Introduction
The parotid, submandibular and sublingual glands are the three major salivary glands in humans. Another 500–1000 small glands are scattered throughout the lining of the upper aerodigestive tract, and are collectively called the minor salivary glands.Reference Beale and Madani1 Nodal metastasis in salivary gland malignancies has important surgical and oncological implications; a good understanding of the complex lymphatic drainage pathways is paramount to the head and neck surgeon.Reference Bhattacharyya and Fried2 Here, we provide a comprehensive and contemporary review of the lymphatic drainage of the salivary glands, with special emphasis on its surgical applications.
Materials and methods
This review was performed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (‘PRISMA’) guidelines.Reference Moher, Liberati, Tetzlaff, Altman and ;3 We used a comprehensive combination of key words to search Medline, Embase and PubMed databases (Table 1).
Table 1. Search strategy and keyword combination for Medline, Embase and PubMed databases

We included all studies that described any aspect of the anatomy of lymphatic drainage of the salivary glands in humans. Titles and abstracts of studies retrieved by the primary search were systematically screened, and potentially relevant studies were shortlisted for full-text review. The search was supplemented by manual follow-up screening of the references of the full-text articles.
Exclusion criteria
We excluded reviews, articles written in languages other than English, studies on non-human subjects, case reports and conference abstracts. We also excluded studies investigating pathological salivary lymph nodes, such as those in malignant metastases.
Results
Our primary search of Medline, Embase and PubMed databases yielded 2328, 2066 and 3687 articles, respectively (Figure 1). Following electronic deduplication, 2861 titles and abstracts were screened, and 111 articles were finally shortlisted. A full-text review of the shortlisted reports and a manual bibliographic search resulted in 13 eligible studies for inclusion in a qualitative literature review.Reference Rouvière and Tobias4–Reference Katayama16
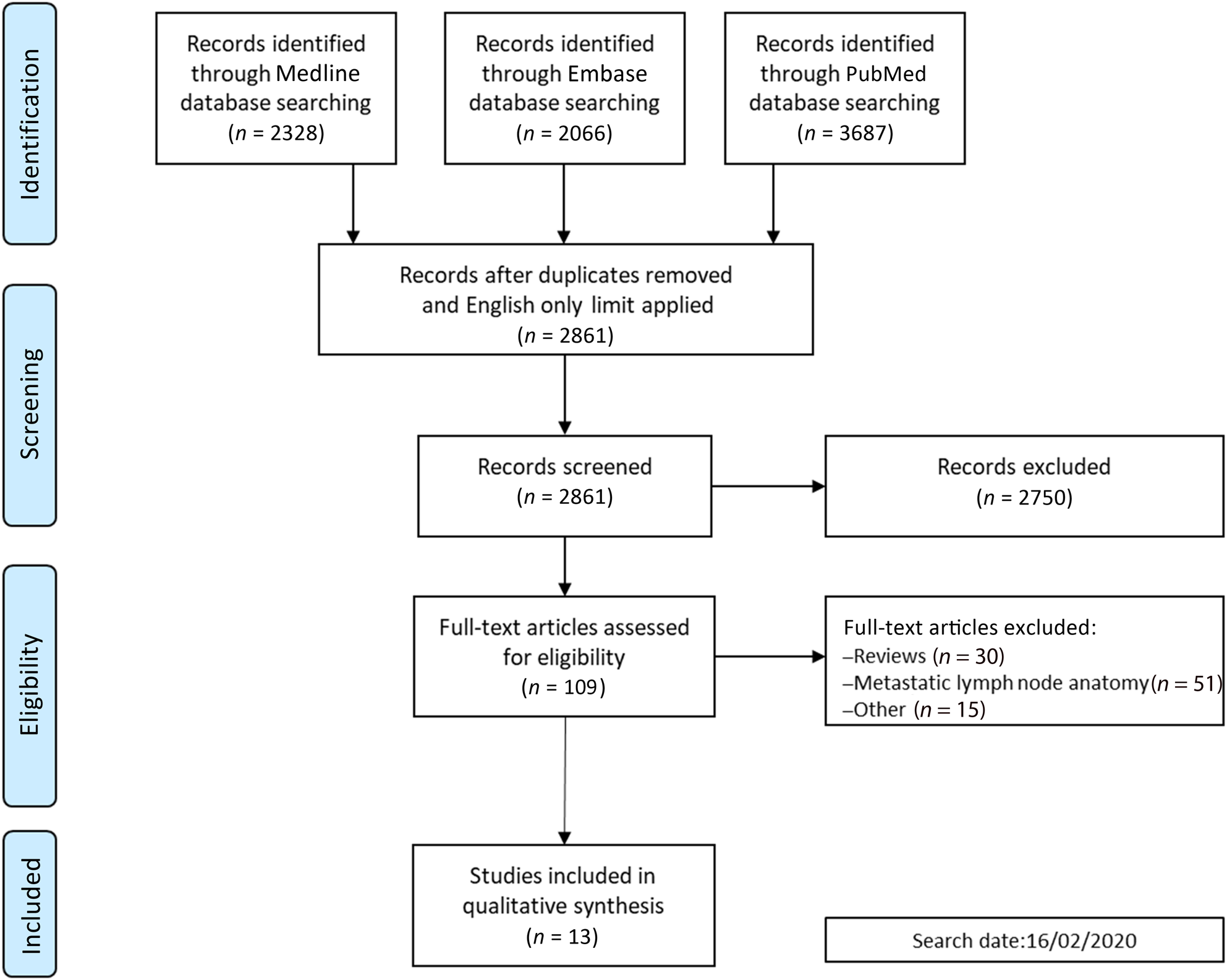
Fig. 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (‘PRISMA’) flow diagram showing the different steps of the systematic review.
Discussion
Parotid gland
