Introduction
Superior semicircular canal dehiscence is an uncommon neurotological disorder in which the petrous temporal bone overlying the superior semicircular canal lacks bone.Reference Ward, Carey and Minor1 Initially identified in 1998 by Minor et al., superior semicircular canal dehiscence is characterised by an abnormal communication between the middle fossa and the superior semicircular canal, resulting in altered vestibular and auditory function.Reference Minor, Solomon, Zinreich and Zee2 The most common symptoms of superior semicircular canal dehiscence include amplification of internal sounds, autophony, tinnitus, sound- and pressure-induced vertigo, hyperacusis, oscillopsia, and hearing loss.Reference Ward, Carey and Minor1,Reference Minor, Solomon, Zinreich and Zee2 Clinical symptoms, suprathreshold bone conduction and vestibular-evoked myogenic potential testing are valuable in superior semicircular canal dehiscence diagnosis, but the ‘gold standard’ method of detection is high-resolution computed tomography (CT) of the petrous temporal bones, preferably using special positioning.Reference Zuniga, Janky, Nguyen, Welgampola and Carey3,Reference Sequeira, Whiting, Shimony, Vo and Hullar4
Treatment of superior semicircular canal dehiscence is divided into two approaches: medical and surgical. The transmastoid approach and the middle fossa repair are surgical options for treating superior semicircular canal dehiscence.Reference Johanis, Yang and Gopen5 This paper demonstrates the repair of superior semicircular canal dehiscence with small middle fossa craniotomy using an oto-microscopic and co-endoscopic assisted approach.
Materials and methods
The study protocol was approved by the local ethics committee of Bezmialem Vakif University, and all patients provided informed consent. Eleven patients with hearing loss, vertigo, aural fullness, pulsatile tinnitus, hyperacusis and autophony symptoms were enrolled in this study.
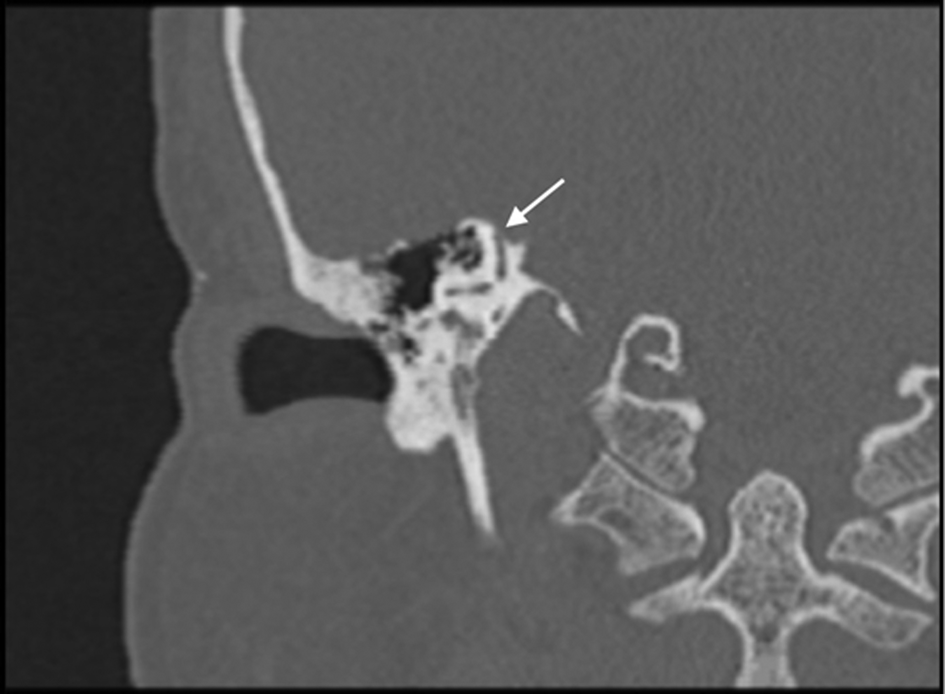
Superior semicircular canal dehiscence diagnoses were verified on the bases of temporal CT in the Pöschl position (Figure 1), pure tone audiograms and cervical vestibular-evoked myogenic potential testing. Nine patients had complaints of aural fullness, pulsatile tinnitus, hyperacusis and autophony. All patients had pure tone audiometry results indicating supranormal bone conduction threshold and conductive hearing loss (Figure 2). Cervical vestibular-evoked myogenic potential findings showed decreased thresholds. Post-operative supranormal bone conduction thresholds were observed to be within normal limits (Figure 3). These findings allowed us to diagnose superior semicircular canal dehiscence in these patients.

Fig. 1. Pre-operative temporal computed tomography image in the Pöschl position, showing dehiscence of the superior semicircular canal (arrow).

