Introduction
Branchial cleft cyst is derived from the remnants of the branchial apparatus. Histologically, this lesion shows a stratified squamous or columnar ciliated epithelial lining together with lymphoid aggregation in the subepithelial connective tissue.Reference Chen, Su, Lin and Hwang1
Nasopharyngeal branchial cleft cyst is an extremely rare type of branchial cleft cystic anomaly. It originates from the lateral nasopharynx and presents as a single, unilateral mass. In some cases, this lesion can extend inferiorly and medially into the lateral oropharynx to produce obstructive symptoms.
The generally accepted treatment of nasopharyngeal branchial cleft cyst is complete surgical excision.Reference Choo, Kim and Jin2–Reference Marom, Russo, Ben Salem and Roth4 However, a recent report described four cases of nasopharyngeal branchial cleft cyst treated with transoral laser marsupialisation.Reference Tsai and Su5
Herein, we report the use of a powered instrument to achieve marsupialisation in two cases of nasopharyngeal branchial cleft cyst, with successful outcomes and no complications.
Case reports
Case one
A two-year-old boy was admitted to hospital. His parents were worried about his severe snoring and sleep apnoea.
Upon physical examination, a snoring sound was audible even in the sitting position. An oropharyngeal cystic mass was visible.
Magnetic resonance imaging (MRI) was performed. Both T1- and T2-weighted scans demonstrated a well defined, hyperintense, non-enhancing, 1.8 × 1.2 × 2.5 cm, cystic mass in the right nasopharynx (Figure 1).

Fig. 1 Magnetic resonance imaging scans of case one: (a) axial, T1-weighted scan, and (b) coronal, T2-weighted scan, both showing a hyperintense, cystic mass. The arrow indicates the 1.8 × 1.2 × 2.5 cm, right nasopharyngeal cyst, which extends from the right nasopharyngeal wall down to the oropharynx.
Polysomnography was discussed in order to investigate the child's snoring and apnoea, but his mother refused.
We planned a transoral nasopharyngeal branchial cleft cyst marsupialisation procedure together with tonsillectomy and adenoidectomy. Under general anaesthesia, a cystic, oropharyngeal mass was observed upon endoscopic examination (Figure 2a). First, the cyst wall was biopsied; this released gushing, brownish-green, seromucinous cyst fluid, which was suctioned away (Figure 2b). The cyst wall was then shaved using a powered instrument (Xomed M4 microdebrider; Medtronic, Minneapolis, Minnesota, USA) (Figure 2c). Tonsillectomy and adenoidectomy were performed.
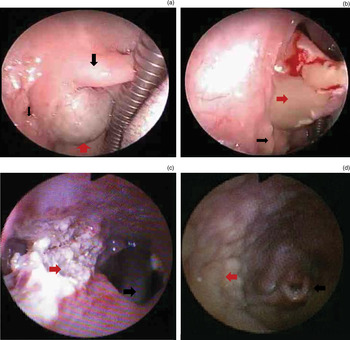
Fig. 2 (a)–(c) Intra-operative endoscopic views showing local findings for the first case of nasopharyngeal branchial cleft cyst. (a) Oral presentation (red arrow = cystic mass; wide black arrow = uvula; narrow black arrow = right tonsil). (b) Cyst wall biopsy results in cyst wall rupture, releasing gushing, brownish-green, seromucinous fluid (red arrow = cystic fluid; black arrow = right tonsil). (c) Fibre-optic nasopharyngeal view on completion of surgery (red arrow = operation site; black arrow = orotracheal intubation tube). (d) Right fibre-optic nasolaryngeal view at 21-month post-operative follow up (red arrow = operation site; black arrow = epiglottis).
The child's snoring disappeared immediately after surgery. There was no evidence of recurrence over 21 months of follow up (Figure 2d).
Histopathological examination of the biopsy specimen revealed a squamous epithelium lined cyst with lymphoid aggregation, consistent with a branchial cleft cyst.
Case two
A 56-year-old man with right nasal obstruction accompanied by a sensation of fullness in the right ear presented to a tertiary hospital.