The parotid gland is the largest salivary gland, usually palpable in the pre-auricular region against the ramus of the mandible. It contains the facial nerve and the external carotid artery with their terminal branches, in addition to the retromandibular vein, autonomic nerves and the surgically important parotid lymph nodes.Reference Beale and Madani1,Reference Stong, Johns, Johns, Bailey and Johnson17
The parotid gland has two lymphatic systems, extraglandular and intraglandular; while separable by topography, they act as a single functional drainage unit.Reference Stong, Johns, Johns, Bailey and Johnson17–Reference Batsakis19 The extraglandular nodes are situated superficial to the gland, while the intraglandular ones are embedded within the parenchyma (Figure 2).Reference Stong, Johns, Johns, Bailey and Johnson17,Reference Som18 Some authors further divide the extraglandular group into a subfascial subgroup, located between the gland and its capsule, and an extra-fascial (pre-auricular) subgroup, usually comprising one to two nodes embedded in the subcutaneous fat around the superficial temporal vessels.Reference Rouvière and Tobias4,Reference Marks5,Reference Stong, Johns, Johns, Bailey and Johnson17,Reference Taylor, Brant, Mendenhall, Mendenhall, Cassisi and Stringer20,Reference Grégoire, Ang, Budach, Grau, Hamoir and Langendijk21
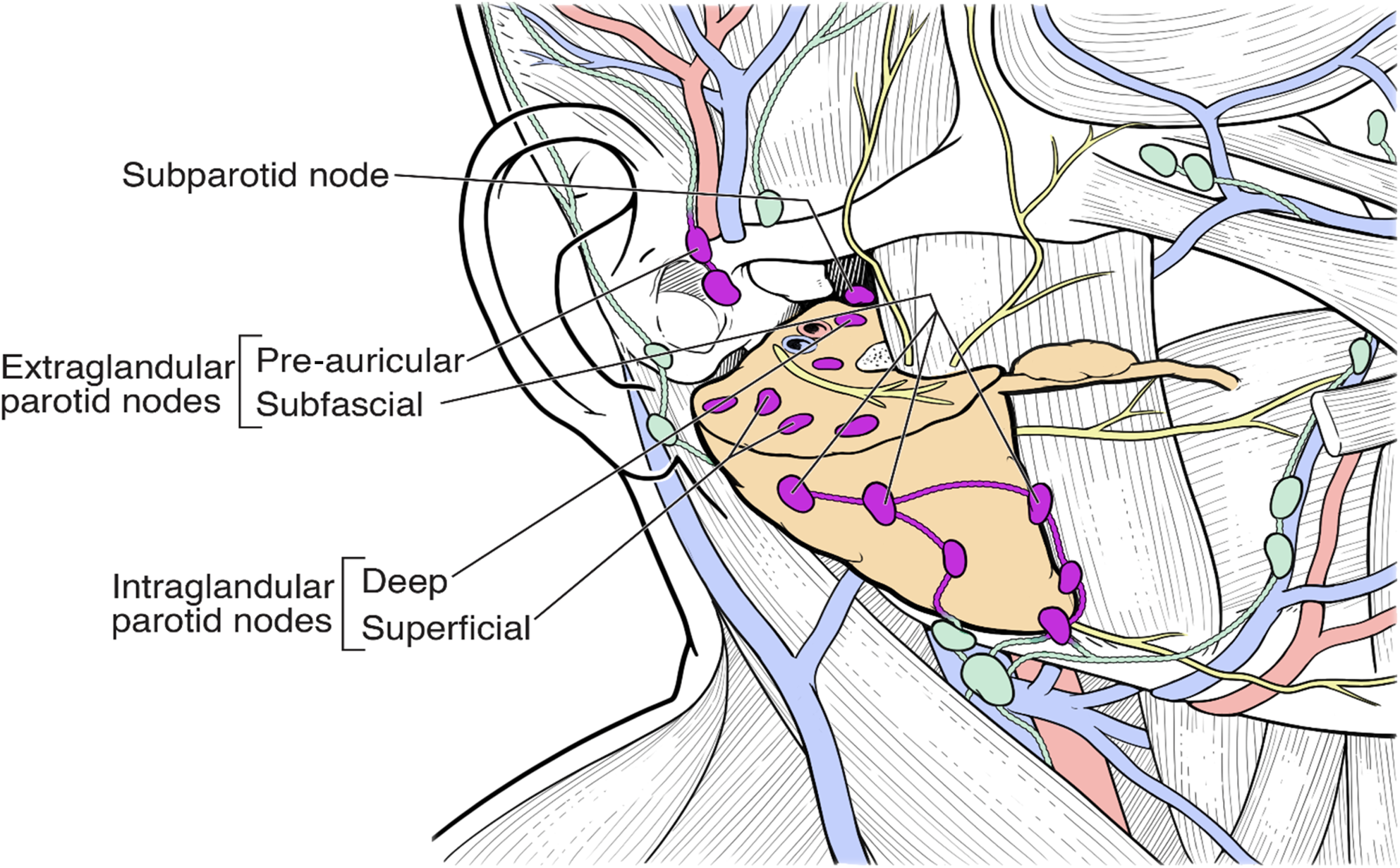
Fig. 2. Schematic illustration showing the various subgroups of parotid lymph nodes.