Fig. 2. Pre-operative audiogram. > = bone conduction – unmasked, mastoid (left); < = bone conduction – unmasked, mastoid (right); ] = bone conduction – masked, mastoid (left); [ = bone conduction – masked, mastoid (right); × = air conduction – unmasked (left); ○ = air conduction – unmasked (right); BC = bone conduction; EML = effective masking level; R = right; L = left

Fig. 3. Post-operative fourth-month audiogram. > = bone conduction – unmasked, mastoid (left); < = bone conduction – unmasked, mastoid (right); ] = bone conduction – masked, mastoid (left); [ = bone conduction – masked, mastoid (right); × = air conduction – unmasked (left); ○ = air conduction – unmasked (right); BC = bone conduction; EML = effective masking level; R = right; L = left
An endoscopy-assisted middle fossa approach was applied to all patients. In the first post-operative week, we took a photograph of the scar of the approximately 6 cm, S-shaped incision over the temporal scalp (Figure 4). Then, a craniotomy of 3 × 3 cm was performed. After the middle fossa retractor was placed, the defect site was detected by endoscopy. Plugging with bone wax and perichondrium was used to close the defect. After the operation was completed successfully, patients were kept in the hospital for 1 day.

Fig. 4. Photograph of the scar at the first week post-operatively.
On the 1st post-operative day, all patients had regression of autophony, hyperacusis and aural fullness. There was no significant difference in pure tone audiometry and cervical vestibular-evoked myogenic potential tests performed in the first post-operative month compared to pre-operative findings.
Results
The superior semicircular canal dehiscence of 11 patients was successfully repaired and observed through the facilitation of a 45-degree endoscope. This is demonstrated in a short video, available on The Journal of Laryngology & Otology website (Appendix 1).
All patients’ complaints disappeared compared with pre-operative symptoms, and there were no complications. The average follow-up duration was 2 years, with an observation period of at least 18 months and a maximum of 42 months. In a case series of 11 patients with superior semicircular canal dehiscence treated surgically with the endoscopically assisted middle fossa approach, we did not observe any epilepsy case following temporal lobe retraction during an average of two years of follow up. It was observed that supranormal bone conduction thresholds (Figure 3) and cervical vestibular-evoked myogenic potential results reached normal limits in the fourth post-operative month.
Discussion
Superior semicircular canal dehiscence is an uncommon neurotological disorder in which the petrous temporal bone overlying the superior semicircular canal lacks bone.Reference Ward, Carey and Minor1 The most common symptoms of superior semicircular canal dehiscence include amplification of internal sounds, autophony, tinnitus, sound- and pressure-induced vertigo, hyperacusis, oscillopsia, and hearing loss.Reference Johanis, Yang and Gopen5
Surgical repair is the only viable option in patients with incapacitating symptoms. Traditionally, superior semicircular canal dehiscence repair has been achieved using a middle fossa craniotomy approach. However, approximately 30 per cent of superior semicircular canal dehiscence cases have a medial arcuate eminence defect along a down-sloping tegmen. In such cases, the defect is difficult to visualise with the binocular surgical oto-microscope without a large craniotomy, extensive temporal lobe retraction and drilling of the skull base.
As complete visualisation of an arcuate eminence defect is essential for successful repair, we use small middle fossa craniotomy and rigid endoscopy. The wide-field view and superior transillumination with skull base endoscopy can be achieved with a minimal-access skin incision, small bony window, less dural dissection and reduced brain retraction. As in our video (Appendix 1), all patients were operated on using a middle fossa approach, with a smaller bony window and a 45-degree rigid endoscope. All patients’ complaints disappeared compared with pre-operative symptoms; furthermore, no post-operative complications developed.
We conducted this investigation as a pilot study of 11 patients. We are planning a larger study of superior semicircular canal dehiscence cases in which we will compare the endoscopically assisted middle fossa approach with the traditional binocular craniotomy or transmastoid approach. We chose to perform superior semicircular canal dehiscence surgery using the endoscopically assisted middle fossa approach because this technique involves a smaller incision, smaller craniotomy and, consequently, a shorter hospital stay.
Conclusion
This case–control study, with a level of evidence of 4, indicated that oto-microscopic and co-endoscopic assisted repair of superior semicircular canal dehiscence may be an alternative and superior approach to the oto-microscopic approach alone. The oto-microscopic and co-endoscopic approach may be used for visualisation of the entire arcuate eminence defect, regardless of the bony skull base topography.
Competing interests
None declared
Appendix 1. Supplementary video material
A short video demonstrating endoscopic-assisted repair of superior semicircular canal dehiscence with middle fossa craniotomy is available online at The Journal of Laryngology & Otology website, at https://drive.google.com/file/d/1kCdMayC77uCKUFyMW4ECgWR0uR7hTu7d/view?usp=sharing.