Introduction
Tympanic membrane perforation is a condition frequently faced by otolaryngologists. Chronic otitis media is the commonest cause.Reference Kawatra, Maheshwari and Kumar1 Perforation leads to varying degrees of conductive hearing loss and discharging ear with increased potential of middle-ear cleft infection. The requirement for frequent visits to hospital poses psychosocial and financial burdens on society. This makes it necessary to diagnose and treat tympanic membrane perforation as early as possible.Reference Pannu, Chadha and Kumar2
Effective management is expedient while prevention and reduction of complications must be given utmost attention to achieve good outcomes. The first recorded attempt at repairing the tympanic membrane was made by Marcus Banzer in 1640 using an ivory tube covered by pig's bladder,Reference Mudry3 whereas the first true tympanoplasty is said to have been performed by Emil Berthold in 1878 and was later popularised and developed by Wullstein and Zollner.Reference Berthold4–Reference Zollner6
It has been reported in the literature that various techniques are employed, depending on the site and size of the perforation. The results of tympanoplasty in terms of graft uptake rates vary between 74 and 97 per cent.Reference Palva and Ramsay7 Otologists have refined various tympanoplasty techniques to achieve better results, including underlay tympanoplasty which is the most widely used technique.Reference Sarkar8 In underlay tympanoplasty, it is not uncommon for the mucous membrane to form the whole (or part) of the lateral surface of drumhead (this is called mucosalisation of the graft). In such cases, in spite of graft uptake, the surface of the drumhead leads to continuous or intermittent oozing as seen in recurrent myringitis.
Total annulus excision is part of a broader technique of grafting the tympanic membrane called interlay tympanoplasty. The main advantage of the interlay technique is that once the graft is placed between middle-ear mucosa and canal skin, there will be no mucous membrane left lateral to the graft and no epithelium medial to the graft, therefore reducing the risk of lateral neotympanum mucosalisation. Another benefit is neovascularisation around the graft. Total annulus excision is an emerging technique and represents a revolutionary change in the history of tympanoplasty as it gives a three-layered tympanic membrane that is physiologically and anatomically as natural as currently possible.
The present study was conducted to find out whether total annulus excision or conventional tympanoplasty is the better surgical technique in cases of inactive mucosal chronic otitis media.
Materials and methods
Study design and protocol
The Institutional Research and Review Board of SMS Medical College, Jaipur, India, granted approval for this study. This study was a hospital-based, double blind, randomised controlled interventional study that took place in the Department of Otorhinolaryngology, SMS Medical College and Attached Hospitals, from April 2017 to December 2018.
Inclusion criteria were: age between 15 and 55 years, patients diagnosed with inactive mucosal type of chronic otitis media with conductive hearing loss and pars tensa perforation, patients fit for surgery, and patients who gave a written consent for inclusion in the study.
Exclusion criteria were: age below 15 years and above 55 years, squamous type or active mucosal type disease, tympanosclerosis, history of previous ear surgery, patients with mixed or sensorineural hearing loss, ossicular chain fixation or disruption and patients in whom ossicular chain status could not be assessed.
As total annulus excision is an uncommon type of tympanoplasty, only 28 cases were enrolled in each group to assess results without causing significant complications.
Patient allocation and randomisation
All patients had a detailed history taken, a thorough clinical examination of the ear, nose and throat, pure tone audiometry testing and routine blood investigations. After written consent was obtained, the patients were randomised into one of the two study groups using a formal computer randomisation protocol (www.random.org/integers).
Patients in group A underwent conventional tympanoplasty and patients in group B underwent total annulus excision tympanoplasty. Patients and evaluators were blind to the procedure performed. In all patients, tympanoplasty was performed through a postauricular approach and temporalis fascia graft was used. All procedures were performed by a single senior author (PS).
Total annulus excision tympanoplasty technique
The approach is the standard postauricular approach via the Korner's flap (this description of technique is for the right ear). The tympanomeatal flap is raised with a flag knife from 12 o'clock to 7 o'clock until the fibrous annulus is reached. Note that the perforation and its margins are not ‘freshened’ or dealt with (in any manner at any stage). Next, the bone of the scutum is removed with a House curette in a small arc from the posterior aspect of the Notch of Rivinus to the area just superior to the entry of the chorda tympani nerve into the middle ear (Figure 1). This will immediately afford a direct view of long process of incus and stapes (and any defect or pathology therein). Next, the chorda tympani nerve is gently separated from the flap and the posterior fibrous annulus is lifted off its groove until the 5 o'clock position.