The parotid lymph nodes are sometimes referred to as ‘level VIII’ nodes, especially in the context of head and neck malignancy.Reference Grégoire, Ang, Budach, Grau, Hamoir and Langendijk21 These nodes not only drain the parotid gland, but also an extensive and varied territory in the face, scalp, ear, nasopharynx and soft palate.Reference Carlson6,Reference Som18,Reference Batsakis19 That makes these nodes clinically relevant in cases with nodal metastasis from a primary parotid gland malignancy, and in other tumours such as malignant melanoma and squamous cell carcinoma (SCC) originating from their afferent areas.Reference Batsakis19,Reference Graham22 In addition, pathological intraglandular parotid nodes may be confused both clinically and on computed tomographic and magnetic resonance images with primary parotid gland tumours.Reference Som18,Reference Batsakis19
The presence of an intraglandular parotid node is unique to the parotid gland, compared to other salivary glands. This is due to entrapment of lymphatic tissue within the parotid parenchyma prior to complete formation of the parotid capsule during fetal development.Reference Beale and Madani1 There is a wide variation in the number of intraglandular parotid nodes, especially in older individuals, but they are usually connected with a rich interlacing network of lymphatic vessels.Reference McKean, Lee and McGregor7,Reference Sönmez Ergün, Gayretli, Büyükpınarbaşılı, Yıldız, Gürses and Avşar8,Reference Poirier, Cuneo, Delamere and Leaf9,Reference Batsakis19,Reference Graham22
Intraglandular parotid nodes are usually subdivided anatomically into a larger superficial group (range of 3–19 nodes) and a smaller deep group (range of 0–9 nodes), generally corresponding to the superficial and deep parts of the parotid gland respectively.Reference McKean, Lee and McGregor7,Reference Pisani, Ramponi and Pia10,Reference Garatea-Crelgo, Gay-Escoda, Bermejo and Buenechea-Imaz11,Reference Cracchiolo and Shaha23 An arbitrary plane marking the intraglandular portion of the facial nerve is universally used to divide the parotid gland, surgically rather than anatomically, into the superficial and deep lobes.Reference Graham22,Reference McKenzie24 Interestingly, the intraglandular parotid nodes have been shown to be topographically related to the retromandibular vein as opposed to the facial nerve.Reference Poirier, Cuneo, Delamere and Leaf9,Reference Batsakis19,Reference Taylor, Brant, Mendenhall, Mendenhall, Cassisi and Stringer20,Reference Graham22 However, many authors still prefer to describe the intraglandular parotid nodes as superficial or deep in relation to the facial nerve instead of the retromandibular vein.Reference McKean, Lee and McGregor7,Reference Pisani, Ramponi and Pia10,Reference Taylor, Brant, Mendenhall, Mendenhall, Cassisi and Stringer20 While being anatomically inaccurate, this can be more surgically relevant when performing superficial or total parotidectomy, as the facial nerve is the landmark for dissection.
