Introduction
The growing popularity of endoscopic ear surgery has led to concerns about the loss of three-dimensional anatomical perception, which the microscope would previously have provided.
Traditional endoscope systems require three-dimensional (3D) orientation in a two-dimensional (2D) representation of the surgical field, resulting in inferior optical reproduction of anatomy. Criticisms of 2D endoscopic surgery include loss of stereopsis and reduced haptic feedback.Reference Wilhelm, Reiser, Kohn, Witte, Leiner and Mühlbach1 Expert surgeons compensate for downfalls of 2D endoscopy through observation of motion parallax and with experience.Reference Storz, Buess, Kunert and Kirschniak2
Three-dimensional endoscopes provide surgeons with a stereoscopic view of the operating field, facilitating depth perception, but they are not yet widely accepted. Wilhelm et al. suggest that surgeons who have already adapted to compensate with 2D devices prefer to continue with these instead of adopting 3D endoscopy.Reference Wilhelm, Reiser, Kohn, Witte, Leiner and Mühlbach1
Existing literature describes the superior performance of 3D endoscopes in simulated and clinical settings, mostly in laparoscopic procedures, and in the majority of studies that addressed surgeon preference, most participants chose 3D over 2D.Reference Storz, Buess, Kunert and Kirschniak2–Reference Tanagho, Andriole, Paradis, Madison, Sandhu and Varela9 Two recent systematic reviewsReference Sørensen, Savran, Konge and Bjerrum10,Reference Fergo, Burcharth, Pommergaard, Kildebro and Rosenberg11 state that the majority of randomised, controlled trials report superior performance and reduced error in 3D laparoscopy compared to 2D laparoscopy, and conclude that newer generation 3D laparoscopy is superior or equal to high-definition 2D laparoscopy. Recent meta-analyses report shorter or comparable operating time, reduced blood loss and shorter hospital stays in laparoscopic and thoracoscopic surgery performed with 3D versus 2D laparoscopes.Reference Vettoretto, Reggiani, Cirocchi, Henry, Covarelli and D'Andrea12,Reference Liang, Liang, Lei, Liu, Wang and He13
Optic replication of the surgical field is considered to be one of the key strengths of 3D endoscopy. Comparative studies within otolaryngology exist for endonasal and skull base surgery.Reference Bickerton, Nassimizadeh and Ahmed14,Reference Rampinelli, Doglietto, Mattavelli, Qiu, Raffetti and Schreiber15 One cohort study compared performance and preference in 2D versus 3D endoscopic type 1 tympanoplasty and stapedotomy using a cadaveric model.Reference Anschuetz, Niederhauser, Wimmer, Yacoub, Weibel and Mast16 There are few studies that quantified anatomical orientation, and none in the field of endoscopic ear surgery.
We set out to ascertain whether a 3D endoscopic system offers any benefit over 2D technology in endoscopic ear surgery. This study aimed specifically to: (1) compare novice surgeons’ ability to either describe anatomical relationships between fixed points on a model of the middle ear, or to perform simulated endoscopic exercises requiring three-dimensional orientation, using both 2D and 3D endoscopes; and (2) investigate operator preference for each task as a proxy for ease of use.
Materials and methods
Design and participants
An endoscope suite was set up in a staff common area within Morriston Hospital, a tertiary care centre in Swansea, Wales, UK. Storz 0-degree, rigid, high-definition endoscope systems, with a high-definition video screen, were used for the two arms of the study. The 2D scope had an outer diameter of 4 mm, a working length of 180 mm, and a focal range of 5–50 mm. The 3D scope had an outer diameter of 4 mm, a working length of 175 mm, and a focal range of 7–44 mm. The 3D system is a combined endoscope and camera head, whilst in the 2D system these are separate components. The weight of each endoscope system was 297 g and 337.8 g respectively, meaning the 2D system was heavier by 40.8 g.
Volunteers from a multidisciplinary team were randomly divided into two cohorts, each completing one task using both the 2D and 3D endoscope systems. Participants’ level of training is summarised in Table 1. Participants were randomised in starting with either the 2D or 3D system. Data for each task cohort were collected separately.