Fig. 1. Minimal curettage of postero-superior bone to visualise the ossicles after elevation of posterior tympanomeatal flap (right ear).
The next step involves detachment of the drumhead along the entire length of the handle of malleus and from the mucosal bubble of the Notch of Rivinus. This manoeuvre involves the incision of the periosteum down to the bone of the malleus with a very sharp and angled instrument (our instrument is called the ‘cobra’) to lift off the entire periosteal cuff (Figure 2). This leads to complete detachment of the tympanic flap along with perforation from the handle of the malleus; the success of this manoeuvre is indicated by the fact that the lateral surface of the tympanic flap and the perforation remains completely undisturbed.
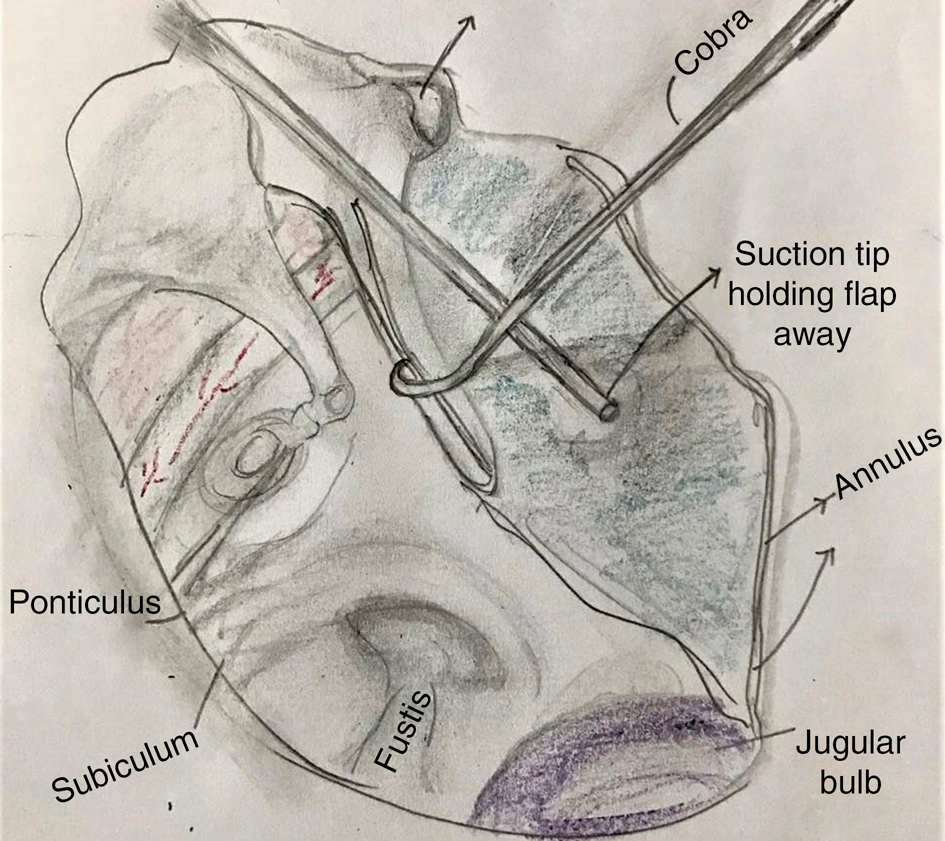
Fig. 2. Removal of entire periosteal cuff from the handle of malleus (right ear).
Now a pair of reciprocating micro-scissors is used to cut the tympanic flap through from the lateral to medial part and into the perforation dividing it in superior and inferior flaps (Figure 3). Now the inferior flap is retracted with the suction canula, and the fibrous annulus is levered out of its bony groove until antero-superiorly freeing the entire flap from the bony sulcus. In the next step, retrograde elevation (medial to lateral) of the anterior tympanic flap is instituted for about 4 mm until it matches the width of the posterior flap.

Fig. 3. Cutting the posterior canal skin laterally to medially until the perforation to make superior and inferior flaps (right ear).
The next step of total annular excision is the essence of this whole process. The same pair of reciprocating micro-scissors are used to start the cut on the tympanic flap lateral to the fibrous annulus on both superior and inferior flaps, all the time staying lateral to the annulus (Figure 4), resulting in removal of the total annulus excision specimen from the field. We are left with a 3 mm cuff of elevated deep meatal skin. The middle-ear field is now completely open, and ossiculoplasty or reconstruction of the hearing mechanism is performed if required. Next we harvest the temporalis fascia graft.

Fig. 4. Cutting the superior and inferior tympanomeatal flaps just lateral to fibrous annulus circumferentially (right ear).
The last step is to lay the graft with the handle of malleus lateral to the graft (if the malleus handle is present). The lateral circumference of the graft is allowed to be trapped between canal bone and the 3 mm cuff of deep meatal skin around the entire circumference (Figure 5). Gel foam is not used medial to graft in our technique.