Nasendoscopic examination showed a well circumscribed, cystic mass in the right nasopharynx (Figure 3a). The mass was covered with a mucous membrane and was attached to the posterolateral aspect of the right nasopharynx.
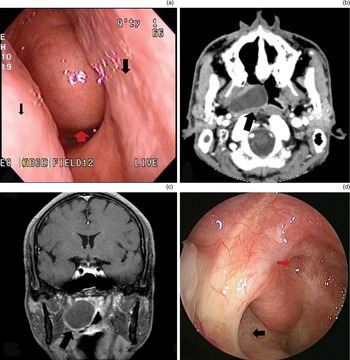
Fig. 3 Findings for case two. (a) Pre-operative endoscopic view (red arrow = cystic mass; wide black arrow = septum; narrow black arrow = right inferior turbinate). (b) Pre-operative, axial computed tomography scan with rim enhancement (arrow = right nasopharyngeal cyst). (c) Pre-operative, coronal, T1-weighted magnetic resonance imaging scan showing a hypointense, cystic, 2 × 4 × 4 cm mass with gadolinium rim enhancement (arrow = right nasopharyngeal cyst). (d) Endoscopic view of right nasopharynx at two-year follow up (red arrow = marsupialisation opening site; black arrow = right eustachian tube orifice).
Magnetic resonance imaging revealed an apparently benign, cystic, 2 × 4 × 4 cm mass with no enhancement of its solid portion, which obliterated the fossa of Rossenmuller in the right nasopharynx (Figure 3b and 3c). The MRI also showed right otomastoiditis and mild sinusitis in the right fronto-ethmoid sinuses. In addition, a right middle-ear effusion was observed.
Tympanometry showed a flat, type B pattern.
Under general anaesthesia, the cystic mass was marsupialised using a powered instrument (Xomed M4 microdebrider) via a transnasal endoscopic approach. A ventilation tube was inserted into the right tympanic membrane under microscopic guidance.
Histopathological examination revealed a lympho-epithelial cyst consistent with a branchial cleft anomaly.
There was no recurrence after two years of follow up (Figure 3d).
Discussion
Branchial cleft cysts comprise the majority of branchial cleft anomalies. These cysts are usually found during the second, third or fourth decade of life. They are located in the upper third of the neck, just below the mandible and anterior to the sternocleidomastoid muscle.Reference Tsai and Su5 Second branchial cleft cysts are the most common type of branchial anomalies, classically located along the anterior border of the sternocleidomastoid muscle with a sinus tract to the oropharynx. However, they can also be found in the parapharyngeal space or the nasopharynx itself, without any connection to the palatine tonsillar fossae. Papay et al. reported a case of nasopharyngeal branchial cleft cyst and stated that this lesion arises most commonly from the lateral extension of the second branchial apparatus.Reference Papay, Kalucis, Eliachar and Tucker6
The differential diagnosis of nasopharyngeal masses include Rathke's pouch, adenoid and tonsillar mucous retention cysts, nasopharyngeal branchial cleft cyst, Thornwaldt's cyst, dermoid cyst, chordoma, herniation of the central nervous system, and sphenoid sinus mucocele.Reference Chen, Su and Hao3 Differentiation between Thornwaldt's cyst and nasopharyngeal branchial cleft cyst is based on anatomical location: Thornwaldt's cysts are usually located in the midline whereas nasopharyngeal branchial cleft cysts lie more laterally, close to the eustachian tube orifice.Reference Shank, Burgess and Geyer7 Our two cases originated in the vicinity of the eustachian tube, at the lateral nasopharyngeal wall.
Histological examination of nasopharyngeal branchial cleft cyst reveals stratified squamous or ciliated columnar epithelium with abundant lymphoid tissue often with germinal centres in the connective tissue. The cystic contents may be clear, mucinous or seromucinous fluid. In contrast, histological examination of Thornwaldt's cyst shows an epithelium-lined cyst with no surrounding lymphoid tissue. A histopathological study of tonsillar and adenoid retention cysts reported the absence of an epithelium-lined cyst wall.Reference Shank, Burgess and Geyer7 In our two cases, histological examination revealed a true, epithelium-lined cyst with surrounding lymphoid aggregates.