Table 1. Participants’ level of training, for each task cohort
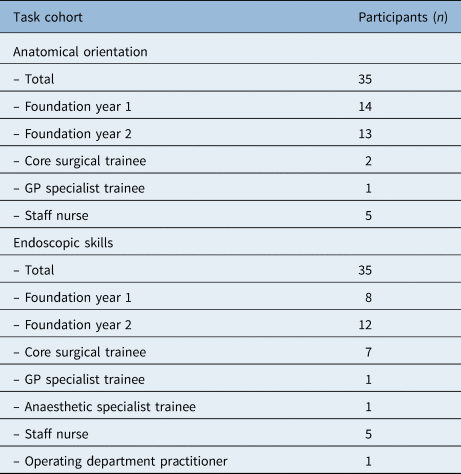
Cohorts were weighted heavily towards foundation doctors, with nursing staff being the second largest group. Consultants were excluded, as were trainees with formal endoscopic experience. GP = general practitioner
Anatomical orientation task
Thirty-five participants were asked to describe anatomical relations in a labelled silicone model of the medial wall of the middle ear. The model (Figure 1) was 3D printed using a computed tomography scan of the petrous temporal bone, and modified for use through the application of alphabet letters at specific fixed points on the medial wall. The points were chosen by the consultant endoscopic ear surgeon to ensure that the letters did not correspond to structures in normal middle-ear anatomy. This was to negate the application of anatomical knowledge by the participants whilst performing tasks.

Fig. 1. Three-dimensional printed silicone model of the middle ear. Alphabet letters were pasted to the medial wall of the middle ear in this model.
Participants were required to identify and explain the anatomical relation between different letters. Scoring was either simple (which letter is the most anterior? = 1 point) or compound (spatial relationship of ‘B’ and ‘G’? = 2 points) (Appendix 1).
The primary outcome measure was questionnaire score (sum of correctly described anatomical relations). Secondary outcomes were: reported difficulty (rated 1–5) and confidence in the correctness of answers (rated 1–5).
Endoscopic skills task
Thirty-five participants used a laparoscopic box trainer with a single grasping instrument to perform two simple exercises. The placement of elastic bands around hooks and the stacking of Polo® mints (annular confectionery) tested the core laparoscopic skills of camera navigation, instrument navigation, co-ordination, grasping and lifting.
The primary outcome measure was time to task completion. Secondary outcomes were: reported difficulty (rated 1–5) and reported confidence in task performance (rated 1–5).
System preference
Participants were asked to express a preference for either the 2D or 3D endoscopy system following completion of either the anatomical orientation or endoscopic skills task. Justification for their choice was given during the debrief.
Data analysis
All data were analysed with IBM SPSS® Statistics for Windows software, version 25.0. The paired t-test was used for all tests of significance.
Results
Anatomical orientation task
There was a significant difference between the 2D and the 3D groups in terms of anatomical orientation questionnaire scores (p < 0.001). Mean 3D group scores were 1.7 points higher than the 2D group scores (95 per cent confidence interval (CI) = 2.35190–1.07667) (Figure 2), out of a maximum of 14.

Fig. 2. Anatomical orientation questionnaire scores. Participants scored significantly higher on the questionnaire when using a three-dimensional (3D) compared with a two-dimensional (2D) endoscope system.
The mean rating for difficulty was 2.3 out of 5 in the 2D group, and 2.1 out of 5 in the 3D group. The mean rating of confidence in the correctness of answers was 3.5 out of 5 in the 2D group and 3.7 out of 5 in the 3D group (Figure 3).

Fig. 3. Self-ratings of difficulty and confidence for the anatomical orientation task. Participants rated difficulty and confidence similarly for both two-dimensional (2D) and three-dimensional (3D) endoscope systems, with marginal preference for 3D endoscopy. Circles indicate outliers.
Endoscopic skills task
There was no significant difference between the 2D and the 3D groups in terms of time to task completion (p > 0.05). Mean time to completion was 7.3 seconds quicker for the 3D group than the 2D group (95 per cent CI = −1.53071–27.98786) (Figure 4).

