Introduction
The treatment approach for laryngeal cancer has been firmly established, and a five-year survival rate of more than 70 per cent is expected even for patients with advanced cancer.Reference Mori, Mihoki, Nakashima, Hirano, Kojima and Hayabuchi1–Reference Miyahara, Yane, Tsuruta and Uemura3 However, in laryngeal cancer cases, cervical lymph node metastasis and distant metastasis are more frequently observed in patients with supraglottic than glottic carcinomas, and the former diagnosis is considered to lower patients' treatment prognosis. A clinical research trial was therefore undertaken to review the available therapeutic methods, by assessing treatment results in patients with supraglottic carcinoma treated at Kurume University Hospital.
Subjects and methods
This study enrolled 161 patients with supraglottic squamous cell carcinoma who underwent radical therapy at the Kurume University Hospital department of otolaryngology beween January 1989 and December 2003. The study group comprised 144 men and 17 women, with a ges ranging between 41 and 95 years (mean: 66 years). Table I shows the tumour–node (TN) staging system and stage grading for the patients' tumours. Many patients had advanced cancer of stage III or IV.
Table I Tumour–node classification

Data represent number of patients.
The basic therapeutic policy for supraglottic carcinoma at our centre is chemo-radiotherapy for cases graded T1 or T2. Chemo-radiotherapy alone is administered for superficial tumours. In the case of larger, more invasive tumours, the tumour volume is reduced as much as possible by CO2 laser therapy prior to chemo-radiotherapy. A cervical lymph node dissection is performed for patients with cervical lymph node metastasis. A partial resection or laryngectomy is performed for patients with grade T3 disease, and laryngectomy is performed for patients with grade T4 disease. Bilateral cervical lymph node dissections are performed for grade T3 and T4 cases. Post-surgical irradiation is performed for patients with grade T4 disease and severe cartilage destruction, and for patients with lymph node metastasis accompanied by pathological extracapsular infiltration.
Based on the therapeutic policy described above, the patients' survival rates were calculated according to their T stage, N stage and overall disease stage. In addition, for patients undergoing conservative therapy of the larynx, local control rates and laryngeal preservation rates were calculated according to patients' T stage, lesion site and therapeutic method. Causes of death were analysed according to the patient's disease stage.
The survival rate, calculated using the Kaplan–Meier method, was determined as the survival rate by cause of death. The log-rank test was used for testing significant differences, and the chi-square test was used for comparisons between groups.
Results
Figure 1 shows survival rates according to patients' T stage. The five-year survival rate was favourable; even patients staged T4 had a five-year survival rate of 71 per cent.

Fig. 1 Patient survival rates by tumour (T) stage (n = 161).
Patient survival rates by N stage are shown in Figure 2. Patients staged N2 had the lowest five-year survival rate, at 66 per cent. None of the patients with N3 disease survived beyond five years.

Fig. 2 Patient survival rates by node (N) stage (n = 161).
Figure 3 shows patient survival rates according to their disease stage. The five-year survival rate was 89 per cent for patients with stage III disease and 75 per cent for stage IV disease, thus demonstrating favourable results even for patients with advanced cancer.

Fig. 3 Patient survival rates by disease stage (n = 161).
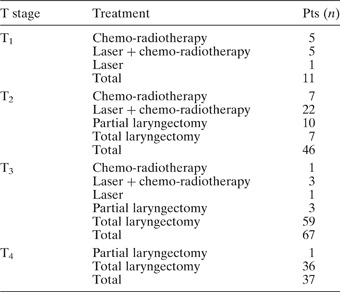
Table II shows the initial therapeutic method according to patients' T stage. Laser therapy was used concomitantly in many of the patients staged T1 and T2, for whom laryngeal preservation therapy was undertaken. Table III shows the local control rates and laryngeal preservation rates according to patients' T stage. The five-year local control rate and the laryngeal preservation rate were poor in patients graded T3 (being 75 per cent for both), but the overall five-year local control rates were 86 per cent.
Table II Initial therapeutic method by tumour stage

Pts = patients; T = tumour
Table III Local control and laryngeal preservation rates according to T stage

T = tumour; pts = patients; yr = year
Table IV shows local control rates and laryngeal preservation rates according to the therapeutic method used. Laser surgery plus chemo-radiotherapy was the most frequently used therapy (n = 30) and gave the best local control rates and laryngeal preservation rates, except for the two patients treated with laser therapy alone.
Table IV Local control and laryngeal preservation rates by therapeutic method