In their cadaveric study, McKean et al.Reference McKean, Lee and McGregor7 demonstrated only 16 out of the total of 193 intra-parotid nodes found to be deep to the facial nerve, and of these all but 4 were superficial to the retromandibular vein. The presence of a larger and more dominant superficial lymphatic system is not surprising considering the fact that almost 80 per cent of the parotid tissue resides within the superficial part of the gland.Reference Cracchiolo and Shaha23 However, in an anatomical study of surgical parotid specimens reported by Pisani et al.,Reference Pisani, Ramponi and Pia10 deep nodes were found in 90 per cent of the cases. Notably, metastatic spread to the deep intraglandular parotid nodes was detected in half of the cases with confirmed metastatic involvement of the superficial nodes.Reference Pisani, Ramponi and Pia10 The authors suggested the presence of direct and indirect lymphatic connections between the superficial and deep parotid lymph nodes. This finding is surgically relevant in cases of primary superficial parotid malignancy, or cutaneous intraglandular parotid nodes metastasis, as any dissection limited to superficial parotidectomy may potentially leave disease behind, and resection of the deep lobe might be necessary in high-risk cases.Reference Pisani, Ramponi and Pia10,Reference Taylor, Brant, Mendenhall, Mendenhall, Cassisi and Stringer20,Reference Cracchiolo and Shaha23
Submandibular gland
The submandibular gland is the second largest of the salivary glands, and fills a major portion of the submandibular triangle. The lymphatic drainage of the submandibular gland is carried to the adjacent submandibular nodes located on the bony, deep and cutaneous surfaces of the gland, as shown in Figures 3 and 4.Reference Beale and Madani1,Reference Stong, Johns, Johns, Bailey and Johnson17,Reference Lengelé, Hamoir, Scalliet and Grégoire12 These nodes are widely known as level IB nodes, based on the classification proposed by the American Head and Neck Society and the American Academy of Otolaryngology – Head and Neck Surgery.Reference Robbins, Clayman, Levine, Medina, Sessions and Shaha25 The submandibular nodes extend within the boundaries of the anterior belly of digastric muscle, the body of the mandible and the stylohyoid muscle, or alternatively the vertical plane passing through the posterior border of the submandibular gland.Reference Robbins, Shaha, Medina, Califano, Wolf and Ferlito26
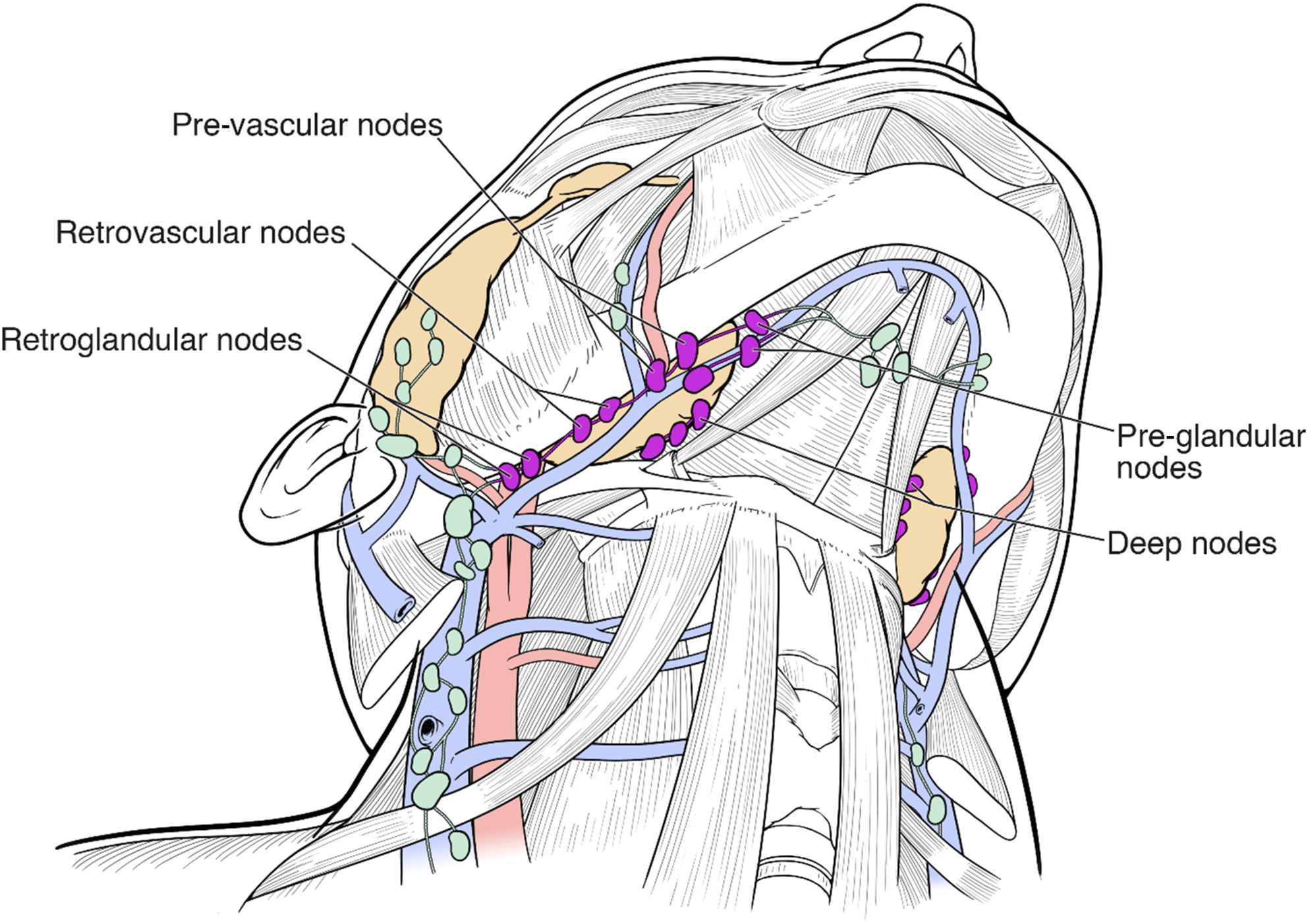
Fig. 3. Schematic illustration showing the submandibular nodes and their relationship to the submandibular gland and the anterior facial vein.