Fig. 4. Time taken to complete the endoscopic skills task. Participants displayed similar performance in terms of time to task completion with both the two-dimensional (2D) and the three-dimensional (3D) endoscope systems.
The mean rating for difficulty was 3.5 out of 5 in the 2D group, and 2.5 out of 5 in the 3D group. The mean rating of confidence in task performance was 3.1 out of 5 in the 2D group and 3.9 out of 5 in the 3D group (Figure 5).

Fig. 5. Self-ratings of difficulty and confidence for the endoscopic skills task. Participants rated lower difficulty and increased confidence with the three-dimensional (3D) endoscope system, compared with the two-dimensional (2D) system. Circles indicate outliers.
Operator preference
For anatomical orientation, 55 per cent of participants preferred 3D over 2D. For the endoscopic skills task, 91 per cent preferred the 3D endoscope. Reported criticisms were the need to wear 3D glasses, and distortion of the image if not located within a specific focal distance and orientation.
Discussion
We found that novice surgeons scored significantly higher in a test of anatomical orientation using the 3D endoscope, with no significant difference in the speed of completion of simple endoscopic skills compared to the 2D endoscope group. For both tasks, the majority of participants preferred the 3D endoscope.
Previous studies have established the superiority of 3D over 2D technology in laparoscopic and thoracoscopic procedures. This is the first study to focus specifically on endoscopic ear surgery, quantifying anatomical orientation using 2D and 3D endoscopes. Our findings add to existing literature suggesting an advantage of 3D endoscopy in simulated surgical tasks and an operator preference for this technology.
Participants scored significantly higher in the anatomical orientation task, requiring depth and spatial perception, when using a 3D endoscope. In their seminal paper, Way et al. reported that most errors leading to bile duct injury in laparoscopic cholecystectomy are due to errors in perception or misinterpretation of an image, rather than errors of skill, knowledge or judgement.Reference Way, Stewart, Gantert, Liu, Lee and Whang17 It is therefore vital for endoscopic imaging to support anatomical orientation. Egi et al. found significantly decreased deviation and approaching time in simulated laparoscopic tasks with 3D imaging compared to 2D imaging.Reference Egi, Hattori, Suzuki, Sawada, Kurita and Ohdan18 Improved spatial perception and accuracy yield increased efficiency of instrument movement. Ogino-Nishimura et al. also described an increased understanding of surgical anatomy with 3D endoscopy, as well as increased precision of instrumentation in posterior sinus and skull base surgery.Reference Ogino-Nishimura, Nakagawa, Sakamoto and Ito19 Three-dimensional endoscopy may therefore have an important role in improving operative morbidity.
This study replicates previously reported findings of decreased or comparable time to completion of endoscopic tasks with 3D (compared to 2D) technology. Negative operator reviews of 3D endoscopy in initial studies are a likely contributor to slow uptake of the technology. The criticisms included: the side effects of digital stereopsis (blurring, fatigue and headache), the need to wear 3D glasses, the incongruity of stereoscopic fields, and the reduced resolution and lower brightness of images compared with 2D endoscopy.Reference Wilhelm, Reiser, Kohn, Witte, Leiner and Mühlbach1 These weaknesses have mostly been negated by the introduction of high-definition 3D endoscopes.Reference Szold20 Wilhelm et al. reported that novel 3D technologies improve operator performance, without these side effects (which are associated with higher cognitive workload).Reference Wilhelm, Reiser, Kohn, Witte, Leiner and Mühlbach1 Our findings are consistent with this and others’ reports, with participants expressing a preference for 3D over 2D technology. The side effects of 3D technology have previously been described to affect preference, and some side effects were evident here (the wearing of goggles or image distortion at an incorrect focal distance). Through the assessment of ‘confidence’ and ‘difficulty’, as reported by participants, we found no evidence to suggest higher cognitive workload with 3D endoscopy.