Pts = patients; yr = year; RT = radiotherapy; ptl = partial
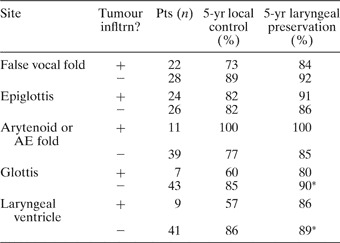
Table V shows the local control rate and laryngeal preservation rate according to the site of the lesion. These rates were compared according to the presence or absence of tumour infiltration at each subsite. Local control rates and laryngeal preservation rates were statistically significantly worse in patients with tumour infiltration of the glottis and the laryngeal ventricle.
Table V Local control and laryngeal preservation rates by lesion site
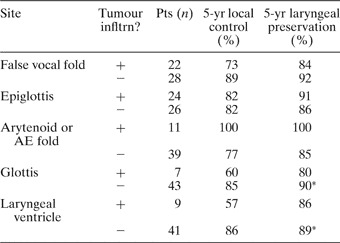
Note that tumour infiltrated more than one site in some patients. *p = 0.04, comparing both values. Infltrn = infiltration; pts = patients; yr = year; AE = aryepiglottic
Table VI shows the cause of death by disease stage. Of the patients who died due to the primary disease, death due to distant metastasis was the most common cause (15 patients), followed by death due to the primary foci (four patients) and death due to lymph node metastasis (one patient). Death due to other disease was the most frequent cause of death in the total patient group.
Table VI Cause of death by disease stage

Pts = patients; mets = metastasis
Discussion and conclusions
Although laryngeal cancer is a malignant tumour and the most common of the head and neck cancers, the therapeutic approach is firmly established and treatment results have improved over time.Reference Mori, Mihoki, Nakashima, Hirano, Kojima and Hayabuchi1 However, cervical lymph node metastasis and distant metastasis are still relatively common in patients with supraglottic laryngeal cancer; therefore, the therapeutic methods for this cancer need further improvement.Reference Chijiwa, Mori, Umeno and Nakashima4
The comprehensive multidisciplinary head and neck cancer team at Kurume University Hospital was established in 1989,Reference Mori, Mihoki, Nakashima, Hirano, Kojima and Hayabuchi1, Reference Hirano5 and enables active cooperation between radiotherapy specialists and clinical oncologists. The participation of radiotherapy specialists in discussions before and after treatment facilitates a more comprehensive judgment regarding diagnosis and therapeutic policy, thereby enabling better patient treatment.
Our multidisciplinary team's therapeutic policy and consequent results for supraglottic carcinoma are discussed below. Recently, radiotherapy has been the first-line treatment in our centre for patients with localised early cancer. However, early cancer may be either superficial or more invasive. With respect to tumour volume, Dubben et al. Reference Dubben, Thames and Beck-Bohnholdt6 and Benzen and ThamesReference Benzen and Thames7 reported a poor prognosis in patients with a large tumour volume. Their conclusions are consistent with our department's policy, whereby, for large tumours, radiotherapy is administered after the tumour volume is reduced as much as possible by laser therapy. The usefulness and efficacy of laser therapy have been proven at this department based on extensive experience with various head and neck cancers since the 1980s.Reference Mihashi8–Reference Mori12
The results of the current study showed a favourable laryngeal preservation rate of 91 per cent following volume reduction by laser therapy plus chemo-radiotherapy. No statistically significant difference was observed in comparison with other therapies, but combination laser therapy is considered to be a useful method (in comparison with chemo-radiotherapy alone) in patients with large tumour volumes. The indications for combination laser therapy should therefore be extended in the future.
The survival rate for supraglottic carcinoma becomes poorer as the tumour stage deteriorates; nevertheless, it was 89 per cent for stage III and 75 per cent for stage IV disease, indicating favourable results even in patients with advanced cancer. Analysis of the cause of death showed that four patients died of the primary foci and one died of lymph node metastasis. The results were favourable for the localised cervical site. One of the reasons for fewer deaths due to lymph node metastasis may be our basic policy of performing bilateral cervical lymph node dissection. However, patients who undergo cervical lymph node dissection often complain of stiff shoulders or tightness of the neck, and it cannot be denied that these patients' quality of life is reduced.
Further study will be conducted to determine which supraglottic carcinoma patients should undergo cervical lymph node dissection, especially on the non-lesion side, rather than performing it in all patients with localised advanced cancer. The high mortality due to distant metastasis is also an unresolved issue. The best type and method of chemotherapy for different patients, and the optimum type and number of courses of chemotherapy, should also be further clarified.