Fig. 4. Schematic illustration (crosscut) of the floor of the mouth in a coronal plane showing the arrangement of the lingual lymph nodes.
The submandibular nodes were classically subdivided into five groups by Rouvière in his seminal book Anatomy of the Human Lymphatic System, published in 1932 (translated into English in 1938).Reference Rouvière and Tobias4 These five groups are the pre-glandular, pre-vascular, retrovascular, retroglandular and the much debated intraglandular groups. The pre-glandular group consists of up to five nodes situated along the submental vein in the triangular space bounded posteriorly by the submandibular gland, superiorly by the mandible and antero-inferiorly by the anterior belly of the digastric muscle.Reference DiNardo13,Reference Abe, Murakami, Noguchi, Yajima and Kohama14 The peri-vascular nodes (the pre-vascular and retrovascular nodes) are defined in relation to the anterior facial vein, not the artery.Reference Lengelé, Hamoir, Scalliet and Grégoire12,Reference DiNardo13,Reference Robbins, Shaha, Medina, Califano, Wolf and Ferlito26 The pre-vascular node is often the largest submandibular node, and may be seen superficial to the submandibular gland or between the gland and the inner surface of the mandible. The retrovascular nodes are usually one or two nodes positioned posterior to the anterior facial vein, and may be hidden between the mandible and the submandibular gland, or embedded in fatty tissue superficial to the gland.Reference DiNardo13 It is a common misconception to describe the peri-vascular nodes as ‘facial nodes’, and this term should be reserved for the lymph nodes along the course of the facial artery in the face.Reference Rouvière and Tobias4,Reference DiNardo13 The retroglandular lymph nodes lie immediately at the posterior margin of the submandibular gland, and can be easily confused with level II lymph nodes located more laterally.Reference Robbins, Shaha, Medina, Califano, Wolf and Ferlito26
Some authors added a sixth group not previously described by Rouvière – the deep submandibular nodes – which are usually small and inconsistently present.Reference Lengelé, Hamoir, Scalliet and Grégoire12,Reference DiNardo13 These are located anywhere along the undersurface of the submandibular gland, but superficial to the mylohyoid muscle and posterior aspect of the hyoglossus muscle (Figure 4).
While Rouvière himself doubted the presence of intracapsular or intraglandular submandibular nodes, he added this group based on previous studies by Bartels, who noted the existence of lymph nodes within the submandibular gland.Reference Bartels27 However, later research by DiNardo and others clearly demonstrated no evidence of intraglandular submandibular nodes.Reference DiNardo13,Reference Spiegel, Brys, Bhakti and Singer28,Reference Dhiwakar, Ronen, Malone, Rao, Bell and Phillips29 Moreover, Fives et al.Reference Fives, Feeley, Sadadcharam, O'Leary and Sheahan30 reviewed the original pathological materials of 69 submandibular glands excised during neck dissection for oral cavity malignancy and oropharyngeal SCC, and none (0 per cent) contained intraglandular lymph nodes. Therefore, in contrast to the parotid gland, lymphatic malignant spread to the submandibular gland is not possible. However, excision of the submandibular gland might become clinically necessary if it is directly invaded by a floor of mouth malignancy or extracapsular spread from the adjacent submandibular nodes. Moreover, excision of a sound submandibular gland might also be required when performing neck dissection for oral cavity malignancy and oropharyngeal SCC to gain access to the relevant nodal groups. For all other scenarios, many surgeons have recently advocated sparing the submandibular gland from excision during routine neck dissection, to reduce unnecessary morbidity, especially with bilateral dissections.Reference Spiegel, Brys, Bhakti and Singer28–Reference Basaran, Ulusan, Orhan, Gunes and Suoglu31