Narrowly defined exclusion criteria resulted in a heterogeneous cohort. All participants were, however, novice surgeons with no prior experience of endoscopy. This sample is therefore representative of those entering surgical training. The participants were not tested for stereoacuity prior to inclusion, but previous studies report low exclusion rates for this reason,Reference Storz, Buess, Kunert and Kirschniak2 and there were no observed behaviours that would negate stereoscopic advantage (e.g. holding one eye closed). The unavailability of a middle-ear box trainer meant that the skills task was performed in a laparoscopic box trainer. Previous studies in otolaryngological surgery have demonstrated the superiority of 3D over 2D endoscopy in operative ranges consistent with endoscopic ear surgery.Reference Bickerton, Nassimizadeh and Ahmed14,Reference Anschuetz, Niederhauser, Wimmer, Yacoub, Weibel and Mast16,Reference Ogino-Nishimura, Nakagawa, Sakamoto and Ito19 Replicating this would have added to the evidence base for 3D endoscopy specific to endoscopic ear surgery, but the almost identical size and focal depth of the 2D and 3D systems used in this study is considered to allow applicability of the findings.
The primary outcome measure for the skills task was time to completion, which is used extensively as a proxy for technical competence. Precision and error rate were not measured; these would have given a more complete impression of application in vivo. The secondary outcomes of reported ‘confidence’ and ‘difficulty’ were subjective assessments of cognitive workload. Others have achieved objective assessment of these through eye movement trackingReference Anschuetz, Niederhauser, Wimmer, Yacoub, Weibel and Mast16 and the use of a magnetic navigation system for following instrument movements.Reference Wilhelm, Reiser, Kohn, Witte, Leiner and Mühlbach1,Reference Rampinelli, Doglietto, Mattavelli, Qiu, Raffetti and Schreiber15 Future studies are needed to validate our findings, perhaps through the development of a specific simulated trainer for endoscopic ear surgery.
• Traditional endoscope systems require three-dimensional (3D) orientation in a two-dimensional (2D) representation of the surgical field
• This results in inferior optical reproduction of anatomy than that of the commonly used operating microscope
• There are few studies that quantify anatomical orientation in 3D endoscopy, and none in the field of endoscopic ear surgery
• A prospective, randomised study was conducted, comprising 70 surgically naïve participants
• Anatomical orientation, performance and preference in using a 2D or 3D endoscope to complete simulated surgical tasks were assessed
• Clarification of the hypothesised benefits of 3D endoscopy should influence surgical training programmes, and would likely affect operative morbidity in endoscopic ear surgery
Conclusion
As endoscopic ear surgery becomes increasingly widespread, failure to adopt 3D technology may limit its clinical potential. We demonstrate the superiority of 3D endoscopy in anatomical orientation, specific to endoscopic ear surgery, with statistically indistinguishable performance in a skills task using a simulated trainer. Novice surgeons preferred 3D over 2D endoscopy in both tasks. This study replicates research favouring 3D endoscopy in abdominal and thoracic surgery in the field of otology, with implications for improving operative morbidity. This should increase confidence for otologists to adopt 3D technology in clinical practice and advocate for greater exposure to 3D endoscopy for junior surgeons in ENT training curricula.
Acknowledgement
Thanks to the Maxillofacial Laboratory at Morriston Hospital for production of the three-dimensional printed petrous temporal bone.
Competing interests
None declared
Appendix 1. Anatomical relations questionnaire
Level of training ______________ Trial number_____________________
Which letter is the most anterior?
Which letter is the most posterior?
Which letter is the most lateral (closest to you)?
Spatial relationship between ‘H’ and ‘A’?
Spatial relationship between ‘H’ and ‘F’?
How many shapes do you see?
List the shape(s) below:
Which letter is most medial (furthest from you)?
Spatial relationship of ‘B’ and ‘G’?
Spatial relationship of ‘B’ and ‘K’?
How hard was it to appreciate the 3D relationships in the model?
(1 = very easy, 5 = very hard)
1 2 3 4 5
How confident are you that your answers are right?
(1 = not confident, 5 = very confident)
1 2 3 4 5
Time to complete the questions _______________________