Fig. 5. Tucking the graft under the medial part of canal skin all around (right ear).
Outcome measures
The outcome measures among both groups in the study were as follows: (1) graft take up, (2) post-operative ear discharge, and (3) hearing gain in terms of air–bone gap, air conduction and bone conduction thresholds, which were compared at the sixth month by pure tone audiometry.
Statistical analysis
Continuous variables were summarised as mean and standard deviation and were analysed by using the unpaired t-test. Nominal or categorical variables were expressed as proportions (per cent) and were analysed by using chi-square and Fisher's exact test. A p-value less than 0.05 was taken as significant. MDCalc (version 16.4) statistical calculation software was used for all statistical calculations.
Results
Study population
A total of 56 patients with chronic otitis media were enrolled for the study. They were randomised and categorised into 2 groups with 28 cases in each group. Group A included patients who underwent conventional tympanoplasty, and group B included patients who underwent total annular excision tympanoplasty.
The age of cases ranged between 15 and 55 years with a mean of 26.46 years in group A and 27.11 years in group B. There were 30.36 per cent male and 69.64 per cent female patients, showing female preponderance. The left ear was operated on in 34 patients (60.17 per cent), and the right ear was operated on in the remaining 22 patients (39.28 per cent). Table 1 shows patient demographic data.
Table 1. Patient demographic data

SD = standard deviation
Outcome analysis
The pre-operative mean (± standard deviation) air conduction in group A (conventional tympanoplasty) was 40.72 ± 8.72 dB and in group B (total annulus excision) was 42.11 ± 8.24 dB (p > 0.05). Pre-operative mean bone conduction in group A (conventional tympanoplasty) was 13.27 ± 4.35 dB and in group B (total annulus excision) was 14.38 ± 5.65 dB (p > 0.05). Pre-operative mean air–bone gap in group A (conventional tympanoplasty) was 27.56 ± 7.39 dB and in group B (total annulus excision) was 27.73 ± 6.59 dB (p > 0.05).
The post-operative graft uptake was seen in all 28 patients who underwent total annulus excision tympanoplasty and in 27 patients who underwent conventional tympanoplasty with residual perforation in one patient at the post-operative sixth month. Post-operative discharge was seen in 14.29 per cent of patients who underwent conventional tympanoplasty, and no discharge was seen in patients who underwent total annular excision tympanoplasty (Table 2).
Table 2. Comparison of post-operative clinical findings

Group B (total annulus excision) had better post-operative mean air conduction thresholds (22.09 ± 4.33 dB) than group A (conventional tympanoplasty) (24.68 ± 3.90 dB; p < 0.05) at the post-operative 6th month. Mean improvement of air conduction in group A (conventional tympanoplasty) was 16.04 ± 7.27 dB and for group B (total annulus excision) was 20.02 ± 9.14 dB. Mean bone conduction at the post-operative 6th month in group A (conventional tympanoplasty) was 11.24 ± 4.30 dB and in group B (total annulus excision) was 10.14 ± 3.72 dB. Mean improvement of bone conduction in group A (conventional tympanoplasty) was 2.03 ± 5.98 dB, comparable to group B (total annulus excision) which was 4.24 ± 6.88 dB (p > 0.05).
Mean air–bone gap at the post-operative 6th month in group A (conventional tympanoplasty) was 13.44 ± 3.27 dB and was 12.31 ± 3.68 dB in group B (total annulus excision). Mean improvement in air–bone gap in group A (conventional tympanoplasty) was 14.12 ± 7.50 dB and in group B (total annulus excision) was 15.43 ± 6.52 dB. Comparison of hearing status among groups is mentioned in Figure 6.