• Nasopharyngeal branchial cleft cyst is extremely rare
• Total excision is time-consuming and risks incomplete excision and neurovascular injury
• Powered instrument marsupialisation is simple, effective and less invasive
The recommended treatment for nasopharyngeal branchial cleft cyst is complete surgical excision.Reference Choo, Kim and Jin2–Reference Marom, Russo, Ben Salem and Roth4 Several completely excisional approaches have been described, including transoral, transpalatal, transmandibular and transcervical routes. The transoral approach is a less invasive technique, but great care should be taken during total excision of the nasopharyngeal branchial cleft cyst because of the risk of neurovascular injury.Reference Tsai and Su5 The transpalatal, transmandibular and transcervical approaches enable extensive exposure of the oropharynx and nasopharynx, but they have many serious potential complications such as velopharyngeal insufficiency, cosmetic deformity and external scarring. Also, total excision is time-consuming and carries the risk of incomplete excision and neurovascular damage.Reference Tsai and Su5 Recently, Tsai and Su reported transoral laser marsupialisation followed by cut edge lining and oropharyngeal mucosal suture.Reference Tsai and Su5 They reported that the technique was safer, less invasive and faster, with no recurrence.
In our first case, transoral powered instrument marsupialisation was easily performed under mirror and endoscopic visualisation. There were no serious complications (e.g. velopharyngeal insufficiency or neurovascular injury). In our second case, transnasal microdebrider marsupialisation was performed under endoscopic visualisation. There were no complications. Operator attention was focused on removing as much of the cyst as possible and creating an unclosed opening. Care was necessary because, after sucking out the cystic fluid, the cyst wall was so thin that punch biopsy, small marsupialisation or penetration could have caused it to collapse. However, towards completion of the shaving procedure, the origin of the nasopharyngeal branchial cleft cyst seemed not to collapse so easily. This may have been due to an adhesion between the nasopharyngeal branchial cleft cyst and the nasopharyngeal wall mucosa, or to invagination of the original branchial pouch in the nasopharyngeal wall.
For nasolabial cysts, surgical removal via a sublabial approach has been the standard choice of treatment. Recently, several reports have proposed that transnasal marsupialisation of nasolabial cyst by microdebrider has safe and effective results.Reference Chen, Su, Lin and Hwang1, Reference Lee, Baek, Byun, Chang, Lee and Kim8 Retrospective and prospective studies comparing the sublabial approach versus transnasal microdebrider-assisted marsupialisation have reported no recurrence, or other post-operative complications, following transnasal powered instrument assisted marsupialisation.Reference Chen, Su, Lin and Hwang1, Reference Lee, Baek, Byun, Chang, Lee and Kim8 However, differences in marsupialisation technique have been noted between nasolabial and nasopharyngeal branchial cleft cysts. In the case of nasolabial cysts, it is not necessary to remove almost all the cystic wall in order to make an unclosed opening, because of the resistance of the cyst wall to collapse. In the case of nasopharyngeal branchial cleft cysts, however, we believe the surgeon should remove as much of the cyst wall as possible, using a microdebrider, in order to make an unclosed opening.
Our two cases had no recurrence following powered instrument assisted marsupialisation (via a transoral approach in one patient and a transnasal approach in the other). This result is consistent with the view that powered instrument assisted transoral or transnasal marsupialisation is the endoscopic surgical technique of choice in order to prevent recurrence.
One limitation of our study was the fact that nasopharyngeal branchial cleft cyst is extremely rare; as a result, there were only two cases in our report. Analysis of more cases with long-term follow up would be needed in order to substantiate our approach.
Conclusion
Powered instrument marsupialisation is a simple, effective and less invasive technique for the treatment of nasopharyngeal branchial cleft cyst. However, the surgeon must pay careful attention to remove as much of the cyst as possible, by making an unclosed opening during powered instrument marsupialisation.





