Introduction
Injury to the thoracic duct or right lymphatic duct during cervical surgery is uncommon, but has significant associated morbidity. If injury is to be avoided, there must be a sound understanding of the anatomy of the lymphatics, and an intra-operative alertness to the potential for considerable inter-patient variation in this anatomy. Unlike left-sided thoracic duct injury, many surgeons underestimate or are unaware of the incidence of chyle leakage as a complication of right-sided neck surgery.
In this review, we describe the anatomical variation of the thoracic and cervical lymphatic ducts, demonstrating why right-sided lymphatic duct injury may be as serious as that on the left. The prevalence of chyle collections and fistulae is also reviewed.
Anatomy of the thoracic and right lymphatic ducts
The thoracic duct and the right lymphatic duct are the final common vessels in the lymphatic system, which overall drains between six and seven hundred lymph nodes.Reference Skandalakis, Skandalakis and Skandalakis1 It is well documented that there is a great degree of variation in the anatomy of the thoracic duct, and yet teaching at medical school or in early surgical life often fails to explore this fact. Basic anatomy texts such as Grant's Atlas of Anatomy usually state only that the thoracic duct receives all lymph that forms below the diaphragm, and empties into the junction of the left subclavian and internal jugular veins.Reference Agur2 This arrangement is indeed that most commonly seen, but there is also the potential for wide variation. Gray's Anatomy acknowledges this variation, stating that the course and termination of the thoracic duct are not only variable but also often multiple.Reference Standring3
Embryology
The embryology of the lymphatic system is not fully understood, but begins to explain the number of anatomical permutations. The first lymphatic primordia appear at the venous angles at around six weeks of gestation. Further primordia form as sprouts from the endothelial lining of veins, and fuse to form symmetrical bilateral right and left thoracic ducts. A dense network of interconnecting lymphatic vessels forms between the main trunks, and the venous connections are lost.Reference Davis4, Reference van der Putte and van Limborgh5 The adult thoracic duct is formed by the persistence and growth of some parts of the embryonic duct, and the disappearance of others. The most frequently seen pattern of the adult thoracic duct develops from the caudal part of the right duct, a transverse anastomotic branch, and the cranial part of the left duct.Reference Davis4, Reference Kihara and Adachi6, Reference Sabin7 In this situation, the upper part of the right duct becomes the right lymphatic duct. The extensive developmental lymphatic plexus explains the multiple types of termination of the duct.
As may be expected by the common origin of the venous and lymphatic systems, anatomical variation of the right and left lymphatic ducts is associated with venous malformations such as persistent left superior vena cavaReference Kihara and Adachi6 and retroesophageal right subclavian artery.Reference Nathan and Seidel8 However, there are also associated arterial malformations, such as partially or fully persistent right aortic archReference van der Putte and van Limborgh5, Reference Yamada9 and anomalous right subclavian artery.Reference Epstein and Debord10
Anatomy
The thoracic duct is thin-walled and typically 45 cm long and 2–3 mm in diameter, but can dilate to several times this width when full. It usually arises from the cisterna chyli – an elongated, dilated sac at the confluence of the lumbar and intestinal trunks – but receives contributions from smaller vessels. The cisterna chyli is most often located at the level of the second lumbar vertebra, to the right of the aorta, though variation exists and it may be indistinct or absent.Reference Skandalakis, Skandalakis and Skandalakis1 The thoracic duct terminates in a cervical lympho-venous junction, the various permutations of which are described below, including its relationship with the right lymphatic duct.
The right lymphatic duct is less well characterised than the thoracic duct, but is equally susceptible to anatomical variation. The most frequently seen origin of the right lymphatic duct is from the right jugular, bronchomediastinal and subclavian lymphatic trunks,Reference Davis4 although these vessels may terminate individually so that the main duct is absent (Figure 1). If present, the duct is 1–2 cm long, closely related to the anterior scalene muscle, and usually empties into the junction of the right subclavian and internal jugular veins.Reference Skandalakis, Skandalakis and Skandalakis1
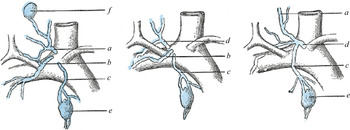
Fig. 1 Medical illustration showing various arrangements of terminal collecting trunks of the right side. a = jugular trunk; b = subclavian trunk; c = bronchomediastinal trunk; d = right lymphatic trunk; e =gland of internal mammary chain; f = gland of deep cervical chain. Reproduced with permission.Reference Standring3
Aside from a role in immune surveillance, the primary function of the lymphatics is to drain the tissues of lymphatic and chylous fluid: lymph arising from all tissues, and chyle, containing emulsified fats, originating from the lacteals of the small intestine. Most commonly, the thoracic duct drains both lymph and chyle, whereas the fluid conveyed via the right lymphatic duct consists solely of lymph from the right cervical and thoracic region. However, if this were always the case, high-volume chyle leaks would not be seen on the right side.