Fig. 6. Comparison of hearing between two groups. AC = air conduction; BC = bone conduction; ABG = air–bone gap.
Discussion
Chronic otitis media is one of the most common causes of preventable hearing loss, particularly in developing countries like India (which, according to the World Health Organization, is among the nations with the highest burden). It requires tympanoplasty for its correction.9
Since it was first introduced in the early 1950s, tympanoplasty has come a long wayReference Primrose and Kerr10 as there is a constant desire to improve technique and outcomes. Total annulus excision tympanoplasty is a type of interlay technique of tympanoplasty that has good results because of its low incidence of complications and promising hearing improvement. The most superior result is a new ear drum which is as close (in appearance and function) to the normal eardrum without disease as is currently possible.
The process of epithelisation and mucosalisation of margins of perforation in the settings of chronic otitis media is well known. Mucosalisation of the annulus and the graft leads to a continuously discharging ear even after successful graft uptake because of presence of mucous secreting glands on the lateral aspect of the graft. In addition, the annulus cannot be snugly fitted into the sulcus tympanicus after conventional tympanoplasty, resulting in less improvement in hearing.
• Often the mucous membrane forms the whole (or part) of the lateral surface of the drumhead in conventional underlay tympanoplasty
• Total annulus excision is an interlay type of tympanoplasty where graft is kept between mucosa medially and canal skin epithelium laterally after removal of residual tympanic membrane with its annulus
• Total annulus excision has a high success rate for hearing improvement, graft uptake and no discharge through neotympanum post-operatively
• Total annulus excision can be preferable over conventional underlay technique
Even after successful tympanoplasty with the underlay technique, intratympanic cholesteatoma may develop between the layers of the tympanic membrane.Reference Patil, Misale, Mane and Mohite11 Therefore, total annulus excision limits the risk associated with conventional tympanoplasty. It also provides better hearing results than conventional tympanoplasty. Excision of the annulus also ensures rich neovascularisation around the graft. The neo-annulus is kept in its original place to prevent anterior angle blunting. This technique is preferred by us because it has many advantages, such as no risk of blunting, lateralisation of graft and epithelial cyst formation.
In the present study, we observed that the take up rate of graft occurred in all 28 cases in group B (total annulus excision) whereas it occurred in 27 cases (96.43 per cent) in group A (conventional tympanoplasty). A study done by Patil et al. on the outcome of interlay grafting in type 1 tympanoplasty had a graft success rate of 96 per cent. The study was done on 100 cases with residual perforation in 4 per cent of cases.Reference Patil, Misale, Mane and Mohite11 Graft uptake rate in interlay tympanoplasty was 96.6 per cent in a study reported by Jain et al.Reference Jain, Gupta, Gupta and Roy12 while a study performed by Sharma et al. reported a graft uptake rate of 90 per cent in underlay type 1 tympanoplasty and 96 per cent in interlay type 1 tympanoplasty.Reference Sharma, Sharma, Goyal and Sharma13 In a study by Singh et al., 30 cases were performed using overlay and 30 cases by underlay technique, and graft uptake rate was 93.3 per cent in both the groups.Reference Singh, Rai, Bandyopadhyay and Gupta14 In a study of overlay versus underlay tympanoplasty outcomes by Sergi et al., the graft uptake rate was 94.2 per cent by underlay technique and 91.5 per cent by overlay.Reference Sergi, Galli, De Corso, Parrilla and Paludetti15 Similarly, the outcome in terms of graft uptake rate was slightly better for the underlay technique (91.43 per cent) when compared with the overlay technique (89.18 per cent) in the study reported by Kalsotra et al.Reference Kalsotra, Gupta, Gupta, Kotwal, Suri and Kanotra16
The result of graft success rate in our study by total annulus excision tympanoplasty was 100 per cent, which was better than all other techniques of tympanoplasty in the studies reported above. Our results of conventional tympanoplasty (96.43 per cent) were also slightly better than Singh et al., Sergi et al. and Kalsotra et al., who reported graft success rates of 93.3 per cent, 94.2 per cent and 91.43 per cent, respectively;Reference Singh, Rai, Bandyopadhyay and Gupta14–Reference Kalsotra, Gupta, Gupta, Kotwal, Suri and Kanotra16 although they were not statistically significant, this might be due to the small sample size. No discharge was observed post-operatively in the total annulus excision group (i.e. no weeping neotympanum).
Cameron et al.Reference Cameron, Demetri, Vivian and Brandon17 also described total annulus excision in their study of endoscopic lateral cartilage graft tympanoplasty, but our technique is different as it used a total microscopic technique; total annulus excision is performed irrespective of the size of the perforation with an intent to get a uniformly thick vibrating trimeric membrane. It does not include taking out the whole cuff of external canal skin but rather tries to preserve the vascularity of skin all around by elevating the anterior canal skin medially to laterally and preserving the vascular strip intact. Our technique is geared towards making sure that there is no mucous membrane on the lateral surface of the graft. This is achieved by: (1) totally denuding the handle of malleus with the specially designed instrument named ‘cobra’ as seen in Figure 2 and (2) seeking the muco-cutaneous junction under vision and removing the annulus with the medial cuff of skin attached to it, mucous membrane and the whole remnant tympanic membrane irrespective of the size of the perforation.
The limitation of our study was the small sample size. This was a non-conventional technique and for the benefit of the patients, the study planned to enrol only 28 cases in each group to assess results without causing significant complications.
Conclusion
Total annulus excision is an interlay type of tympanoplasty where graft is kept between mucosa medially and canal skin epithelium laterally after removal of residual tympanic membrane with its annulus. This study has shown that total annulus excision tympanoplasty has a high success rate in terms of hearing improvement, graft uptake and no discharge through the neotympanum post-operatively. The neotympanum formed was as close as possible to normal tympanic membrane anatomically and functionally with rich vascularisation around the graft. Although the sample size was small, we can say that in view of the advantages this technique offers, it may be preferred over the other conventional approaches in patients with central perforations. Further long-term randomised comparative studies are needed to validate the significant advantages of total annulus excision tympanoplasty over conventional tympanoplasty.
Competing interests
None declared