In addition to draining the adjacent submandibular gland, the submandibular nodes also drain a wide and variable territory that includes the lips, nose, teeth and palate, the anterior portion of the tongue, the floor of the mouth, and the lingual glands.Reference Som18 They also drain the facial nodes, which drain the eyelids, cheek and mid portion of the face. Therefore, the submandibular nodes, especially the peri-vascular group, are not only clinically significant in primary submandibular gland cancers, but are important in the context of oropharyngeal SCC. They act as the primary draining nodes of the oral cavity, and can harbour metastatic involvement from floor of mouth and tongue cancers in about 5–7 per cent of cases.Reference Basaran, Ulusan, Orhan, Gunes and Suoglu31,Reference Lim, Kim, Koh, Kim, Kim and Kim32
Sublingual salivary glands
The sublingual glands are the smallest of the major salivary glands. They are flat, oblong-shaped structures located immediately below the mucosa on the floor of the mouth. In 1898, Küttner first described two to three lymph nodes situated posterior and anterior to the sublingual glands.Reference Küttner33 Rouvière called these nodes lingual lymph nodes, and further subdivided them into median and lateral groups.Reference Rouvière and Tobias4 Other authors prefer to use the term ‘sublingual’ lymph nodes to describe these nodes, as this is more indicative of the anatomical site; however, both terms are often used interchangeably.Reference Zhang, Ord, Wei and Zhao34,Reference Kaya, Öztürk and Turhal35
Ananian et al.Reference Ananian, Gvetadze, Ilkaev, Mochalnikova, Zayratiants and Mkhitarov15 dissected specimens from 21 cadavers and divided the lingual lymph nodes topographically into 3 groups: median nodes, para-hyoid (intermediate) nodes and para-glandular (lateral) nodes. The median nodes, historically called ‘intralingual glands’ by Poirier, are located between the genioglossus and geniohyoid muscles on either side of the lingual septum (Figure 4). The para-hyoid (intermediate) nodes are situated along the course of the lingual artery between the genioglossus and geniohyoid muscles medially and hyoglossus muscle laterally. The para-glandular (lateral) nodes are located around the sublingual glands in the space limited by the hyoglossus muscle medially and the internal surface of the mandibular body laterally.Reference Ananian, Gvetadze, Ilkaev, Mochalnikova, Zayratiants and Mkhitarov15,Reference Zhang, Ord, Wei and Zhao34 The lingual lymph nodes are a very inconsistent group, with lateral and intermediate nodes found in 24–30 per cent and median nodes in 0–15.1 per cent of cases.Reference Ananian, Gvetadze, Ilkaev, Mochalnikova, Zayratiants and Mkhitarov15,Reference Katayama16
Beside draining the sublingual glands, the lingual lymph nodes also receive afferent lymphatics from the structures situated in the floor of mouth and the tongue.Reference Som18,Reference Zhang, Ord, Wei and Zhao34 The lingual lymph nodes can therefore harbour metastatic spread of oral malignancy and impact overall survival if overlooked.Reference Zhang, Ord, Wei and Zhao34–Reference Woolgar36
Minor salivary glands
The minor salivary glands are located in the submucosal layer throughout the upper aerodigestive tract.Reference Beale and Madani1,Reference Stong, Johns, Johns, Bailey and Johnson17 Heterotopic minor salivary glands may also be found in many unusual sites, including the mandible, neck, middle ear and external auditory canal.Reference Hiatt, Sauk, Ellis, Auclair and Gnepp37 Around two-thirds of minor salivary gland carcinomas are encountered in the oral cavity, followed by the oropharynx, which likely correlate with the natural density of these glands.Reference Hay, Migliacci, Karassawa Zanoni, McGill, Patel and Ganly38,Reference Moreno, Moreno and Tomé39 The lymphatic drainage of the minor salivary glands corresponds to the general lymphatic drainage of the region they are located in.Reference Stong, Johns, Johns, Bailey and Johnson17
Efferent pathways of lymphatic drainage from salivary glands
The efferent lymphatic drainage of the head and neck (including the salivary glands) is classically described in terms of three functional drainage pathways depending on the origin.Reference Lengelé, Hamoir, Scalliet and Grégoire12 These are the main lymphatic pathway, the posterior accessory lymphatic pathway and the anterior accessory lymphatic pathway (Figure 5).