Anatomical variation
Like other organ systems, developmental anomalies of the lymphatic system can provide surgical challenges. Cystic hygromas and primary lymphoedema are two such pathologies, although they are relatively uncommon. However, localised anatomical variation of the pre-vertebral lymphatic system is common, and not usually associated with pathology.Reference van der Putte and van Limborgh5 The variable anatomy of the lymphatics is often misunderstood, and therefore these structures can be at significant risk during neck surgery.
Path of the thoracic duct
The majority of the course of the thoracic duct is mediastinal and beyond the reach of neck surgeons, although variation here has a significant impact on anatomy within the neck. Bilateral thoracic ducts ascending in parallel, anterior to the vertebral column and behind the oesophagus, have been described, often with one or more anastomotic branches crossing the midline.Reference Chen, Shoumura and Emura11 Isolated bilateral ducts are extremely rare, with few cases reported.Reference Yamada9 More commonly, if the thoracic duct is right-sided, the left duct will be absent.Reference Watson12 Partially duplicated ducts are frequently interconnected with anastomosing branches,Reference Standring3, Reference Davis4 and even single ducts may bifurcate and then merge again before entering the venous angle.Reference Nathan and Gitlin13
Termination of the thoracic duct
The greatest variation in thoracic duct anatomy is seen at and around its termination,Reference Davis4 in an area explored during dissection of level IV and V lymph nodes.Reference Rouvière14 Perhaps it is therefore unsurprising that the most common site of injury to the lymph duct during neck dissection is lateral to the inferior portion of the carotid sheath on either side.Reference Crumley and Smith15, Reference Jacobsson16
Various classifications have been developed to describe the variation in course and termination of the thoracic duct.Reference Nathan and Gitlin13 JacobssonReference Jacobsson16 classified the cervical part of the duct, noting that only 36 per cent of the cadavers studied had a single trunk with one opening into the venous system. Single trunks with multiple openings were seen in a further 16 per cent of cases, whilst the remaining cadavers had either multiple trunks or a lymphatic plexus with one or more openings. This variation may be found in both right and left terminating ducts.Reference Davis4, Reference Lane and Todd17
LaneReference Lane and Todd17 noted the frequency of termination of the thoracic duct on the right, and provided one of the earliest classification systems for this phenomenon, as follows: type I, double thoracic ducts terminating bilaterally at their corresponding venous angle; type II, bifurcation of the duct at any level with the branches terminating at their corresponding venous angle, or with the right-sided branch ending in the right lymphatic duct; and type III, a single duct terminating at the right venous angle, with an absent left duct. In the case of a type III duct, an equivalent structure to the right lymphatic trunk is usually found on the left, though this may be absent, implying that all lymphatic fluid is drained via the right duct.Reference Watson12 The reported variations of lymphatic connections from the ‘standard’ adult pattern are demonstrated in Figure 2. The prevalence of the thoracic duct terminating on the right is difficult to estimate. Dissection studies describing right-sided termination (summarised in Table I) suggest a prevalence of between 1 and 5 per cent. However, the true figure is unclear as some studies of the thoracic duct only document left-sided termination, including the largest published study (which included 1081 cadavers).Reference Van Pernis20

Fig. 2 Diagram summarising previously reported anatomical variations of the thoracic ducts. R = right; L = left
Table I Previous anatomical studies describing right-sided termination of thoracic duct

RTD = right thoracic duct prevalence
Variation also occurs at the point of entry of the thoracic duct to the venous system. Most frequently, the duct ends in the left internal jugular vein, or in the left venous angle between the internal jugular and subclavian veins, having received the cervical lymph trunks (jugular, bronchomediastinal and subclavian). Less commonly, it terminates in the subclavian vein, or in combinations of veins via multiple branches, and the cervical lymphatic trunks may enter the venous system separately.Reference Davis4, Reference Lane and Todd17, Reference Kinnaert21 The termination of the thoracic duct on the right is less well described due to its lower incidence, but similar variation has been seen in cadavers. As well as single duct termination in the right venous angleReference van der Putte and van Limborgh5 or internal jugular vein,Reference Watson12, Reference Peña and Zuñiga22 branching and multiple terminations occur (Figure 3).Reference Davis4, Reference Crumley and Smith15 The lympho-venous junction is usually within 15 mm of the venous angle,Reference Kinnaert21 though more distant termination in the brachiocephalic and left transverse cervical vein is also reported.Reference Skandalakis, Skandalakis and Skandalakis1, Reference Jacobsson16, Reference Kinnaert21

Fig. 3 Diagrams showing previously reported right-sided terminations of the thoracic duct (light green) and right lymphatic duct (dark green) with the venous system (blue): (a) DavisReference Davis4; (b) Chen et al. Reference Chen, Shoumura and Emura11 and Nathan and GitlinReference Nathan and Gitlin13 (without mention of the right lymphatic duct); (c) Peña and ZuñigaReference Peña and Zuñiga22 and WatsonReference Watson12; and (d) Watson.Reference Watson12
Valves are more common in the cervical part of the duct, with a bicuspid valve or tissue fold often present at the venous junction to prevent reflux of blood.Reference Jacobsson16, Reference Shimada and Sato23 A dilated ampulla is also frequently found near the termination of the duct, often associated with lower cervical lymph nodes,Reference Kinnaert21 a feature that may potentially increase the risk of intra-operative injury. There is equal sex distribution in variations of the course of the thoracic duct, and no familial tendency.Reference Skandalakis, Skandalakis and Skandalakis1 Racial differences may however occur, with Kihara and AdachiReference Kihara and Adachi6 reporting thoracic duct termination at the jugulosubclavian angle in 78.2 per cent of Japanese subjects but only 33 per cent of Caucasian subjects.
