated with Klebsiella pneumoniae and less with streptococcus and anaerobes.Reference Hidaka, Yamaguchi, Hasegawa, Yano, Kakuta and Ozawa 6 This was confirmed by Huang et al., who also described a higher incidence of K pneumoniae in diabetics.Reference Huang, Tseng, Yeh, Hsu and Chen 7 Diabetes itself is usually considered to be a crucial factor in the development of life-threatening complications;Reference Hasegawa, Hidaka, Tateda, Kudo, Sagai and Miyazaki 8 however, diabetes was not a significant predictive factor of life-threatening complications in our study. Interestingly, we found that the incidence of C albicans was significantly higher in diabetics than non-diabetics.
Imaging methods can distinguish the nature and the extent of the infection. Ultrasound is a superior method for the investigation of superficially located lesions. Experienced radiologists can differentiate between an abscess or cellulitis; moreover, they can exclude or confirm vein thrombosis.Reference Maroldi, Farina, Ravanelli, Lombardi and Nicolai 9 , Reference Hegde, Mohan, Pandya and Shah 10 Computed tomography is the appropriate examination for further localised lesions and is sometimes considered compulsory for the evaluation of deep neck infections.Reference Wang, Gao, Xu and Xiang 11 Computed tomography is suitable for assessing the resolution of cellulitis or an abscess in the retropharyngeal area, an area highlighted in our study as a significant predictor of complications. However, this represents only 50 per cent of the positive predictive value of CT scans.Reference Chuang, Lin, Wen and Hsu 12 Magnetic resonance imaging is used in adults in exceptional circumstances.Reference Maroldi, Farina, Ravanelli, Lombardi and Nicolai 9 Surprisingly, only a relatively small number of patients in our sample underwent imaging. This is because a significant proportion of patients (n = 485; 82.8 per cent) were treated by dental surgeons via incision of the affected area, without any imaging. The perspective differs significantly between dental surgeons and ENT specialists. Imaging should always be carried out if there is any suspicion of the spread of infection towards other areas.
Deep neck infection regions and aetiology
Infections usually tend to follow anatomical borders and they have the tendency to firstly involve one interfascial compartment before they spread into another. The higher occurrence of deep neck infections in perimandibular spaces reflects the spectrum of patients with a dental origin of infection (n = 485; 82.2 per cent). Dental causes are often reported as the main reason of deep neck infections in adults;Reference Wang, Tai, Kuo and Chien 5 lymphadenopathy and tonsillar infections are more common in paediatric patients. If the infection involves perimandibular spaces, it remarkably tends to propagate horizontally, which is due to the horizontal-shaped anatomy of perimandibular fascial spaces. In contrast, areas with a tendency to propagate vertically are dangerous from the viewpoint of life-threatening complications.Reference Maroldi, Farina, Ravanelli, Lombardi and Nicolai 9 Indeed, our study highlights the involvement of spaces with possible vertical spread as a predictor of life-threatening complications.
Bacteriological findings
Pharyngeal and dental infections are usually caused by different bacterial strains; however, bacterial cultures of deep neck infections of both origins are not considerably different. Bacteriological investigations revealed that the most common bacterial strain was Streptococcus viridans (n = 170; 29.0 per cent), followed by Micromonas micros (peptostreptococcus) (n = 165; 28.2 per cent). These findings are similar to those of Huang et al.Reference Huang, Tseng, Yeh, Hsu and Chen 7 In that study, S viridans was the most commonly isolated organism (38.3 per cent), followed by K pneumoniae (32.0 per cent) and peptostreptococcus (17.2 per cent).Reference Huang, Tseng, Yeh, Hsu and Chen 7 Surprisingly, K pneumoniae was found in only a few cases (1.2 per cent) in our study.
Treatment findings
Both surgical and conservative treatments should be considered in deep neck infections. A high dosage intravenous empirical antibiotic with a broad antibacterial spectrum is usually the first step of treatment. More focused antibiotic treatment can be used once the results of microbiological cultivations are apparent.Reference Boscolo-Rizzo, Stellin, Muzzi, Mantovani, Fuson and Lupato 1 Surgical therapy (in the proof of an abscess) is considered the ‘gold standard’ of treatment.Reference Boscolo-Rizzo, Stellin, Muzzi, Mantovani, Fuson and Lupato 1 Moreover, the treatment provided by an experienced physician usually has better results than that provided by less experienced specialists. All patients who were treated surgically were operated on by an experienced surgeon, as required by the national health services’ policy.
Univariate and multivariate statistical models
Different types of statistical modelling are widely used in large medical studies to discover the predictors, strengths and trends of pathologies. A multivariate model was previously used to identify factors associated with the duration of hospital stay and consequently with serious complications in 282 cases of deep neck infections.Reference Staffieri, Fasanaro, Favaretto, Torre, Sanguin and Giacomelli 13 In that model, the only predictor of complications was multi-space involvement. Other factors such as leukocytosis (white cell counts over 11 × 109/l), co-morbidities or the need for surgical intervention should only affect the length of hospitalisation.Reference Staffieri, Fasanaro, Favaretto, Torre, Sanguin and Giacomelli 13 In our study, the most important predictors of impending complications appeared to be the localisation of inflammation in the retropharyngeal space and large blood vessels area, and the presence of C albicans (Table V).
-
• A retrospective multi-institutional analysis of 586 deep neck infection patients was conducted
-
• Various factors and statistical models were used to ascertain the most influential prognostic factors for the occurrence of life-threatening complications
-
• Retropharyngeal space and major blood vessels area involvement, and C albicans in cultures, are significant risk factors for life-threatening complications
Table V Statistically significant multivariate model predictors of life-threatening complications*

* In deep neck infection patients. CI = confidence interval
The sheets of deep fascia of the neck are organised so that between the middle and the profound layer of the deep cervical fascia is an alar sheet of deep fascia. Thus, the whole area is divided into three subspaces. The retropharyngeal space originates below the skull base and finishes in the level of the 1st to 2nd thoracic vertebrae (danger space), ending caudally on the diaphragm and prevertebral space, which runs along the entire spine. The major cervical vessels space is caudally opened towards the middle mediastinum, which again contributes to the spread of inflammation. The space along the major vessels in the neck is also called the Lincoln highway. These ideas are in accord with the observation of mediastinal spread of retrotonsillar and retropharyngeal infections.Reference Hasegawa, Hidaka, Tateda, Kudo, Sagai and Miyazaki 8
Conclusion
Even in this time of modern antibiotics, and advanced imaging and laboratory methods, the treatment of deep neck infections remains a considerable challenge. Increased attention should be given to all patients with deep neck infections, as the course and outcome of deep neck infections are unpredictable. Nevertheless, on the basis of our results, it can be predicted that patients with neck mobility disturbances, dysphonia, shortness of breath, external neck swelling with severe pain, and inflammatory changes in the large vessels area and retropharyngeal space, are likely to develop life-threatening complications. Such complications are more likely when the bacterial culture C albicans is cultivated. In these patients, the timely initiation of combined intravenous antibiotic therapy and possible need of surgical intervention should be considered.