Fig. 5. Schematic illustration showing the different pathways of the salivary glands’ lymphatic drainage in the neck.
The main efferent lymphatic pathway in the neck usually passes through the submental and submandibular nodes to the upper jugular nodes.Reference Lengelé, Hamoir, Scalliet and Grégoire12 Rouvière detailed two principal connections between the submandibular nodes (level IB) and the upper jugular nodes (level II) via lymphatic channels that follow the anterior facial vein (para-venous) and the facial artery (para-arterial).Reference Rouvière and Tobias4,Reference DiNardo13 The lymphatic drainage coming through these pathways usually joins the efferent drainage of the parotid space nodes in the upper jugular nodes, before draining in a stepwise manner to the middle and lower jugular nodes (levels III and IV respectively).Reference Som18 It eventually empties in the brachiocephalic veins via the thoracic and the right lymphatic ducts.Reference Lengelé, Hamoir, Scalliet and Grégoire12,Reference Som18 The posterior accessory lymphatic pathway links the posterior upper jugular nodes (level IIB) to the posterior cervical group (level V), before it goes through successive nodes located alongside the accessory nerve and the transverse cervical vessels.Reference Lengelé, Hamoir, Scalliet and Grégoire12 The anterior accessory pathway runs from the submandibular nodes medially to the submental nodes, where it either descends to the anterior neck lymph nodes (level VI) or re-joins the main pathway at level III or IV (Figure 5).Reference Rouvière and Tobias4,Reference Poirier, Cuneo, Delamere and Leaf9,Reference DiNardo13
The efferent lymphatic drainage of the parotid nodes (intraglandular and extraglandular) primarily passes through the infra-auricular nodes and the upper jugular nodes (level II) to continue caudally in the main pathway.Reference Beale and Madani1,Reference Lengelé, Hamoir, Scalliet and Grégoire12,Reference Stong, Johns, Johns, Bailey and Johnson17,Reference Som18 The subparotid nodes (Figure 2), located outside and medial to the parotid gland, may also contribute to the drainage of the deep part of the gland.Reference Poirier, Cuneo, Delamere and Leaf9,Reference Lengelé, Hamoir, Scalliet and Grégoire12 These nodes are connected with the retropharyngeal and the posterior upper jugular nodes, and may drain via the posterior accessory pathway.Reference Beale and Madani1,Reference Stong, Johns, Johns, Bailey and Johnson17,Reference Som18 The lymphatic drainage of the sublingual glands and submandibular glands usually follows the main and the anterior accessory pathways. The efferent lymphatic channels from the lingual lymph nodes usually join the submandibular and submental nodes.Reference Beale and Madani1,Reference Ananian, Gvetadze, Ilkaev, Mochalnikova, Zayratiants and Mkhitarov15,Reference Stong, Johns, Johns, Bailey and Johnson17,Reference Som18
It should be noted that these complex lymphatic pathways in the neck can be highly variable, and unexpected interconnections between these groups might occur. As demonstrated by the lymphographic studies by RouvièreReference Rouvière and Tobias4 and Pan et al.,Reference Pan, Le Roux and Briggs40 the lymph-collecting vessels in the head and neck do not always enter the closest lymph nodes but sometimes bypass them, especially through the anterior accessory pathway. This finding is clinically relevant as it offers an anatomical explanation for skip metastases seen in head and neck malignancy.Reference Ferlito, Shaha, Rinaldo, Pellitteri, Mondin and Byers41
Conclusion
Lymphatic drainage of the salivary glands tends to form complex local arrangements. Metastases from a primary salivary malignancy to the local and regional lymph nodes may not only pose clinical challenges to the surgeon, but also often perplex the pathologist, the radiologist and the oncologist, particularly if they are unaware of the aggregation of lymph nodes draining the salivary glands. This review provides a valid anatomical explanation for the commonest nodal metastasis patterns encountered in salivary gland malignancy.
Acknowledgements
We would like to thank Mr Blake Swanson, medical illustrator, for his help in producing the figures used in this review.
Competing interests
None declared