The termination of the thoracic duct has relevance to surgeons aside from the risk of intra-operative injury, as some authorsReference Shimada and Sato23, Reference Byers24 report that multiple and complex terminations of the thoracic duct are associated with a higher risk of metastasis during mediastinal and cervical lymph node dissection.
Surgical significance
The thoracic duct is at risk in any surgery of the lower neck. The risk of injury is significantly greater during dissection of the lower cervical nodes, in particular the retrojugular region – a crucial area for clearance which is frequently a site of metastasis in papillary thyroid carcinoma cases. The highly variable anatomy and thin, translucent walls ensure that identification of the major lymphatics is difficult and injury common. As predicted by the potential for connections between the thoracic duct and right lymphatic duct, right-sided chyle leaks have been reported.
The incidence of chyle leakage on either side after neck dissection is usually estimated to be 1 to 2.5 per cent,Reference Crumley and Smith15 although a rate of 8.3 per cent was found in one prospective study of lateral neck dissections.Reference Roh, Kim and Park25 Large studies quote very variable figures for the prevalence of chyle leakage after right-sided neck dissections, from 0 per cent to a prevalence nearly matching that on the left.Reference Roh, Kim and Park25 These figures are perhaps surprising when compared with the prevalence of right-sided thoracic duct termination, and suggest that this anatomical abnormality is at high risk of injury when present. Whilst neck dissection is the most common cause of right-sided cervical chyle leakage, it can also occur during other surgery, most frequently that involving the thyroid gland.Reference Priego Jiménez, Collado Guirao, Rojo Blanco, Grajal Marino, Rodríguez Velasco and García Villanueva26
In a large review, Santaolalla et al. Reference Santaolalla, Anta, Zabala, Del Rey Sanchez, Martinez and Sanchez27 concluded that: (1) chylous collections and fistulae were significantly more common in radical versus functional dissections; (2) radiotherapy prior to surgery was a risk factor; and (3) there was no correlation between duct injury and tumour stage. Interestingly, in this series of over 300 cases, no right-sided chyle leaks were seen. Chyle fistulae and collections greatly contribute to patient morbidity and also significantly increase the length of hospital stay.Reference Santaolalla, Anta, Zabala, Del Rey Sanchez, Martinez and Sanchez27
Chyle leakage may be suspected clinically based on high drainage volumes and a characteristic thin and cloudy or milky appearance. Its identity is confirmed by laboratory demonstration of a cholesterol/triglyceride ratio of less than 1.Reference Halldorsson28 If a chyle leak has occurred, the comparison of both triglyceride and cholesterol levels in serum versus drainage fluid on post-operative day one usually demonstrates significantly raised levels in drainage fluid, enabling an objective and early diagnosis.Reference Erisen, Coskun and Basut29
Conclusion
It is evident that difficulty in identifying the thoracic duct during neck dissection and other cervical surgery may lead to the formation of chyle collections and fistulae. This problem is exacerbated by a lack of appreciation of the significant variability in duct anatomy, in particular the possibility of a right-sided thoracic duct draining the lower part of the body, with multiple cervical interconnections.
We therefore advise that care be taken to avoid duct injury when performing neck dissection on either side, with particular attention when clearing level IV or V nodes, or if vascular abnormalities are present. While it is wise to be vigilant regarding the thoracic duct, intra-operative dissection to locate the duct is not recommended as the risk of iatrogenic injury is high.Reference Nussenbaum, Liu and Sinard30
It is noteworthy that enlarged right supraclavicular nodes may herald not only cervical or thoracic malignancies but also those of intra-abdominal origin.






